Notes on pulmonary causes
advertisement
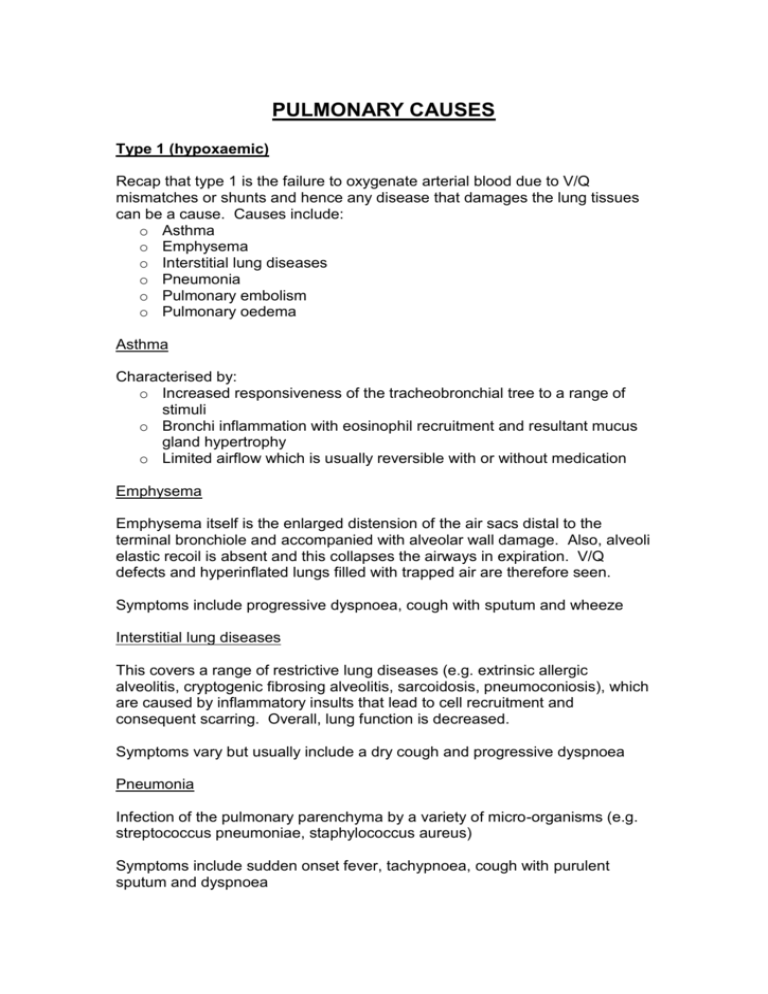
PULMONARY CAUSES Type 1 (hypoxaemic) Recap that type 1 is the failure to oxygenate arterial blood due to V/Q mismatches or shunts and hence any disease that damages the lung tissues can be a cause. Causes include: o Asthma o Emphysema o Interstitial lung diseases o Pneumonia o Pulmonary embolism o Pulmonary oedema Asthma Characterised by: o Increased responsiveness of the tracheobronchial tree to a range of stimuli o Bronchi inflammation with eosinophil recruitment and resultant mucus gland hypertrophy o Limited airflow which is usually reversible with or without medication Emphysema Emphysema itself is the enlarged distension of the air sacs distal to the terminal bronchiole and accompanied with alveolar wall damage. Also, alveoli elastic recoil is absent and this collapses the airways in expiration. V/Q defects and hyperinflated lungs filled with trapped air are therefore seen. Symptoms include progressive dyspnoea, cough with sputum and wheeze Interstitial lung diseases This covers a range of restrictive lung diseases (e.g. extrinsic allergic alveolitis, cryptogenic fibrosing alveolitis, sarcoidosis, pneumoconiosis), which are caused by inflammatory insults that lead to cell recruitment and consequent scarring. Overall, lung function is decreased. Symptoms vary but usually include a dry cough and progressive dyspnoea Pneumonia Infection of the pulmonary parenchyma by a variety of micro-organisms (e.g. streptococcus pneumoniae, staphylococcus aureus) Symptoms include sudden onset fever, tachypnoea, cough with purulent sputum and dyspnoea Pulmonary embolism The obstruction of the pulmonary arteries from a thrombus in the venous circulation (e.g. from DVT) Symptoms include sudden onset dyspnoea, pleuritic chest pain, haemoptysis, and syncope Pulmonary oedema The accumulation of excessive fluid in the air spaces of the lungs. Generalised pulmonary oedema only occurs in ARDS (adult respiratory distress syndrome) and factors that disturb the Starling equilibrium such as left ventricular failure, renal failure (volume overload) and liver failure (hypoalbuminaemia). Type 2 (hypercapnic) Recap type 2 is due to alveolar hypoventilation and the consequent build up of CO2. Causes include: o Chest wall defects o Respiratory muscle weakness o Reduced respiratory centre drive o Severe pulmonary disease Chest wall defects These include flail chest and kyphoscoliosis Flail chest is due to trauma causing fracture of three or more ribs in at least two areas. The flail piece moves paradoxically during inspiration and expiration and therefore alters the normal movement of the ventilation apparatus to induce RF. Kyphoscoliosis is the posterolateral curvature of the spine that can be congenital or affected by diseases of the vertebrae and surrounding muscles. This curvature of the spine may eventually cause restrictive ventilatory failure because total lung volumes, FEV1 and FVC are all reduced, and the work of breathing is increased to try to ventilate the lungs. Respiratory muscle weakness These can affect the muscles of inspiration and active expiration. Can occur with: o Myasthenia gravis o Muscular dystrophy or May be a result of neurological diseases: o Phrenic nerve paralysis o Lesions in the cervical spine o Guillain-Barré syndrome Reduced respiratory centre drive Causes include: o Drugs that act as a sedative such as opiates o Trauma to the brainstem Severe pulmonary disease These include COPD, asthma, pulmonary fibrosis, and pneumonia, which can induce either type 1 or type 2 patterns of RF, and not affect the ventilatory apparatus. If these induce type 2 then it suggests ventilation is completely inadequate to compensate for the hypoxaemia and implicates most, if not all, the lung is damaged. Severe chronic obstructive pulmonary disease (COPD) is the most common cause of type 2 RF. COPD A progressive disorder where there is an increased resistance to airflow with limited reversibility FEV1 <80% and FEV1:FVC ratio <70% Cigarette smoking is the main aetiological factor Two diseases comprise COPD: emphysema (previously mentioned) and chronic bronchitis Chronic bronchitis is defined clinically as cough with sputum for at least 3 months in 2 successive years. Pathologically, it consists of hypertrophic mucus secreting glands in cartilaginous airways, and inflammatory cells and intraluminal mucus plugs in smaller airways. All these contribute to a significant obstruction to the airflow. There are two groups of patients that present with COPD but these are NOT strictly distinct from each other - it just makes understanding easier: Pink puffers Blue bloaters Typical Thin and not cyanosed Overweight and cyanosed Appearance (central and peripheral) Clinical Dyspnoea +/- cough Cough with sputum, symptoms exacerbated by infections Blood gases PaO2 : low PaO2 : low (ABGs) PaCO2 : low or normal PaCO2 : high Physiology Attempts to maintain normal Fails to increase respiratory ABGs by increasing the effort effort thus CO2 levels rise to for respiration drive respiration Predominate Emphysema Chronic bronchitis disease Respiratory Failure Typically type 1 Typically type 2 In the long-term, the COPD of ‘blue bloaters’ become severe in that they depend upon hypoxaemic levels of oxygen to stimulate ventilation, and the normal CO2 drive is loss. This makes oxygen therapy for their type 2 RF limited, as too much O2 would cause their respiratory drive to shut down. Be aware that although the paragraph above is usually taught in clinical medicine, there is actually little experimental evidence to support the dependency on hypoxic drive and there are alternative factors that may contribute, e.g. administration of oxygen may result in hypoxic vasoconstriction such that the V/Q mismatch worsens and results in hypercapnia.