Corticosteroids
advertisement

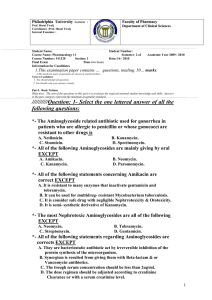
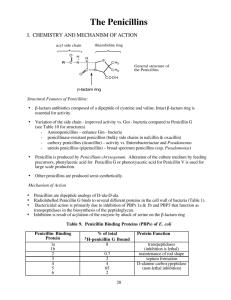
KINE 3330 Pathology and Pharmacology Spring 2005 Study Guide – Test #1 The test will be made up of multiple-choice, short answer, and critical thinking questions. Test questions will be taken from class notes, power points, class discussions, and chapter reading assignments (Chapters 1-6, 10, and 13) YOU WILL BE ALLOWED TO USE YOUR NOTEBOOK FOR TEN (10) MINUTES DURING THE EXAM. TO MAXIMIZE THESE 10 MINUTES, YOU SHOULD HAVE YOUR NOTEBOOK VERY ORGANIZED. CONTENT TO BE COVERED ON EXAM: Chapter 1 Intro to Pharmacology drug nomenclature drug names (i.e., chemical, generic, trade) drug classification (OTC, prescription drugs, controlled substances) pharmacodynamics vs. pharmacokinetics role of FDA in drug development and approval FDA new approval process drug recalls drug info sources (PDR, Drug Facts & Comparisons, etc.) Chapter 2 Pharmacokinetic Principles ADME process of pharmacokinetics & the effect of exercise on each phase half-life bioavailability bioequivalence volume of distribution fat soluble vs. water soluble routes of drug administration and their effect on absorption passive diffusion vs. active transport Chapter 3 Pharmacodynamic Principles Receptor theory of drug interaction drug interactions and adverse reactions additive, synergistic, antagonistic, placebo drug dosing & potency maintenance dose vs. loading dose Chapter 4 Medication Management in Athletic Training Facilities (covered in lab by Sarah Marek) Policies and Procedures for storing medications Disposal of expired medications Security & storage DEA requirements Record keeping including signatures Repackaging of medications Chapter 5 Drugs for Treating Infections causes of antibiotic resistance narrow spectrum vs. broad spectrum what factors should be considered when selecting an antibiotic upper respiratory infections (bacterial) vs. lower respiratory infections (viral) antibiotics (be able to identify the more commonly used drugs in this category) antibacterials general adverse effects: nausea, vomiting, loss of appetite, penicillins (bactericidal) most common: ampicillin. amoxicillin, amoxil, augmentin drug-drug interactions cause allergic reactions in up to 10% of patients primary uses: urinary tract infections, respiratory tract infections, infections of the heart, syphilis cephalosporins (bactericidal) common: Ceclor, Rocephin, Keflex primary uses: respiratory tract infections, urinary tract infections, skin infections cause fewer allergic reactions than penicillins tetracyclines broad spectrum use of these antibiotics have declined due to increase in bacterial resistance often becomes the drug of choice for patients who are allergic to other penicillins or cephalosprorins primary uses: Rocky Mountain spotted fever, Lyme disease, pneumonia, acne, ulcers caused by H. pylori vibramycin (doxycycline) – one of most common macrolides (bacteriostatic) drug of choice for patients allergic to penicillins & cephalosporins common: Zithromax, E-Mycin (erythromycin) primary uses: infections of the GI, genitals, & respiratory tract antifungals tinea pedis (athlete’s foot) & tinea cruris (jock itch) treated with OTC meds tinea unguium – nail fungus treated with oral antifungals (Lamisil solution or Lamisil tablets) tinea versicolor can be treated with oral or topical antifungal (1-2 weeks) vaginal candidiasis (yeast infection) can be treated orally (Diflucan) or topically oral candidiasis (thrush) treated with topical agents (1-2 weeks) general antifungal side effects fever, chills, rash, itching, nausea antivirals usually very expensive acyclovir (Zovirax) [oral] & Penciclovir (Denavir) [topical] used to treat fever blisters amantadine (Symmetrel) & Rimentadine (Flumadine) – used to prevent or lessen the severity of the flu (influenza A strain) zanamivir (Relenza) – used to prevent or lessen the severity of the flu (influenza A & B strains) Chapter 6 Drugs for Treating Inflammation NAIDs physiology of inflammation NSAID effects role of prostaglandins COX -1 and COX-2 pathways difference between COX-2 selective NSAIDs and COX nonselective NSAIDs (be able to list 2-3 examples of each) adverse effects of NSAIDs cautions associated with the use of NSAIDs drug interactions Corticosteroids chemical make-up: lipid soluble hormone general indications routes of administration side effects & adverse reactions (generally and by route of administration) Chapter 10 Drugs for Treating Cold and Allergies cough, cold & allergy products (be able to identify the more commonly used meds in each of the categories, indications for the drugs, mechanisms of action, & common side effects) antihistamines Allegra, Benadryl (dyphenhydramine) Clarinex, Claritin (causes less drowsiness than dyphenhydramine), Zyrtec, Singular Decongestants Allegra D, Nasonex, Zyrtec D, Sudafed (pseudoephedrine) expectorants mucolytics guaifenesin zinc Chapter 13 Performance-Enhancing Drugs Physiological effects (theory for using these drugs), side effects, pharmacodynamics, etc. androgenic-anabolic steroids human growth hormone erythropoietin