Intensive Care Nursery
advertisement
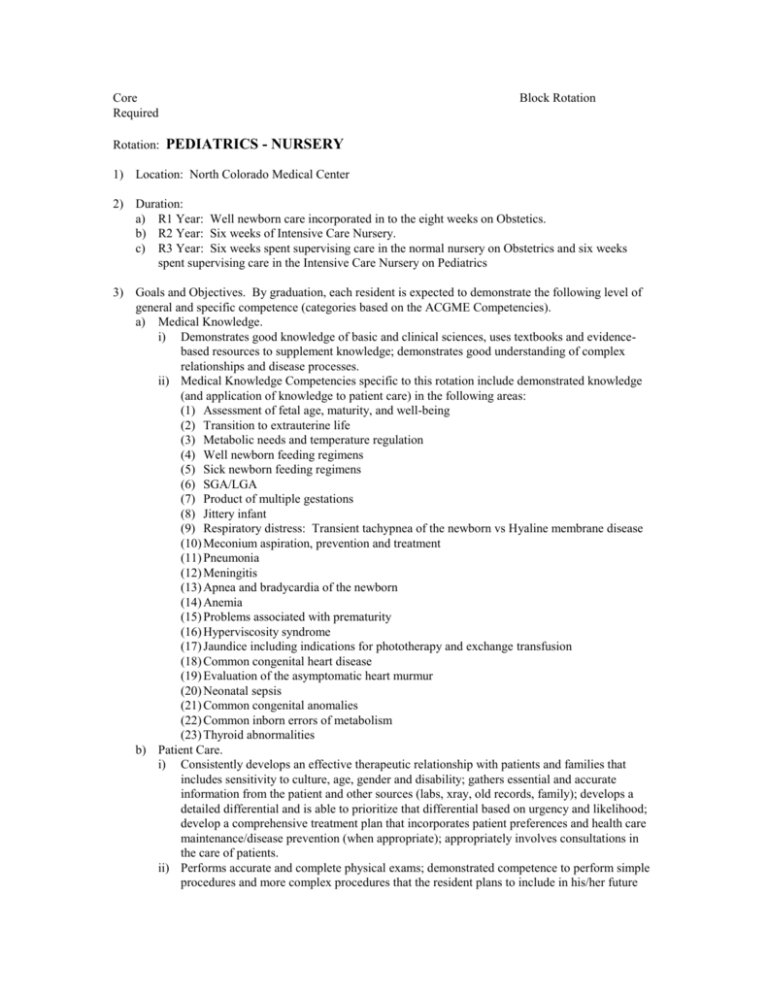
Core Required Rotation: Block Rotation PEDIATRICS - NURSERY 1) Location: North Colorado Medical Center 2) Duration: a) R1 Year: Well newborn care incorporated in to the eight weeks on Obstetics. b) R2 Year: Six weeks of Intensive Care Nursery. c) R3 Year: Six weeks spent supervising care in the normal nursery on Obstetrics and six weeks spent supervising care in the Intensive Care Nursery on Pediatrics 3) Goals and Objectives. By graduation, each resident is expected to demonstrate the following level of general and specific competence (categories based on the ACGME Competencies). a) Medical Knowledge. i) Demonstrates good knowledge of basic and clinical sciences, uses textbooks and evidencebased resources to supplement knowledge; demonstrates good understanding of complex relationships and disease processes. ii) Medical Knowledge Competencies specific to this rotation include demonstrated knowledge (and application of knowledge to patient care) in the following areas: (1) Assessment of fetal age, maturity, and well-being (2) Transition to extrauterine life (3) Metabolic needs and temperature regulation (4) Well newborn feeding regimens (5) Sick newborn feeding regimens (6) SGA/LGA (7) Product of multiple gestations (8) Jittery infant (9) Respiratory distress: Transient tachypnea of the newborn vs Hyaline membrane disease (10) Meconium aspiration, prevention and treatment (11) Pneumonia (12) Meningitis (13) Apnea and bradycardia of the newborn (14) Anemia (15) Problems associated with prematurity (16) Hyperviscosity syndrome (17) Jaundice including indications for phototherapy and exchange transfusion (18) Common congenital heart disease (19) Evaluation of the asymptomatic heart murmur (20) Neonatal sepsis (21) Common congenital anomalies (22) Common inborn errors of metabolism (23) Thyroid abnormalities b) Patient Care. i) Consistently develops an effective therapeutic relationship with patients and families that includes sensitivity to culture, age, gender and disability; gathers essential and accurate information from the patient and other sources (labs, xray, old records, family); develops a detailed differential and is able to prioritize that differential based on urgency and likelihood; develop a comprehensive treatment plan that incorporates patient preferences and health care maintenance/disease prevention (when appropriate); appropriately involves consultations in the care of patients. ii) Performs accurate and complete physical exams; demonstrated competence to perform simple procedures and more complex procedures that the resident plans to include in his/her future practice (including knowledge of indications, contra-indications, appropriate consent, complications (and how to address them), and follow up). iii) Patient Care competencies specific to this rotation include: (1) Resuscitation of the newborn (2) Stabilization of the newborn (3) Uncomplicated transport of the newborn (4) Newborn physical examination (5) Circumcision (6) Venipuncture (7) Peripheral arterial puncture for blood gas sampling and interpretation of ABG (8) Lumbar puncture (9) Orotracheal intubation (10) Peripheral IV insertion (11) UVC and UAC placement c) Practice-Based Learning and Improvement. i) Investigates and evaluates his/her own patient care, appraises and assimilates scientific evidence, and uses this information to work toward improvements in patient care. ii) Practice-Based Learning and Improvement activities specific to this rotation includes presentation of didactic topics to the OB/Peds rounding team: (1) Three times during the R1 year. (2) Four times during the R2 year. (3) Sixteen to twenty times during the R3 year. d) Interpersonal and Communication Skills. i) Written documentation/communication is legible, timed and dated, complete (but with appropriate conciseness), accurate and using appropriate language and abbreviations. Verbal communication with patients, families, and members of the healthcare team are respectful and effective (including effective presentation skills). Keeps supervising physicians up to date on patients. ii) Interpersonal and communication competency specific to this rotation include: (1) Addressing parental concerns and questions (2) Assessment and promotion of bonding e) Professionalism. Consistently on-time, works hard, able to identify required tasks and complete them in a timely and efficient manner; team-oriented and willing to assist with work load as needed to optimize team function; able to identify need for help and request it; demonstrates a positive attitude and interactions with team members; adheres to ethical principles in the course of his/her practice; identifies and progresses toward personal educational goals; is receptive to, seeks, and incorporates feedback. f) Systems-Based Practice. i) Demonstrates an awareness of the larger healthcare system, assists patients in dealing with system complexities through the effective use of hospital and community resources; participates in some system improvement through identification of errors and system problems and initial discussion of potential system improvements; acts as an effective teacher of junior residents and other members of the healthcare team. ii) Systems-Based Practice competencies specific to this rotation include: (1) Demonstration of appropriate skills in referral and consultation of pediatric specialists for more complex nursery problems. (2) Utilization of and coordination with hospital and community resources such as physical/occupation/respiratory therapists, breast feeding specialists, social workers, WIC, and Child Protective Services. 4) Methods: a) During the two four week Obstetrics rotations in the R1 year, the resident is responsible for the care of all well newborns of unassigned, NCFM, Weld County Health Department, Sunrise Community Health Center and Monfort Children’s Clinic patients. The resident is under the direction of the third year resident and the attending staff. b) The second year resident on Intensive Care Nursery (one six week block) is responsible for all patients admitted to the neonatal intensive care unit, and follows these patients in conjunction with the family medicine and pediatrics attending staff, and working closely with the staff NNP’s. While taking Obstetrics call, the R2 is also responsible for admission of well newborns to the normal nursery. c) The resident is on Intensive Care Nursery is expected to attend all C-sections, and all vaginal deliveries at which the need for neonatal resuscitation is anticipated. d) During the third year, each resident spends six weeks as “Pediatrics Chief”, supervising the care of all intensive care nursery care provided by more junior residents. e) Daily obstetric and pediatric lectures are held for residents on service in conjunction with morning rounds. f) Other nursery (newborn) experience includes: i) Significant amounts of well and sick newborn care is provided in the FMC. ii) The residents are required to maintain current certification in the Neonatal Resuscitation Protocol (NRP) and PALS, accomplished with certification during the first month of residency and re-certification late in the R2 year. iii) Pediatric topics are included as part of the core didactic curriculum. iv) When on in-house obstetrics call, the resident may be called to all neonatal emergencies. 5) Evaluation: This curricular area is evaluated as outlined in the policy “Evaluation of Residents”. RAC Reviewed and Approved: David Smith, MD, Program Director