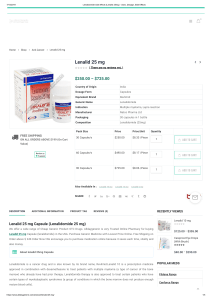
lenalidomida en pacientes con mieloma múltiple y en hemodiálisis
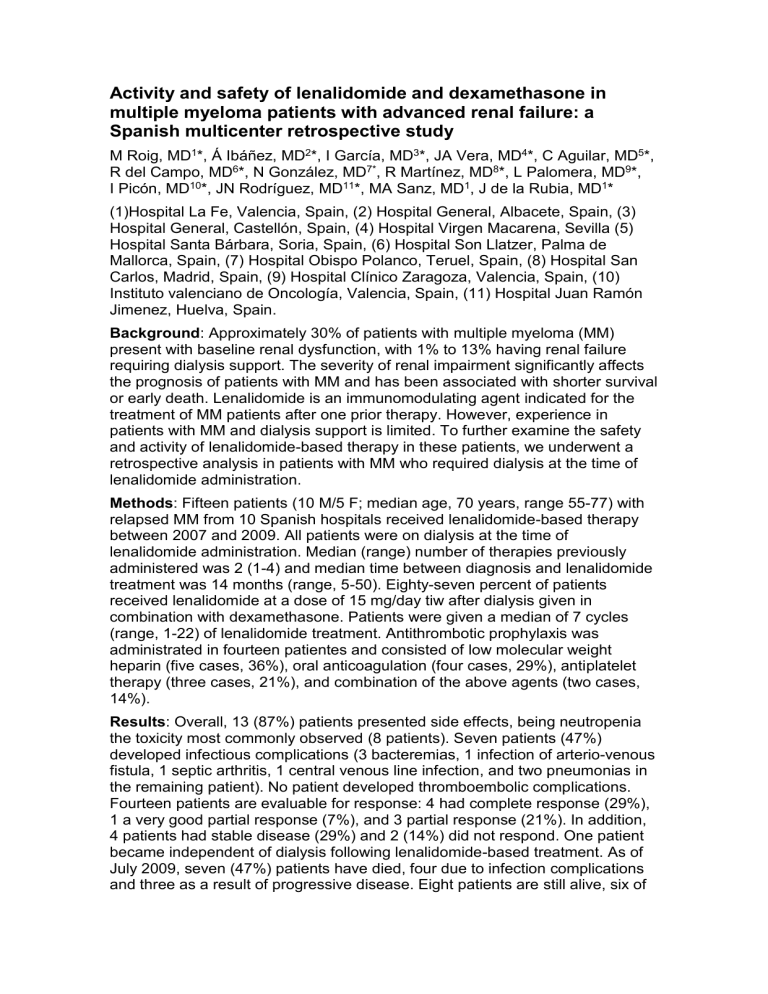
Activity and safety of lenalidomide and dexamethasone in multiple myeloma patients with advanced renal failure: a
Spanish multicenter retrospective study
M Roig, MD 1 * , Á Ibáñez, MD 2 *, I García, MD 3 *, JA Vera, MD 4 *, C Aguilar, MD 5 *,
R del Campo, MD 6 *, N Gon zález, MD 7* , R Martínez, MD 8 *, L Palomera, MD 9 *,
I
Picón, MD 10 *,
JN Rodríguez, MD 11 *, MA Sanz, MD 1 , J de la Rubia, MD 1 *
(1)Hospital La Fe, Valencia, Spain, (2) Hospital General, Albacete, Spain, (3)
Hospital General, Castellón, Spain, (4) Hospital Virgen Macarena, Sevilla (5)
Hospital Santa Bárbara, Soria, Spain, (6) Hospital Son Llatzer, Palma de
Mallorca, Spain, (7) Hospital Obispo Polanco, Teruel, Spain, (8) Hospital San
Carlos, Madrid, Spain, (9) Hospital Clínico Zaragoza, Valencia, Spain, (10)
Insti tuto valenciano de Oncología, Valencia, Spain, (11) Hospital Juan Ramón
Jimenez, Huelva, Spain.
Background : Approximately 30% of patients with multiple myeloma (MM) present with baseline renal dysfunction, with 1% to 13% having renal failure requiring dialysis support. The severity of renal impairment significantly affects the prognosis of patients with MM and has been associated with shorter survival or early death. Lenalidomide is an immunomodulating agent indicated for the treatment of MM patients after one prior therapy. However, experience in patients with MM and dialysis support is limited. To further examine the safety and activity of lenalidomide-based therapy in these patients, we underwent a retrospective analysis in patients with MM who required dialysis at the time of lenalidomide administration.
Methods : Fifteen patients (10 M/5 F; median age, 70 years, range 55-77) with relapsed MM from 10 Spanish hospitals received lenalidomide-based therapy between 2007 and 2009. All patients were on dialysis at the time of lenalidomide administration. Median (range) number of therapies previously administered was 2 (1-4) and median time between diagnosis and lenalidomide treatment was 14 months (range, 5-50). Eighty-seven percent of patients received lenalidomide at a dose of 15 mg/day tiw after dialysis given in combination with dexamethasone. Patients were given a median of 7 cycles
(range, 1-22) of lenalidomide treatment. Antithrombotic prophylaxis was administrated in fourteen patientes and consisted of low molecular weight heparin (five cases, 36%), oral anticoagulation (four cases, 29%), antiplatelet therapy (three cases, 21%), and combination of the above agents (two cases,
14%).
Results : Overall, 13 (87%) patients presented side effects, being neutropenia the toxicity most commonly observed (8 patients). Seven patients (47%) developed infectious complications (3 bacteremias, 1 infection of arterio-venous fistula, 1 septic arthritis, 1 central venous line infection, and two pneumonias in the remaining patient). No patient developed thromboembolic complications.
Fourteen patients are evaluable for response: 4 had complete response (29%),
1 a very good partial response (7%), and 3 partial response (21%). In addition,
4 patients had stable disease (29%) and 2 (14%) did not respond. One patient became independent of dialysis following lenalidomide-based treatment. As of
July 2009, seven (47%) patients have died, four due to infection complications and three as a result of progressive disease. Eight patients are still alive, six of
them continue on lenalidomide treatment and two discontinued therapy due to liver toxicity (1 case) and progressive disease (1 case).
Conclusion : These results suggest that lenalidomide-based regimens can be used in MM patients requiring dialysis, with a good response rate. The high incidence of neutropenia and infectious complications highlights the need of a close monitoring of these patients. Further studies will more formally evaluate the impact of lenalidomide-based regimens in this patient population.