ST210_SurgicalPositioning_Handout
advertisement
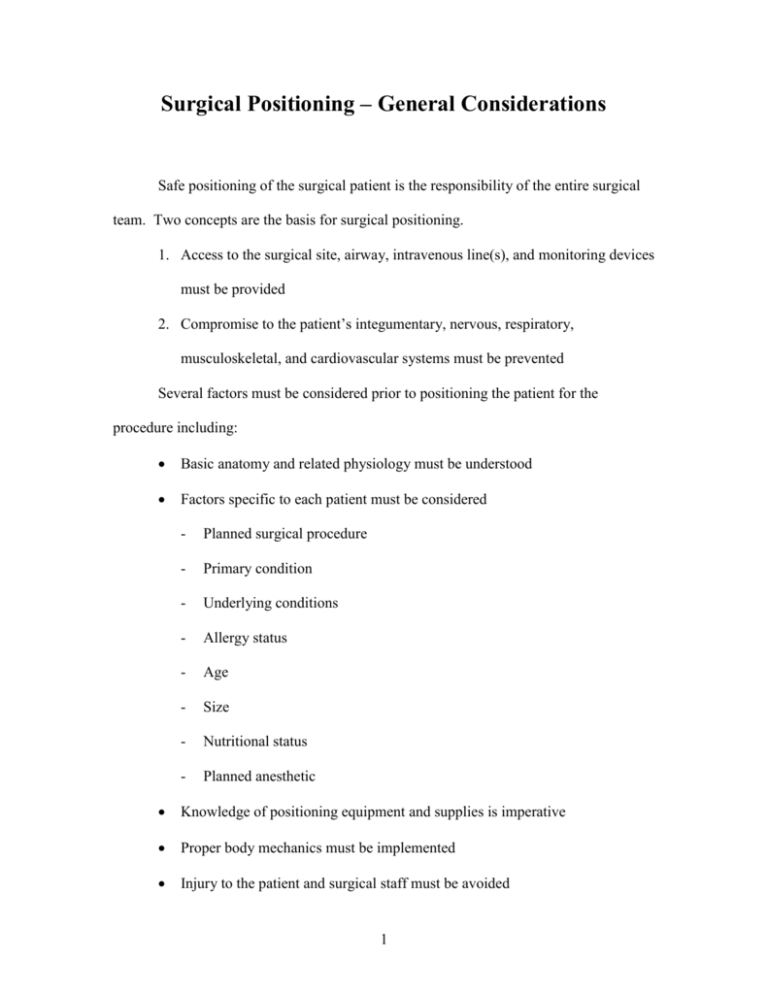
Surgical Positioning – General Considerations Safe positioning of the surgical patient is the responsibility of the entire surgical team. Two concepts are the basis for surgical positioning. 1. Access to the surgical site, airway, intravenous line(s), and monitoring devices must be provided 2. Compromise to the patient’s integumentary, nervous, respiratory, musculoskeletal, and cardiovascular systems must be prevented Several factors must be considered prior to positioning the patient for the procedure including: Basic anatomy and related physiology must be understood Factors specific to each patient must be considered - Planned surgical procedure - Primary condition - Underlying conditions - Allergy status - Age - Size - Nutritional status - Planned anesthetic Knowledge of positioning equipment and supplies is imperative Proper body mechanics must be implemented Injury to the patient and surgical staff must be avoided 1 - Chemical - Electrical - Mechanical (gravity, friction, shearing) - Thermal Surgeon and anesthesia provider preferences must be considered For the safety and comfort of the patient – as well as your own safety, many basic safety measures must be followed each time the patient is transferred or positioned. Patient identification and assessment (including allergy status and surgical site confirmation) occurs prior to transportation to the OR A minimum of two individuals should be available to assist the mobile patient A minimum of four individuals should be available to assist the immobile patient The patient is assessed prior to arrival in the OR and preparations are made in advance All patient care devices (such as oxygen and IV administration equipment, Foley catheter, and drainage collection devices) must be protected during transfer or positioning Adequately cover the patient – to provide warmth and privacy Provide comfort devices (such as a pillow) and adjust the head of the transport device or OR table to a comfortable level, as the patient’s condition allows The wheels of both the OR table and transportation device must be locked and the mattress stabilized 2 Lift, rather than slide the patient to prevent friction and shearing injuries (transfer devices may be used) The patient is moved slowly to maintain control of the body and allow for circulatory changes Pressure points and bony prominences should be padded to prevent gravity related injuries The patient’s skin should not come in direct contact with any metallic table parts, accessories, or unpadded surfaces to prevent electrical and gravity related injuries No part of the patient may extend beyond the table surface Restraints are used whenever indicated The anesthetized patient is not moved without permission from the anesthesia provider. The anesthesia provider directs movement of the patient. The anesthesia provider is responsible for maintaining the patient’s airway and may not be able to help lift the patient The armboard may not extend beyond a ninety degree angle The patients legs may not be crossed The patient must be protected from injury during movement of the OR table Patient care supplies (e.g. Mayo stand) and personnel may not rest on the patient The patient’s eyes must be protected from drying and abrasion Excessive torsion, flexion, and/or extension of any part of the patient’s body must be avoided 3 Prior to any surgical intervention, the patient must be transported to the operating room, transferred to the OR table, have the appropriate monitors applied, and receive their planned anesthetic. Patient monitoring and anesthesia are presented in detail in the video entitled Preoperative Case Management. A number of methods are used to transport the surgical patient to the OR. The patient may be carried or allowed to ambulate as well as use a wheelchair, gurney, or their hospital bed. In the hospital setting, use of a gurney and the patient’s bed are the most common. The basic concepts that relate to patient transportation via a gurney or the patient’s bed are as follows: The guardrails should be in the upright and secure position The safety belt is secured, if necessary The wheels are in the correct position Transport the patient slowly, feet first – be certain that all parts of the patient’s body are within the guardrails Use good body mechanics Never leave the patient unattended The patient is transferred to the OR table using one of the two following methods. 1. The mobile patient may be able to more him or herself to the OR table independently. A minimum of two nonsterile team members should be available to assist with transfer of a mobile patient Position the gurney next to the OR table Instruct the patient not to move until you give the command 4 Be sure that the wheels of both the gurney and the OR table are locked One individual should be positioned at the side of the gurney and the other at the side of the OR table Brace your bodies against the gurney and OR table to prevent any unexpected movement Instruct the patient to keep their blanket on and move to the OR table Assist the patient any way you can – for example, move the pillow from the gurney to the OR table or assist by lifting a fractured extremity Apply the safety strap, then remove the gurney 2. The immobile patient will be unable to assist with the transfer and will have to be moved onto the OR table. A minimum of four nonsterile team members should be available to assist with transfer of an immobile patient Position the gurney next to the OR table If necessary, explain the transfer procedure to the patient One individual should be positioned at the side of the gurney, another at the side of the OR table, and one at the head and foot of the gurney Brace your bodies against the gurney and OR table to prevent any unexpected movement Keep the patient covered and transfer him or her to the OR table using the preferred method Apply the safety strap, then remove the gurney 5 The three basic surgical positions and their common variations are demonstrated in the video that accompanies this study guide. Here you will learn which body region(s) may be accessed when the patient is in each position, the potential hazards to the patient, and the precautions that must be taken to prevent injury to the patient. Keep in mind that there are many variations to all of these procedures. The patient’s situation, surgeon and anesthesia provider preference, product differences, and school or facility policy may cause a variance. Supine Position Typically, the patient is placed in the supine or dorsal recumbent position prior to the administration of anesthesia. The patient may remain in the supine position for the procedure or be repositioned, as needed, once anesthetized. Any additional procedures such as application of antiembolism devices, insertion of a Foley catheter, or application/insertion of additional monitoring devices are performed prior to repositioning. Once the patient is anesthetized, you must seek permission from the anesthesia provider to reposition the patient. The anesthesia provider usually assumes the leadership role in positioning the anesthetized patient, giving the commands to the other surgical team members. Body regions that may be accessed with the patient in the supine position include: Anterior lower extremity Pelvis Abdomen Chest/Breast 6 Shoulder Head and neck Upper extremity The following potential hazards and necessary precautions apply to the patient in the supine position. Potential Hazard 1. Brachial plexus injury 2. Ulnar nerve injury 3. Pressure injury to skin, blood vessels, and nerves 4. Back and neck pain 5. Hypo/hyperthermia 6. Corneal drying and abrasion 7 Precautionary Action(s) Position armboard at less than a 90º angle Pad elbows Place arms on armboards with palms facing upward Place arms next to patient’s body with palms facing inward Pad all bony prominences Uncross ankles Be sure restraining devices are not restrictive Use egg crate padding or gel pads on the OR table No part of the patient’s body is to extend beyond the padded OR table Excessive torsion, flexion, and/or extension of any part of the patient’s body must be avoided Legs are parallel and the spine is in alignment Provide lumbar support pillow Head is stabilized on a pillow or foam headrest Adjust OR temperature Provide or remove blankets Implement use of hypo/hyperthermia unit Solutions (IV and irrigation) correct temperature Provide warm humidified inhalation agents Lubricate eyes Secure eyes in the closed position Prevent pressure on the eyelids 7. Foot drop 8. Electrical injury Use padded foot board No part of the patient’s body is allowed to contact any metal object Trendelenburg’s Position Trendelenburg’s position is a modification of the supine position. It is used to displace the abdominopelvic organs cephalad to provide better visualization of the surgical site. Another benefit of the Trendelenburg position is that blood flow to the lower body is reduced and venous drainage is promoted. Conversely, the position may be used to increase blood flow to the upper body, as in the treatment of shock or for distention of blood vessels to be cannulated. Body regions that may be accessed with the patient in the supine position include: Pelvis Lower abdomen The following potential hazards and necessary precautions apply to the patient in the Trendelenburg’s position, in addition to those previously listed for the supine position. Potential Hazard 1. Cardiovascular and respiratory compromise Precautionary Action(s) Decrease angle of OR table Return patient to supine position as soon as possible Flex leg section of the OR table Use padded shoulder braces Use antiembolism devices Raise leg section of the OR table 2. Pressure injury to skin, blood vessels, and nerves Note: Special attention is given to the peroneal nerves 3. Patient movement toward the head of the OR table 4. Venous stasis 8 5. Blood pressure changes slowly prior to leveling the table Level the OR table slowly Reverse Trendelenburg Position The reverse Trendelenburg position is a modification of the supine position. It is used to displace the abdominal organs caudad to provide better visualization of the surgical site. Other benefits of the reverse Trendelenburg position is that blood flow to the upper body is reduced, venous drainage is promoted, and respiration is facilitated. Body regions that may be accessed with the patient in the reverse Trendelenburg position include: Upper abdomen Head and neck The following potential hazards and necessary precautions apply to the patient in the reverse Trendelenburg position, in addition to those previously listed for the supine position. Potential Hazard 1. Patient movement toward the foot of the OR table 2. Venous stasis 3. Blood pressure changes Precautionary Action(s) Use a padded foot board Safety strap is placed approximately 2” distal to the knees Pillows or the kidney lift may be used Use antiembolism devices Level the OR table slowly Lithotomy Position The lithotomy position is a modification of the supine position. Body regions that may be accessed with the patient in the lithotomy position include: Perineum 9 Anus and rectum Vagina Urethra The following potential hazards and necessary precautions apply to the patient in the lithotomy position, in addition to those previously listed for the supine position. Potential Hazard 1. Crushing or shearing injury to the hand 2. Pressure injury to skin, blood vessels, and nerves Note: Special attention is given to the peroneal nerves 3. Back, knee, and hip pain 4. Blood pressure changes 5. Venous stasis 6. Cardiovascular and respiratory compromise 10 Precautionary Action(s) Arms are placed on armboards If arms are positioned at the patient’s sides, the hands must be observed during table movement Pad feet and ankles Be sure restraining devices are not restrictive Excessive torsion, flexion, and/or extension of any part of the patient’s body must be avoided The legs may not come in direct contact with the stirrups Stirrups are adjusted to an equal height and length Legs are raised and lowered slowly and simultaneously by two individuals Buttocks rests completely on the OR table Stirrups are adjusted to an equal height and length Legs are raised and lowered slowly and simultaneously by two individuals Legs are raised and lowered slowly and simultaneously by two individuals Use antiembolism devices Restrict accompanying use of Trendelenburg’s position Decrease leg height and hip flexion Return patient to the supine position as soon as possible Fowler’s Position The Fowler’s position is a modification of the supine position. Fowler’s position provides improved access to the surgical site and reduces blood flow to the upper body, promotes venous drainage, and facilitates respiration. Air embolism is a potential concern when the patient is in the Fowler’s position. Body regions that may be accessed with the patient in the Fowler’s position include: Breast Head and neck Shoulder The following potential hazards and necessary precautions apply to the patient in the Fowler’s position, in addition to those previously listed for the supine position. Potential Hazard 1. Blood pressure changes Note: Postural hypotension is of special concern 2. Respiratory compromise 3. Venous stasis 4. Patient movement on the OR table 5. Pressure injury to skin, blood vessels, and nerves Note: Special attention is given to the sciatic nerves Precautionary Action(s) Make adjustments to the OR table slowly Note: A pneumatic compression device may be useful in combatting postural hypotension If arms are not placed on a armboard, they will be placed and restrained on a pillow resting across the abdomen, NOT on the chest Use antiembolism devices Padded footrest may be used Upper body may be restrained Neurosurgical headrest may be used Pad pressure points Note: Special attention is given to the ischial tuberosities 11 Lateral Position The lateral position is also referred to as the lateral recumbent or lateral decubitus position. The patient in the right lateral position is placed on the OR table with the right side downward, exposing the left side of the body. All preoperative procedures, such as Foley catheter insertion, must be performed prior to placement in the lateral position. Body regions that may be accessed with the patient in the lateral position include: Retroperitoneal space Hip Hemithorax The following potential hazards and necessary precautions apply to the patient in the lateral position, in addition to those previously listed for the supine position. Potential Hazard 1. Respiratory compromise Note: Due to gravitational forces the lower lung is better perfused, but contains less residual air due to diaphragmatic and mediastinal compression 2. Circulatory compromise Note: Arterial circulation to the lower body is restricted, as is venous return 3. Movement on the OR table 4. Pressure injury to skin, blood vessels, and nerves Note: The peroneal nerve, brachial plexus, and the vascular structures of the axilla are of special concern 12 Precautionary Action(s) Positive pressure ventilation is implemented Maintain cervical alignment An axillary roll is placed Use antiembolism devices Avoid excessive compression of the abdomen Blood pressure is measured from the lower arm Lower leg is flexed Safety strap is applied over the hip, if possible An upper body restraint may be necessary Pillows are placed between the knees and ankles An axillary roll is placed Arms are placed on a double padded armboard. The palm of the lower hand faces upward and the palm of the upper 5. Foot drop hand faces downward The head is in alignment with the spine Support foot and ankle of upper leg Kidney Position The kidney position is a modification of the lateral position. Body regions that may be accessed with the patient in the kidney position include: Retroperitoneal space The following potential hazards and necessary precautions apply to the patient in the kidney position, in addition to those listed for the supine and lateral positions. Potential Hazard 1. Abdominal compression 2. Circulatory compromise Precautionary Action(s) The large kidney rest is attached anteriorly Both kidney rests must be well padded Be sure patient is positioned correctly over the kidney lift Lower kidney lift as soon as possible Reduce table flexion as soon as possible Be sure patient is positioned correctly over the kidney lift Lower kidney lift as soon as possible 3. Venous stasis Note: Reducing table flexion will also facilitate tissue approximation Use antiembolism devices Note: The dependent arm and leg are at greatest risk 4. Shoulder pain 5. Muscle strain to the torso 6. Blood pressure changes 13 Place a chest roll Use the least possible amount of table flexion Reduce table flexion as soon as possible Be sure patient is positioned correctly over the kidney lift Lower kidney lift as soon as possible Fluid management Sims’ Position The Sims’ position is a modification of the left lateral position. This is the preferred position for endoscopy performed via the anus. The patient is often awake is able to assist with positioning. Body regions that may be accessed with the patient in the Sims’ position include: Anus The potential hazards and necessary precautions that apply to the patient in the supine and lateral positions apply to the Sims’ position. Prone Position Prior to placement in the prone position, the patient is anesthetized on the gurney or another OR table. All preoperative procedures, such as Foley catheter insertion, must be performed prior to placement in the prone position. Body regions that may be accessed with the patient in the prone position include: Posterior lower extremity Dorsal body surface Spine Posterior cranium The following potential hazards and necessary precautions apply to the patient in the prone position, in addition to those previously listed for the supine position. Potential Hazard 1. Pressure on abdominal contents and 14 Precautionary Action(s) Use chest rolls thoracic compression Note: The vena cava and abdominal aorta are of particular concern 2. Pressure injury to skin, blood vessels, and nerves Use axillary rolls Use antiembolism devices Move breasts laterally Place arms on armboards, rather than at the patient’s sides Be sure all pressure on the male genitalia is removed Place pillows under the knees and ankles Place padding under the knees Flex arms on armboards with the palms facing downward or along the sides of the body with the palms facing inward Use antiembolism devices Elevate lower portion of the legs Lower and rotate arms for placement on armboards 3. Venous statis 4. Shoulder injury Kraske (Jackknife) Position The Kraske position is a modification of the prone position. Body regions that may be accessed with the patient in the prone position include: Anus Pilonidal area The following potential hazards and necessary precautions apply to the patient in the Kraske position, in addition to those previously listed for the supine and prone positions. 1. Potential Hazard Blood pressure changes 15 Precautionary Action(s) Return the patient to the horizontal position slowly