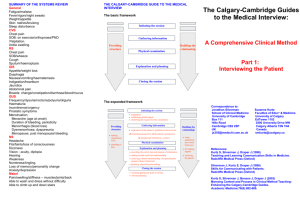
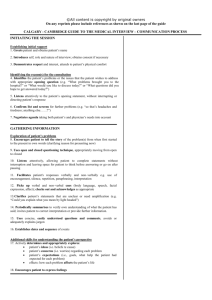
CALGARY - CAMBRIDGE OBSERVATION GUIDE TO THE
advertisement
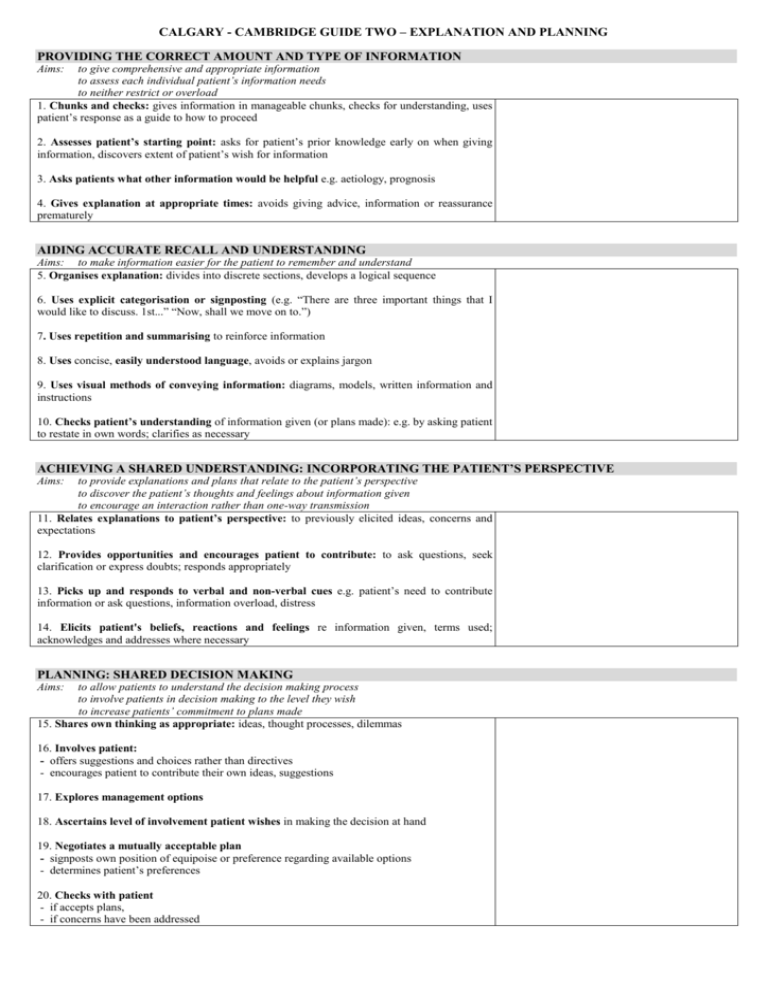
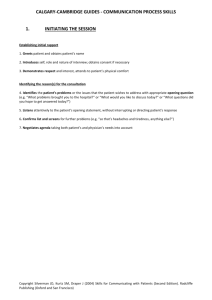
CALGARY - CAMBRIDGE GUIDE TWO – EXPLANATION AND PLANNING PROVIDING THE CORRECT AMOUNT AND TYPE OF INFORMATION Aims: to give comprehensive and appropriate information to assess each individual patient’s information needs to neither restrict or overload 1. Chunks and checks: gives information in manageable chunks, checks for understanding, uses patient’s response as a guide to how to proceed 2. Assesses patient’s starting point: asks for patient’s prior knowledge early on when giving information, discovers extent of patient’s wish for information 3. Asks patients what other information would be helpful e.g. aetiology, prognosis 4. Gives explanation at appropriate times: avoids giving advice, information or reassurance prematurely AIDING ACCURATE RECALL AND UNDERSTANDING Aims: to make information easier for the patient to remember and understand 5. Organises explanation: divides into discrete sections, develops a logical sequence 6. Uses explicit categorisation or signposting (e.g. “There are three important things that I would like to discuss. 1st...” “Now, shall we move on to.”) 7. Uses repetition and summarising to reinforce information 8. Uses concise, easily understood language, avoids or explains jargon 9. Uses visual methods of conveying information: diagrams, models, written information and instructions 10. Checks patient’s understanding of information given (or plans made): e.g. by asking patient to restate in own words; clarifies as necessary ACHIEVING A SHARED UNDERSTANDING: INCORPORATING THE PATIENT’S PERSPECTIVE to provide explanations and plans that relate to the patient’s perspective to discover the patient’s thoughts and feelings about information given to encourage an interaction rather than one-way transmission 11. Relates explanations to patient’s perspective: to previously elicited ideas, concerns and expectations Aims: 12. Provides opportunities and encourages patient to contribute: to ask questions, seek clarification or express doubts; responds appropriately 13. Picks up and responds to verbal and non-verbal cues e.g. patient’s need to contribute information or ask questions, information overload, distress 14. Elicits patient's beliefs, reactions and feelings re information given, terms used; acknowledges and addresses where necessary PLANNING: SHARED DECISION MAKING Aims: to allow patients to understand the decision making process to involve patients in decision making to the level they wish to increase patients’ commitment to plans made 15. Shares own thinking as appropriate: ideas, thought processes, dilemmas 16. Involves patient: - offers suggestions and choices rather than directives - encourages patient to contribute their own ideas, suggestions 17. Explores management options 18. Ascertains level of involvement patient wishes in making the decision at hand 19. Negotiates a mutually acceptable plan - signposts own position of equipoise or preference regarding available options - determines patient’s preferences 20. Checks with patient - if accepts plans, - if concerns have been addressed CLOSING THE SESSION Forward planning 21. Contracts with patient re next steps for patient and physician 22. Safety nets, explaining possible unexpected outcomes, what to do if plan is not working, when and how to seek help Ensuring appropriate point of closure 23. Summarises session briefly and clarifies plan of care 24. Final check that patient agrees and is comfortable with plan and asks if any corrections, questions or other issues Additional comments References: Kurtz SM, Silverman JD, Draper J (2005) Teaching and Learning Communication Skills in Medicine 2nd Edition. Radcliffe Publishing (Oxford) Silverman JD, Kurtz SM, Draper J (2005) Skills for Communicating with Patients 2nd Edition. Radcliffe Publishing (Oxford) Kurtz S, Silverman J, Benson J, Draper J (2003) Marrying Content and Process in Clinical Method Teaching: Enhancing the Calga ry-Cambridge Guides Academic Medicine;78(8):802-809