Anesthesia and Analgesia
advertisement
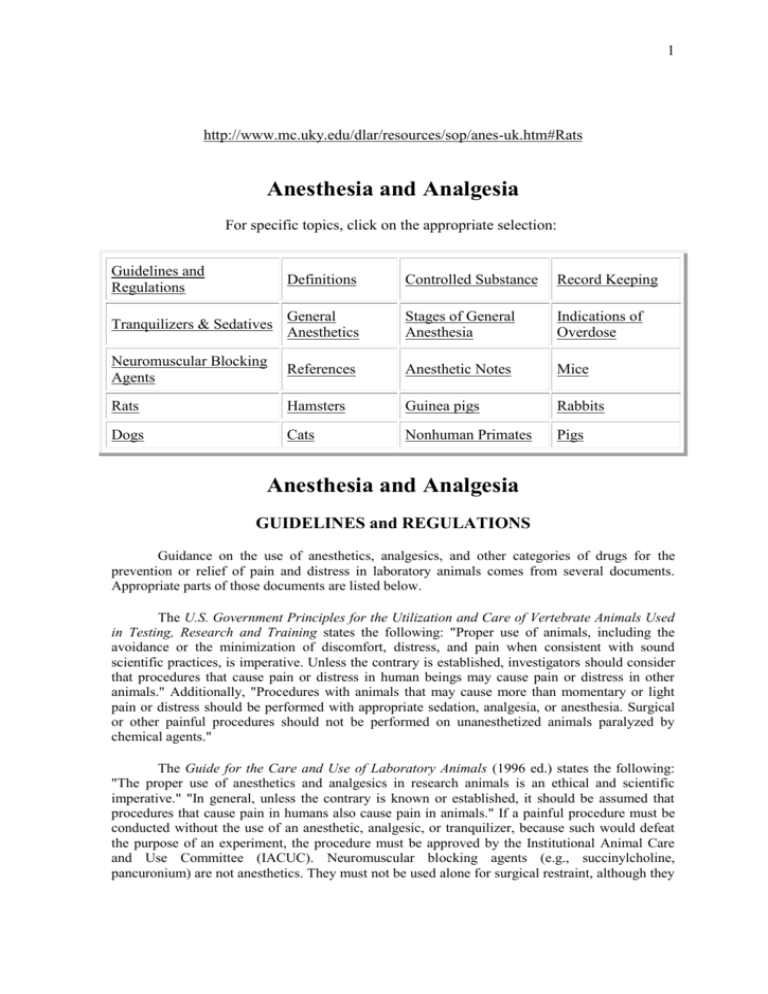
1 http://www.mc.uky.edu/dlar/resources/sop/anes-uk.htm#Rats Anesthesia and Analgesia For specific topics, click on the appropriate selection: Guidelines and Regulations Definitions Controlled Substance Record Keeping Tranquilizers & Sedatives General Anesthetics Stages of General Anesthesia Indications of Overdose Neuromuscular Blocking Agents References Anesthetic Notes Mice Rats Hamsters Guinea pigs Rabbits Dogs Cats Nonhuman Primates Pigs Anesthesia and Analgesia GUIDELINES and REGULATIONS Guidance on the use of anesthetics, analgesics, and other categories of drugs for the prevention or relief of pain and distress in laboratory animals comes from several documents. Appropriate parts of those documents are listed below. The U.S. Government Principles for the Utilization and Care of Vertebrate Animals Used in Testing, Research and Training states the following: "Proper use of animals, including the avoidance or the minimization of discomfort, distress, and pain when consistent with sound scientific practices, is imperative. Unless the contrary is established, investigators should consider that procedures that cause pain or distress in human beings may cause pain or distress in other animals." Additionally, "Procedures with animals that may cause more than momentary or light pain or distress should be performed with appropriate sedation, analgesia, or anesthesia. Surgical or other painful procedures should not be performed on unanesthetized animals paralyzed by chemical agents." The Guide for the Care and Use of Laboratory Animals (1996 ed.) states the following: "The proper use of anesthetics and analgesics in research animals is an ethical and scientific imperative." "In general, unless the contrary is known or established, it should be assumed that procedures that cause pain in humans also cause pain in animals." If a painful procedure must be conducted without the use of an anesthetic, analgesic, or tranquilizer, because such would defeat the purpose of an experiment, the procedure must be approved by the Institutional Animal Care and Use Committee (IACUC). Neuromuscular blocking agents (e.g., succinylcholine, pancuronium) are not anesthetics. They must not be used alone for surgical restraint, although they 2 can be used in "properly ventilated conscious animals for specific types of nonpainful, wellcontrolled neurophysiologic studies." Last, but certainly not least, the Animal Welfare Act (Public Law 89-544) as amended, requires that institutional veterinarians provide guidelines regarding the use of tranquilizers, anesthetics, analgesics, and euthanasia agents. In the case of a research facility, the program of adequate veterinary care shall include "the appropriate use of anesthetic, analgesic, or tranquilizing drugs..." Anesthesia is the act of providing sensation-free relief from pain or pain-producing procedures. Anesthesia must be performed by a person with knowledge of and familiarity with the drugs to be used in the animal species under consideration. It is the responsibility of the Principal Investigator to ensure adherence to proper procedures during the execution of the protocol. Investigators may arrange training for their technicians by contacting the Division of Laboratory Animal Resources (DLAR) (323-5885) or the Office of the University Veterinarian (257-2549). Definitions: Neuroleptic - produce central nervous depression, depression of excitability of the autonomic nervous system, a dulling of consciousness and a reduction of spontaneous motor activity. Analgesia - relief from pain Preemptive analgesia - managing pain before it begins Tranquilization - a state of behavioral change in which the patient is relaxed, unconcerned by its surroundings, and often, indifferent to minor pain. Sedation - a mild degree of central depression in which the patient is awake but calm; larger doses of sedative may lead to narcosis. Narcosis - a drug-induced state of sedation in which the patient is oblivious to pain. Local anesthesia - loss of sensation in a limited body area. Regional anesthesia - insensibility in a larger, though limited, body area. Basal anesthesia - a light level of general anesthesia usually produced by preanesthetic agents. It serves as a basis for deeper anesthesia on administration of other agents. General anesthesia - complete unconsciousness Surgical anesthesia - unconsciousness, accompanied by muscular relaxation to such a degree that surgery can be performed painlessly and without struggle on the part of the patient. Neuroleptanalgesia - a state of central nervous system depression and analgesia usually produced by a combination of a neuroleptic and a narcotic analgesic. Factors Affecting Choice of Anesthetic and Analgesic Regimens 3 Dosage charts for anesthetic and analgesic agents state only the average amount of drug that would be expected to produce a desired level of anesthesia or analgesia under standard conditions. Consequently, animals must be monitored carefully and the dosages tailored to meet each clinical and research situation. The DLAR veterinarian(s) are available for consultation on the selection of the best agent and dosage to meet specific research needs. Many factors can affect the activity of anesthetics. The species, strain, sex, age, physiologic status, relative body size, disposition/demeanor, presence of concurrent pain or distress, or medication are known to cause a variation in the amount of drug needed to produce a desired effect in an individual animal. Numerous studies have shown that preemptive analgesia, managing pain before it begins, holds significant benefits for the animal. If the selected analgesic does not interfere with the research parameters, the quality of the data produced by use of the animal can be improved when the stress secondary to pain is removed. Analgesia is more effective when given before a painful procedure is introduced, and preemptive analgesia should be used whenever possible. The duration of anesthesia produced by the anesthetic should coincide with the expected duration of the operative procedure. The duration of analgesia produced by the analgesic should coincide with the expected duration and intensity of post-operative pain generated by the procedure. The time required for post-surgical recovery from anesthesia, as well as the frequency of administration of analgesics should coincide with the level of post-surgical care that is available. Knowledge, experience and skill with available agents and equipment can affect the outcome of the use of anesthetics and analgesics. Safety precautions would include the protection of humans from vapors of volatile anesthetics. This is best accomplished by the use of an approved gas scavenging system, or by using the volatile anesthetic agent inside an approved fume hood. Many of the drugs described in this section have the potential for human abuse. Therefore, they must be maintained in a manner that is in compliance with all federal laws and requirements for the handling and storage of controlled substances. Drugs that are subject to control under the Drug Enforcement Agency (DEA) must be stored in a locked cabinet. Controlled Substance Public Law 91-513, Section 202: "There are five schedules of controlled substances, to be known as schedules I, II, III, IV, and V." Oversight for compliance with the law resides with the Drug Enforcement Agency (DEA). Schedule I - "The substances in this schedule are those that have no accepted medical use in the United States and have a high abuse potential." Schedule II - "The substances in this schedule have a high abuse potential with severe physic or physical dependence liability. Schedule II controlled substances consist of certain narcotic, stimulant and depressant drugs." Schedule III -"The substances in this schedule have an abuse potential less than those in Schedules I and II, and include compounds containing limited quantities of certain narcotic drugs and nonnarcotic drugs..." 4 Schedule IV- "The substances in this schedule have an abuse potential less than those listed in Schedule III..." Schedule V - "The substances in this schedule have an abuse potential less than those listed in Schedule IV and consist primarily of preparations containing limited quantities of certain narcotic and stimulant drugs..." Record Keeping Requirements: A written record is required when any DEA controlled substances are used. The record should reflect the purchase/acquisition date of each drug, the volume received, the date and volume of each use of the drug, and the volume of drug remaining in the inventory. Each entry in the record should be signed by the person authorized to dispense the drug. Individual animal clinical records should be annotated to reflect the use of the agents described above, showing the date and dose. All records should be stored in such a way that they are readily available for review by members of the IACUC, by authorized inspectors from the Office of Laboratory Animal Welfare (OLAW), the DEA, and/or the U.S. Department of Agriculture. Pretreatment of the Surgical Patient: Drugs such as anticholinergics, tranquilizers, or sedatives are given as anesthetic pretreatment for a variety of reasons. The primary goal of pretreatment with the majority of these agents is to minimize anxiety or excitement of the patient. Some drugs may be used to ease the transition to the first plane(s) of anesthesia, to decrease the amount of anesthetic agent, to prevent vomiting, or to control secretions. Anticholinergic: (e.g., atropine sulfate, glycopyrrolate) These agents block parasympathetic impulses to the cardiopulmonary system, glands and smooth muscle. Consequently, they prevent vasovagal reflexes, with concurrent slowing of the heart, and reduce salivary gland and bronchial secretions. The effectiveness of atropine varies among species. Tranquilizers/Sedatives: (Tranquilizers = phenothiazines [e.g., acepromazine] and butyrophenones [e.g., droperidol and azaperone]) (Sedatives = barbiturates, benzodiazepines [e.g., diazepam, zolazepam]). The distinction between tranquilizers and sedatives is mainly semantic. One differentiating characteristic, however, is that tranquilizers at high dose levels tend to produce side effects without a loss of consciousness. Sedatives at high dose levels cause a profound CNS depression that resembles anesthesia. Tranquilizers calm the animal, facilitate handling for anesthetic induction, and reduce the amount of anesthetic required for induction and maintenance of general anesthesia, thereby decreasing the undesirable side-effects of the anesthetic agent. Tranquilizers also may enhance smooth anesthetic recoveries (usually in conjunction with analgesics). Tranquilized animals can be readily aroused by painful stimulation because tranquilizers do not produce analgesia. Tranquilizers can, in some settings, provide skeletal muscle relaxation when the relaxation produced by the anesthetic agent is insufficient. This effect may be observed in rabbits and cats 5 with the administration of a combination of acetylpromazine and ketamine hydrochloride. This activity is not as pronounced, however, as the skeletal muscle relaxation which results from the administration of neuromuscular blocking agents (e.g. succinylcholine). Sedatives produce a mild degree of central nervous system (CNS) depression in which the animal is conscious but calm and not nervous. These agents will produce a psychological calming of an animal but do not exert hypnotic or analgesic effects. Animals can become aroused and can react to painful procedures. Loud noise stimulation can reverse the calming effects of these drugs. When used as preanesthetics, ample time should be allowed for the drug to reach its maximum effect, before attempting to induce anesthesia. All tranquilizers and sedatives share many of the described characteristics, but each drug has its own diverse pharmacologic properties, along with contraindications. Alpha2-Adrenergic Agonists: ( e.g., xylazine, detomidine, medetomidine) This class of drugs mediates analgesia, anxiolysis, sedation, sympatholysis, and control of hypertension. These drugs are usually classified as sedative-analgesics and skeletal muscle relaxants. There is wide species variation in the reaction to these drugs. Xylazine sedation may be reversed using yohimbine, tolazoline, or idazoxan. Atipamezole is a highly selective and potent 2-antagonist that rapidly reverses sedation as well as other behavioral and physiologic effects of medetomidine. Nonchemical pretreatment: Nonchemical pretreatment procedures, such as withholding food prior to surgery, are advisable to prevent regurgitation of stomach contents and aspiration into the respiratory tract while the animal is anesthetized. General Anesthetics: Anesthetics produce, in a controllable manner, both loss of consciousness and an absence of motor response to noxious stimuli. This unconsciousness, analgesia, and muscle relaxation should be sufficient to allow the performance of painful procedures without the subject experiencing pain. Animals should be in good health before the administration an anesthetic agent. The animal's physical condition should be evaluated to assure that there are no disease conditions that may compromise the well being of the animal during anesthesia. The level of anesthesia should be limited to the induction of the minimal degree of CNS depression necessary for performing the procedure. When an injectable anesthetic agent is used, drug dose calculation should be based on body weight and age. Because of the wide variation within and among species, there is really no such thing as a predetermined anesthetic dose. General anesthesia must be given "to effect," as noted in physiologic responses and in response to noxious stimuli. It is important to realize that some drugs take time to take effect. Many anesthetic deaths can be attributed to giving the anesthetic insufficient time to work. This is especially true of parenterally administered drugs (e.g., barbiturates) - once they are injected, there is little the anesthetist can do to control the outcome. 6 To avoid hypothermia, body temperature should be monitored and maintained throughout the anesthetic process. Conservation of body heat is an integral part of anesthetic management. Especially in small animals, core body temperature can fall precipitously during general anesthesia. Hypothermia, when added to other factors, can produce an irreversible sequence of events leading to death. To avoid thermal burns, water heating pads rather than electrical pads, should be used. During lengthy procedures, anesthetized animals may become dehydrated. To help maintain normal hemodynamics, warm, balanced electrolyte solutions should be administered, by continuous intravenous drip, throughout the surgical procedure. Rodents may be administered fluids via the subcutaneous route. The anesthetist's responsibility for the animal’s welfare extends beyond the completion of the surgical procedure. Continuous monitoring by a trained person should be provided until the animal is able to maintain itself in sternal recumbency and is breathing normally. Some anesthetics and analgesics affect animals for days after administration. Therefore, it is important to check animals daily for signs of anorexia, fever, vomiting, or abnormal respiration or heart rate. Stages of General Anesthesia Stage I Stage of Analgesia; loss of pain without loss of consciousness or sense of touch. This stage exists from the moment of induction to the loss of consciousness. Respiration is unchanged, and the pupils may not change or exhibit moderate reflex dilation. Analgesia is present. Stage II Excitement Stage: loss of consciousness to the onset of regular respiration. In this stage, the higher cerebral centers are depressed with loss or inhibition of the secondary centers. Excitement and struggling may occur. This is one of the danger periods of anesthesia during which vomiting and physical injury may take place. Therefore, the anesthetist should strive to cause the patient to pass through this stage as quickly as possible. In order to obtain a smooth and rapid induction, careful attention must be paid to proper and adequate premedication, proper restraint of the animal, and minimal sensory stimuli. Respiration is irregular; there may be periods of breath-holding. The pupils show reflex dilation. Muscular tone is increased, while analgesia is present. Stage III Surgical Anesthesia: from the onset of regular respiration to the cessation of spontaneous respiration due to central respiratory paralysis from the action of the anesthetic agent. Plane 1 - Respiration is regular with an increase in tidal volume. There is nystagmus and the pupils are constricted. There is a loss of the vomiting, eyelid, and pharyngeal reflexes. Small muscle tone is lost. Although swallowing is retained in upper first plane, it is of value primarily in recovery from anesthesia. Plane 2 - Respiration is regular but shallower. The eyeballs are fixed (central) and the pupil is in mid-dilation. There is a loss of the corneal, visceral, laryngeal, and cough reflexes. The large muscles are beginning to relax in this plane. 7 Plane 3 - This plane is entered when there is the beginning of progressive intercostal muscle lag, in which diaphragmatic movement precedes the action of the intercostals. It ends with the cessation of intercostal movement. The pupil is moderately dilated and all muscle tone (except diaphragmatic) is lost. Plane 4 - Respiration shows complete intercostal paralysis and breathing is diaphragmatic. Inspiration is short and gasping, with retraction of the intercostal spaces. The pupils show paralytic dilatation. Stage IV - begins with respiratory paralysis and progresses quickly to circulatory failure. Pertinent notes on the signs of anesthesia The eyelash reflex is related to the eyelid reflex. If the eyelash is stroked or the eyelid is opened, the patient will actively attempt to close its eye in the second stage. In the third stage, the eyelid will close passively, or will remain open, and stroking the eyelash will elicit no response. Since swallowing will occur before vomiting when the patient is becoming "light," the continuous presence of the anesthetist’s hand on the patient’s chin may aid in detecting signs of swallowing, and permit an increase in the depth of anesthesia before vomiting occurs. Pupillary size may be influenced by pre-anesthetic drugs, and may not be a reliable sign of anesthetic depth. However, a widely dilated pupil, with little or no iris visible, should always cause concern, since it may be the result of excessively deep anesthesia or hypoxia. Evaluation of anesthetic effects: Test pedal (toe pinch) and palpebral reflexes, and the tone of jaw and anal sphincter muscles. Reflexes are absent and muscle tone is relaxed during surgical anesthesia. Monitor depth and rate of respiration - increase in depth and decrease in rate signifies surgical anesthesia. Monitor heart rate - slowing indicates surgical anesthesia. An increase in rate during the performance of a surgical procedure often indicates that the depth of anesthesia is not adequate and the animal is feeling pain. A decrease of rate during surgery may signify an overdose of anesthetic. Monitor body temperature - temperature falls during anesthesia; warming causes faster metabolism of anesthetic agent. Maintain body temperature at normal levels, usually 37ºC, if possible Indications of anesthetic overdose: Heart rate - may be rapid or slow, depending on the animal's state of physiological decompensation. Pulses - may be weak, or even imperceptible. Blood pressure - reduced to shock level. Cardiac dysrhythmias - may be noted. 8 Capillary refill time - progressively slows to 3 or more seconds. Respiration - slow and irregular; often becomes diaphragmatic; may eventually cease. Mucous membrane/skin colors - pale to cyanotic. Gastrointestinal, ocular, musculoskeletal, and nervous system reflexes - greatly diminished or cease. Interventions for anesthetic overdose: Turn off gas anesthetics. If reversible anesthetics are on board, administer reversal agent. Mechanically ventilate with oxygen. Administer isotonic fluids, intravenously or intraperitoneally. Warm animal to increase body temperature. If available, administer antidote/reversal agent. Neuromuscular Blocking Agents (Immobilizing Drugs or Paralytics): Neuromuscular blocking agents inhibit the transmission of nerve impulses at the neuromuscular junction (e.g., succinylcholine) or at spinal synapses (e.g., mephenesin, guaifenesin) resulting in skeletal muscle paralysis and profound muscular relaxation without loss of consciousness. These agents are used as an adjuvant in surgical anesthesia to obtain more complete muscle relaxation for specific procedures; i.e. bone fracture repair in heavily muscled animals (horses). Depolarizing neuromuscular blocking drugs (e.g., succinylcholine) cannot be reversed. Competitive neuromuscular blocking agents (e.g., d-tubocurarie, pancuronium) can be reversed. These agents produce muscle paralysis only. They do not produce sedation or analgesia. These agents should never be used as anesthetic or analgesic agents (9 CFR 2.31: NRC. 1996: PHS. 1996). Anesthesia is the act of providing sensation-free relief from pain or pain-producing procedures. Anesthesia must be performed by a person with knowledge of and familiarity with the drugs to be used in the animal species under consideration. It is the responsibility of the Principal Investigator to ensure adherence to proper procedures during the execution of the protocol. Investigators may arrange training for their technicians by contacting the Division of Laboratory Animal Resources (DLAR) (323-5885) or the Office of the University Veterinarian (257-2549). REFERENCES Code of Federal Regulations, Title 9 (Animals and Animal Products), Subchapter A (Animal Welfare), Parts 1-3. Guide for the Care and Use of Laboratory Animals, Institute of Laboratory Animal Resources, Commission of Life Sciences, National Research Council. Washington, D.C., National Academy Press, 1996. 9 Public Health Service Policy on Humane Care and Use of Laboratory Animals, Office for Protection from Research Risks, National Institutes of Health, U.S. Department of Health and Human Services. Washington, D.C, 1996. Principles and Practices of Veterinary Anesthesia, Short, Charles E. (ed.) Baltimore: Williams & Wilkins, 1987 Lumb & Jones’ Veterinary Anesthesia, Thurmon, John C., Tranquilli, W.J., & Benson, G.J. (eds.) Third Edition, Philadelphia: Lea & Febiger, 1996. Goodman & Gilman’s The Pharmacological Basis of Therapeutics, Hardman, Joel, G., Limbird, L.E., Onlinoff, O.B., et. al., (eds.) Ninth Edition, New York: McGraw-Hill, 1996. Veterinary Pharmacology and Therapeutics, 7th ed., Adams, H. Richard (ed.), Iowa State University Press, Ames, 1995 ANESTHETIC NOTES Several commonly-used anesthetics and analgesic medications are described briefly below. However, numerous additional agents are available for use in a variety of species. Please contact a DLAR veterinarian for additional information on drugs that are not listed. A veterinary drug formulary and a number of anesthesia textbooks are available in the DLAR office. Acepromazine Maleate: Acepromazine maleate (formerly acetylpromazine), a phenothiazine derivative, is a potent neuroleptic agent with relatively low toxicity. Acepromazine induces tranquilization, muscle relaxation, and a decrease in spontaneous activity. At high doses, sedation occurs. Preanesthetic administration decreases the amount of general anesthetic required. Acepromazine possesses antiemetic, anticonvulsant, antispasmodic, hypotensive, and hypothermic properties. Acepromazine will prevent or decrease severity of the malignant hyperthermia syndrome in susceptible swine exposed to halothane. Acepromazine potentiates opiates such as butorphanol, buprenorphine which if used in combination as a pre-anesthetic, will provide sedation as well as preemptive analgesia. Chloral hydrate: Chloral hydrate should not be used in species other than rodents. The IP dosage for a surgical plane of anesthesia in rodents is 300-400 mg/kg body weight. Unfortunately, because this dosage approaches the LD50 for this agent, dosages sufficient to provide surgical anesthesia and analgesia approach lethality. Much lower dosages (30-35 mg/kg body wt) that are reported in the literature are hypnotic doses and are inadequate for surgical procedures. Chloral hydrate has been reported to cause adynamic ileus in the rat. This condition involves an accumulation of fluid and gas in the intestine and can be avoided by using a low concentration of drug (3-4% solution, rather than a 7-8% solution). Adverse effects include severe respiratory depression and cardiovascular and thermoregulatory depression. Equi-Thesin: No longer commercially available, but can be prepared in the following manner. Dissolve 8.5 mg of chloral hydrate in 20 ml 95-100% ethanol. Then add 1.96 g pentobarbital (Nembutal = 50 mg/ml) and 4.25 g MgS04. After everything else is in solution, add 60 ml propylene glycol. Bring up to total volume of 200 ml with water (water can be added at any stage). Dose for rats is 1 ml/300 g IP. Ether: Because of the serious hazard created by the highly flammable and explosive properties of ether, together with the fact that satisfactory alternative inhalatant anesthetics are available (e.g., isoflurane or halothane), use of ether as an anesthetic agent is discouraged. Because animal 10 rooms are not equipped with appropriate ventilation hoods, the use of ether in animal rooms, or in any DLAR space, is prohibited. In addition, the use of ether as a euthanasia agent is restricted because of the requirement for degassing of carcasses by storage in appropriate explosion-proof refrigerators, since ether-saturated carcasses create an extremely serious hazard when they are incinerated. Fentanyl Patch: Fentanyl citrate is a very potent opiate agonist. The patch is a transdermal delivery system for the fentanyl, and it is used primarily in dogs and cats for postoperative pain, and in the control of severe pain associated with chronic pain, dull pain, and non-specific pain (e.g., associated with cancer). Therapeutic levels are achieved within 6-8 hours of application in the cat, while it takes at least 12 hours to reach therapeutic levels in the dog, so patch application should be performed prior to the painful procedure, keeping these times in mind. Small dogs and cats may be dosed with 1/2 patch, but the patch should NOT be cut in half. Cover 1/2 of the gel membrane with tape. The patch is generally placed on the dorsal cervical area, or over the shoulders. The hair at the site should be closely clipped with at least a 1 cm margin around the patch. Do not shave, as cuts, abrasions or wounds can alter the absorption of fentanyl. After clipping, wipe the skin with a damp cloth to remove small hairs and skin debris; do not scrub or surgically prepare the site. Allow to completely dry. Place patch over the clipped area and hold it in place for 2-3 minutes to maximize adherence. Use a slightly padded bandage or transparent dressing used with medical adhesive spray to assure adherence and to keep it dry. Increased temperatures can stimulate an excessive release of fentanyl from the patch, so avoid placing the patch on a heating pad. Local anesthetic: A variety of local anesthetic agents are available and may be valuable in several types of experimental procedures. For example, local infusion of an incision site with lidocaine may reduce the amount of general anesthetic that is required. Application of lidocaine gel to a suture line or a cranial implant or the use of bupivicaine to block intercostal nerves following thoracotomy, may provide considerable pain relief. Pentobarbital: Pentobarbital can induce severe cardiovascular and respiratory depression at doses close to those needed to obtain a surgical level of anesthesia, often resulting in death. To reduce the likelihood of this occurrence, pentobarbital can be administered intravenously in the following manner: calculate the required drug volume based on a mg/kg dose and draw this volume into a syringe; administer approximately half of the volume by rapid IV injection to achieve basal narcosis, and then slowly inject additional incremental volumes until surgical anesthesia is achieved. The IP route of administration should be used in rodents only. Telazol®: Telazol® is a commercially available preparation of tiletamine (50 mg/ml) and zolezapam (50 mg/ml). Urethane: Urethane is mutagenic and carcinogenic in rodents. Due to its numerous adverse effects, the use of urethane is strongly discouraged unless strict precautions are taken (e.g., gloves, face masks, mixing under a fume hood) to protect personnel. The use of urethane should be limited to nonsurvival procedures. Volatile anesthetics: Such agents include halothane, enflurane, isoflurane, sevoflurane, and desflurane. These agents should be used only with adequate ventilation or scavenging systems. Precision vaporizers must be used for these agents because lethal concentrations can easily be reached using the open drop method or using a bell jar as an anesthetic chamber. Xylazine: Xylazine (Rompun®) is a centrally-acting alpha-2 adrenergic receptor agonist with analgesic and sedative effects. Xylazine can induce profound bradycardia, decreased cardiac 11 output, emesis and depressed thermoregulation. Ruminants are extremely sensitive to xylazine. Yohimbine or 4-aminopyridine can be used to reverse the effects of xylazine. However, xylazine used is associated with a high anesthetic complication rate. The following pages provide tables of drugs commonly used for preanesthesia, anesthesia, analgesia, sedation, tranquilization, and restraint of laboratory animal species. The dosage recommendations and other data presented on the following pages are based upon current data in the literature, and the professional judgement of the University of Kentucky attending veterinarian(s). Doses published in the literature are often variable. Drugs are listed for their intended use according to species. Information on agents other than those listed may be obtained from the Division of Laboratory Animal Resources veterinarians. Variations in dose and duration of action will probably be observed due to factors such as animal strain, route of administration, weight, temperament, presence of other drugs, and state of health. Because of these considerations, animal users must be able to judge depth of anesthesia in the individual animal to avoid administration of a lethal dose or a dose that inadequately controls pain. Depth of anesthesia should be monitored frequently. Response to tissue incision indicates inadequate depth. Withdrawal response to ear pinch is a good indicator of depth in rodents and rabbits. Toe pinch and corneal reflexes are good in carnivores. Several additional factors should also be considered when performing surgery on animals. Food should be withheld for 12 hours prior to anesthesia to reduce the likelihood of aspiration of gastric material. A patent airway should be maintained during surgery, preferably by use of an endotracheal tube. Salivation and bradycardia can be controlled by use of atropine or glycopyrrolate. Glycopyrrolate is longer acting and should be used as a pre-anesthetic agent when known vagal stimulation will occur during a procedure to aid in preventing, or minimizing the cardiac effects of the stimulation. Atropine can be used to help correct bradycardia that develops during a procedure. It is faster acting than glycopyrrolate, but it is also of shorter duration. Anesthetized animals are very prone to hypothermia. They should be insulated from cold table surfaces and preferably should receive supplemental heat. Temperature should be monitored every 15 minutes during anesthesia to prevent hypo-and/or hyperthermia. Use care to avoid thermal injury from uncontrolled heat sources. If excessive blood loss occurs during surgery, replacement fluids should be given to avoid shock. Neuromuscular blocking agents, when used in surgical procedures, will be restricted to anesthetized animals. Use of any anesthetic agent must be approved by the Institutional Animal Care and Use Committee. MICE ANESTHESIA Isoflurane (Forane®) Halothane (Fluothane®) DOSE (mg/kg) & ROUTE To effect COMMENTS Inhalation; precision vaporizer required; adequate ventilation or scavenging system essential 12 Enflurane (Ethrane®) Pentobarbital Thiopental 35 IV Variable response; administer to effect 40-70 IP Up to 20 min. sleep time 50 IP 25 IV Tribromoethanol (Avertin) 125-250 IP Store at 4ºC; dark conditions Ketamine + Xylazine 100 + 10 IP Ketamine + Medetomidine 75 + 1.0 IP, SC Chloral hydrate 400 IP Use a 5% solution Hypothermia (neonate only) 3-4 min Submerge pup (to cervical area) in water + ice; 10 min. anesthesia Morphine 1-10 SC 3 hr Oxymorphone 0.05 SC 3 hr Meperidine 10-20 SC 3 hr Imipramine 2-3 SC 12 hr Butorphanol (Torbutrol® 0.5mg/ml 0.5-5 SC 6-12 hr Buprenorphine (Buprenex® 0.05-0.1 SC 6-12 hr; do not use with tribromoethanol Pentazocine 10 SC 4 hr Medetomidine 30-100µg/kg SC Reverse w/atipamezole; 1µg/kg SC, IP, or IV Ketamine 44 SC Chlorpromazine 5-10 SC ANALGESIA SEDATION 13 NOTES Small muscle mass: Mice have a relatively small total muscle mass and are prone to develop muscular atrophy or nerve damage following IM injections. This route should therefore be avoided in mice. If drugs must be administered via the IM route, minimal injection volumes (0.05 ml) should be used. Use 27-30 gauge needle. RATS ANESTHESIA DOSE (mg/kg) & ROUTE Isoflurane (Forane®) To effect Inhalation; precision vaporizer required; adequate ventilation or scavenging system essential 30-40 IV 40-60 min. duration Halothane (Fluothane®) COMMENTS Enflurane (Ethrane®) Pentobarbital 40-60 IP Thiopental 20-40 IV 5-10 min. duration 40 IP Ketamine + Xylazine 60-90 + 6-9 IP 30-45 min duration; supplement with 1/3 of ketamine dose only Ketamine + Medetomidine 75 + 0.5 IP, SC Urethane 1000-1500 IP Prolonged (12 hr +) anesthesia; terminal procedure only; carcinogenic + mutagenic Chloral Hydrate 300-400 IP Use 5% solution; anesthetic dose approaches LD50 Inactin 80-100 IP Tiletamine-Zolazepam (Telazol®) 20-40 IP Concentration of reconstituted mixture is 100 mg/ml Methohexital 40 IP 1% solution; 20 min. duration Equithesin 3 ml/kg 40 min. duration; fresh mixture req. 10 SC 3 hr ANALGESIA Morphine 14 Meperidine 20 SC 3 hr Imipramine 10 SC 12 hr Butorphanol (Torbutrol® 0.5mg/ml) 10-12 SC 3 hr Buprenorphine (Buprenex®) 0.02-0.05 SC 6-12 hr Carprofen 5 SC 12-24 hr Medetomidine 30-100 µg/kg SC Reverse w/atipamezole; 1 µg/kg SC, IP, or IV Ketamine 50-100 IM, IP SEDATION NOTES Small muscle mass: Rats have a relatively small total muscle mass and are prone to develop muscular atrophy or nerve damage following IM injections. This route should be minimized in rats. If drugs must be administered via the IM route, minimal injection volumes (0.3 ml) should be used. Use a 25 gauge needle (or smaller). HAMSTERS ANESTHESIA Isoflurane (Forane®) DOSE (mg/kg) & ROUTE COMMENTS To effect Inhalation; precision vaporizer required; adequate ventilation or scavenging system essential Pentobarbital 70-90 IP 60-75 min. duration Ketamine + Xylazine 80-100 + 7-10 IP Ketamine + Medetomidine 100 + 0.25 IP Tiletamine + Zolazepam 20-30 IP (Telazol®) + Xylazine +10 IP Urethane 1500 IP Halothane (Fluothane®) Enflurane (Ethrane®) 10-30 min. duration 6 hr 15 Urethane (50%) + aChloralose (10%) + Pentobarbital 380 IP 38 IP 26 IP Extend anesthesia (every 2 hr) w/Urethane (135 mg) + Chlorase (14 mg) IP Carcinogenic + mutagenic ANALGESIA Morphine 10 SC 3 hr Meperidine 20 SC 3 hr Buprenorphine (Buprenex®) 0.05-0.5 SC 8-12 hr SEDATION Chlorpromazine 0.5 IM Ketamine 40-80 IP GUINEA PIGS DOSE (mg/kg) & ROUTE ANESTHESIA Isoflurane (Forane®) COMMENTS To effect Inhalation; precision vaporizer required; adequate ventilation or scavenging system essential Pentobarbital 15-40 IP 60 min. duration Ketamine + Xylazine 40-100 + 4-5 IM 60 min. duration Ketamine + Medetomidine 40 + 0.5 IP Moderate anesthesia a-Chloralose (1%) + Urethane (40%), in a mixture 8.0 ml/kg IP >2 hr duration Morphine 10 SC 4 hr Meperidine 20 IM, SC 2-3 hr Buprenorphine 0.05 SC 8-12 hr Halothane (Fluothane®) Enflurane (Ethrane®) 7:1 ANALGESIA 16 SEDATION Ketamine 40 IM Chlorpromazine 0.2 SC Diazepam 2.5-5.0 IP Xylazine 5-40 IP RABBITS ANESTHESIA Isoflurane (Forane®) DOSE (mg/kg) & ROUTE COMMENTS To effect Inhalation; precision vaporizer required; scavenging system essential. Less anesthetic is necessary, and a more even plane of anesthesia can be achieved if a preanesthetic such as butorphanol/acepromazine is used. Pentobarbital 30 IV Very narrow margin between effective and lethal dose Ketamine + Xylazine 35-50 + 510 IM 45 min., minor procedures Ketamine + Medetomidine 25 + 0.5 IM a-Chloralose 80-120 IV Urethane 1000 IV, IP Carcinogenic, acute procedures only Equithesin 1-3 ml/kg Fresh solutions only Morphine 2-5 SC 3 hr Meperidine 10 SC 2-3 hr Buprenorphine 0.01-0.05 SC 6-12 hr Halothane (Fluothane®) Enflurane (Ethrane®) Supplement with 1/3 the original dose of Ketamine + Xylazine ANALGESIA 17 Butorphanol 0.1-0.5 SC, IM, IV 4 hr Carprofen 1.5 SC 12-24 hr Ketoprofen 1 SC, IM 24 hr SEDATION Butorphanol + Acepromazine 1 + 1 IM Chlorpromazine 25-100 IM Acepromazine .75-1.0 IM Diazepam 5-10 IM Ketamine 30 IM Xylazine 3-5 IM, SC NOTES: Anesthetic depth: Adequate anesthesia for surgery can be very difficult to obtain in rabbits, especially when barbiturates are used. Rabbits are prone to develop respiratory depression and edema when anesthetized. Atropinase: Atropine is frequently administered to anesthetized animals to reduce oral and respiratory secretions and to support heart rate. Many rabbits (up to 50%) have circulating atropinase and thus may demonstrate a reduced duration of effectiveness of this drug. Normal values: temperature 38.5-39.0oC (101.3-102.2oF); heart rate 130-300/min; respiration rate 3060/min. DOGS ANESTHESIA Isoflurane (Forane®) DOSE (mg/kg) & ROUTE COMMENTS To effect Inhalation; precision vaporizer required; scavenging system essential. Less anesthetic is necessary, and a more even plane of anesthesia can be achieved if a preanesthetic such as butorphanol/acepromazine or buprenorphine/acepromazine is used. 20-30 IV Give ½ as a bolus; the rest to effect; 30-45 min. duration Halothane (Fluothane®) Enflurane (Ethrane®) Pentobarbital 18 Thiopental 8-12 IV Short acting; <15 min Chloralose 80-110 IV 6-10 hr; premedicate w/morphine procedures Ketamine + Diazepam 10 + 0.5 IV 5.5 + 0.3 IV 5 mg/kg; terminal Minor procedures; premedicate with anticholinergic ?? Good for induction of anesthesia after a pre-anesthetic is given, and then maintenance of anesthesia with a gas anesthetic such as isoflurane. Ketamine + Midazolam 10 + 0.5 IV Minor procedures; premedicate with anticholinergic ?? Tiletamine + Zolazepam 6-8 IM 1 hr. surgical anesthesia 0.5 IM (Telazol®) + Xylazine 0.2 IM +Butorphanol ANALGESIA Meperidine 2-10 SC, IM 2-3 hr Morphine 0.25-5 IM, SC 4-6 hr Butorphanol (Torbutrol® 0.5 mg/ml) 0.2-0.4 IM, SC 2-5 hr Buprenorphine 0.01-0.02 SC 8-12 hr Carprofen 2.2 PO, 5 SC 12 hr Ketoprofen 2 SC, IIM 24 hr Fentanyl patch See table Place 12 hours prior to painful procedure. Do not apply heat to patch area as this will stimulate a large release of the fentanyl (watch heating pads). 19 Weight of Dog < 5 kg 5-10 kg 10-20 kg 20-30 kg > 30 kg Fentanyl patch size 1/2 of a 25 mcg/hr 25 mcg/hr 50 mcg/hr 75 mcg/hr 100 mcg/hr Duration 72 hrs 72 hr 72 hrs 72 hrs 72 hrs ?? See above: discuss these items with a DLAR veterinarian. SEDATION 0.2-0.4 SC, IM, IV + Butorphanol + Acepromazine 0.02-0.05 SC, IM, IV Buprenorphine + Acepromazine 0.07 SC, IM + 0.0009 SC, IM Xylazine 0.5-1.0 IM Chlorpromazine 1-6 IM, SC Acepromazine 0.05-0.1 IM, SC Maximum of 3 mg total NOTES: Food: Prior to elective surgery, food should be withheld for 12 hrs. Normal values: temperature 37.5-39oC (99.5-102.2oF); heart rate 70-120/min, respiratory rate 15-25/min. Anticholinergic medication is recommended in anesthetized dogs to support the heart rate and reduce bronchial secretions. Recommended agents include atropine (0.02-0.04 mg/kg SC, IM) or glycopyrrolate (0.02 mg/kg IM, SC). Note that the above treatment has become controversial in the field of veterinary medicine, and unless a documented bradycardia is present, anticholinergics are not necessary and can cause a profound tachycardia. Anticholinergic premedication is not currently recommended by veterinary anesthesiologists. Atropine is good for quick IV use if bradycardia is present, but it doesn't last long. If a known vagal stimulation is expected during a surgical procedure, then glycopyrrolate is a good/better anticholinergic premedication than atropine. It will not produce as profound a tachycardia as with atropine, and it will last longer. It does however need to be given at least 30 minutes prior to vagal stimulation. Discuss the need for this treatment with a DLAR veterinarian. CATS ANESTHESIA Isoflurane (Forane®) DOSE (mg/kg) & ROUTE To effect COMMENTS Inhalation; precision vaporizer required; scavenging system essential. Less anesthetic is necessary, and a more even plane of anesthesia can be achieved if a pre- 20 anesthetic such as butorphanol/acepromazine is used. Halothane (Fluothane®) Enflurane (Ethrane®) Pentobarbital 20-30 IV Give ½ as a bolus; the rest to effect; 30-45 min. duration Ketamine + Diazepam 10 + 0.5 IV Minor procedures; premedicate with anticholinergic ?? 5.5 + 0.3 IV Good for induction of anesthesia after a pre-anesthetic is given, and then maintenance of anesthesia with a gas anesthetic such as isoflurane Ketamine + Medetomidine 7 + 0.08 IM Minor procedures; 45 min. duration ANALGESIA Morphine 0.1 IM, SC Meperidine 2-10 IM, SC 4 hr.; mania and excitation with overdose Buprenorphine 0.005-0.01 SC, IM 12 hr. Oxymorphone 0.05-0.15 IM, SC, or IV 3-5 hr. Minimal respiratory depression Carprofen 4 SC, IV 24 hr Ketoprofen 1 SC, IM, IV 24 hr Fentanyl patch See table Place 8 hours prior to painful procedure. Do not apply heat to patch area as this will stimulate a large release of the fentanyl (watch heating pads). Weight of Cat Fentanyl patch size Duration < 2.5 kg 1/2 of a 25 mcg/hr 5 days > 2.5 kg 25 mcg/hr 5 days ?? See above: discuss these items with a DLAR veterinarian. 21 SEDATION 0.1-0.4 SC, IM, IV + Butorphanol + Acepromazine Ketamine Acepromazine Chlorpromazine Midazolam Diazepam Xylazine 0.02-0.05 SC, IM, IV 10-20 IM 0.05-0.1 IM, SC 1-2 IM 0.2-0.4 IM 0.2-0.4 IV, IM 0.4-0.9 SC, IM NOTES: Acetaminophen (Tylenol) is extremely toxic in cats and should not be used in this species. Cats are also very sensitive to the toxic effects of aspirin, and fatalities are frequently reported. Although aspirin can be used in cats, other agents should be used if possible. Food: Prior to elective surgery, food should be withheld for 12 hrs. Normal values: temperature 38.0-39.5oC (100.4-103.1oF); heart rate 110-140/min; respiration rate, 2030/min. Anticholinergic medication is recommended in anesthetized cats to support the heart rate and reduce bronchial secretions. Recommended agents include atropine (0.02-0.04 mg/kg SC, IM) or glycopyrrolate (0.02 mg/kg IM or SC). Note that the above treatment has become controversial in the field of veterinary medicine, and unless a documented bradycardia is present, anticholinergics are not necessary and can cause a profound tachycardia. Anticholinergic premedication is not currently recommended by veterinary anesthesiologists. Atropine is good for quick IV use if bradycardia is present, but it doesn't last long. If a known vagal stimulation is expected during a surgical procedure, then glycopyrrolate is a good/better anticholinergic premedication than atropine. It will not produce as profound a tachycardia as with atropine, and it will last longer. It does however need to be given at least 30 minutes prior to vagal stimulation. Discuss the need for this treatment with a DLAR veterinarian. NON-HUMAN PRIMATES ANESTHESIA Enflurane (Ethrane®) DOSE (mg/kg) & ROUTE COMMENTS To effect Inhalation; precision vaporizer required; scavenging system essential 2-6 + 0.03-0.06 60 min. duration Halothane (Fluothane®) Isoflurane (Forane®) Ketamine + 22 Medetomidine IM Ketamine + Xylazine 10 + 0.25 IM 45 min. duration Ketamine + Diazepam 10 + 0.2-0.35 IM Restraint + muscle relaxation Telazol® 4-6 IM ANALGESIA Morphine 1-2 SC 4 hr Meperidine 2-4 IM 3-4 hr Buprenorphine 0.01 IM 6-8 hr SEDATION Ketamine 5-20 IM Acepromazine 1-5 IM, SC Chlorpromazine 5-10 SC, IM ANTICHOLINERGIC Atropine 0.02-.05 IM, SC NOTES: Normal values (Rhesus monkey): temperature 37.0-39.1oC (99.0-102.5oF); heart rate (sedated) 120-180/min; respiration rate (sedated) 32-50/min. PIGS ANESTHESIA Enflurane (Ethrane®) DOSE (mg/kg) & ROUTE COMMENTS To effect Inhalation; precision vaporizer required; scavenging system essential Ketamine + Xylazine 20 + 2 IM 20 min.; minor procedures Ketamine + Acepromazine 33 + 1.1 IM Pentobarbital 5-15 IV Halothane (Fluothane®) Isoflurane (Forane®) Administer to effect 23 Ketamine + Telazol® 2.2 + 4.4 IM 20-30 min. duration Telazol® + Xylazine 2.0-8.8 + 2.2 IM 20 min. duration; may produce cardiopulmonary depression Ketamine + Medetomidine 10 + 0.08 IM Immobilization; light anesthesia ANALGESIA Aspirin 10 PO 4-6 hr.; use enteric-coated tablet Meperidine 4-10 IM 4 hr. Phenylbutazone 10-20 PO 12 hr. For musculoskeletal pain Buprenorphine 0.005-0.01 IM 12 hr. SEDATION Acetylpromazine 0.11-1.1 SC, IM Chlorpromazine 0.5-4 IM, SC Diazepam 0.5-10 IM Azaperone (Stresnil®) 2-8 Usually combined w/other agents NOTES: Malignant hyperthermia: Malignant hyperthermia (MH) is commonly reported in swine. The first cardinal clinical sign of MH is an elevation in end-tidal CO2. MH characterized by the sudden onset of muscle rigidity, tachypnea, tachycardia and hyperthermia (rectal temperatures up to 108oF), followed by dyspnea, cardiac arrhythmias, apnea and death. Anesthesia (particularly with halothane isoflurane, or ethrane), restraint, stress and excitement have all been reported to trigger this condition. Anesthetized swine should be monitored closely for the development of hyperthermia. Emergency measures include cessation of the anesthetic, cooling the body with ice water, and the IV administration of sodium bicarbonate and the muscle relaxant dantrolene (2-10 mg/kg). Food: Prior to elective surgery, withhold food for 12 hrs. Normal values: temperature 38.0-40.0oC (100.4-104.0oF); heart rate 60-120/min; respiration rate 10-12/min. Anticholinergic: Glycopyrrolate (0.004-0.01 mg/kg IM) or atropine (0.05 mg/kg IM ).







