Child and Adolescent Neurology
advertisement

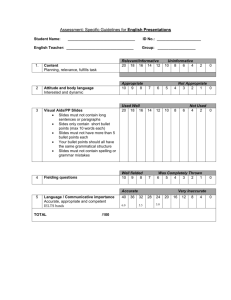
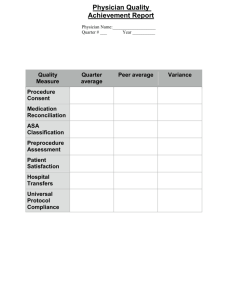
Office Use Ht: cm ( %) Child and Adolescent Neurology Wheelchair / Arm Span ________ cm Patient Information Questionnaire Wt: Kg ( %) FOC: BP: cm ( / %) Pulse: /min. Temp NKDA/Allergies: Staff Initials: _________________ Today’s Date: / / Please complete the following items. If in doubt, leave blank. Return this form with a recent photo of your child to the front desk. Patient Name: Nickname: Primary Care Physician: Referring Physician: Problem for which your child is being seen? Age DOB / Yr. / Mo. What other concerns do you have? Other current medical problems? (Allergies, Infections, Etc.): Preferred Pharmacy: ___________ Pharmacy Phone Number: ____________ Who is completing this form?______________________________ Relationship to Patient______________________ Revised 3/13/15 1 Pregnancy History Maternal age at delivery: years Illnesses during pregnancy, please list: Medications or drugs used, please list: Check if any of the following applies to you: Alcohol Incomplete pregnancies? If yes, how many? Other children: Prescription Drugs Recreational Drugs Girls Boys Birth History Hospital: Place of Birth, City: Duration of Pregnancy Length of Labor Check type of delivery: Birth weight: Apgar Scores: 1 min.: Vaginal hours C-Section Length: 5 mins.: Due Date Forceps State: Vacuum Head size: Neonatal History Abnormalities noted at birth? Breathe or Cry Immediately? Feeding: breast or bottle Special care given in the hospital? How long was the hospital stay? Developmental History Gross Motor Fine Motor Rolled over Months Reached ______ Sat alone Transferred ______ Pulled to stand _______ Ate w/ fingers ______ Crawled _______ Used fork/spoon ______ Cruised Undressed ______ Walked alone _______ Dressed ______ Ran well _______ Tied shoes ______ Pedaled tricycle _______ Caught a ball ______ Pedaled bicycle Scribbled ______ Left/Right handed Pincer grasp ______ Expressive Language, Self Help MaMa/DaDa ______ Laughed ______ Babbled ______ Single words ______ 2 or more words ______ Name, age, gender ______ Learned colors ______ Potty Trained ______ Told Story ______ School History Current School: Present teacher’s name: Special classes? __ If yes, what type: Repeated grades? __ If yes, which grades, and at which schools? Classroom performance? Clubs, activities: Special problems while attending school: Receptive Language Recognized Mom ______ Turned to voice ______ Understood “no” ______ 1-step commands ______ 2-step commands ______ Grade: Current Medications (Name of medication & dose; prescription or non-prescription) 1.______________________________________ 2.______________________________________ 3.______________________________________ 4.______________________________________ 5.______________________________________ 6.____________________________________ 7.____________________________________ 8.____________________________________ 9.____________________________________ 10.___________________________________ 2 Past Medical History Birthmarks Yes Allergies: Yes Asthma Yes Bedwetting Yes Clumsiness Yes Constipation/Diarrhea Yes Headaches Yes Unsuccessful past medication(s): No No No No No No No Head Injury Yes Hearing Problems Yes Heart Problems Yes Orthopedic problems Yes Reactions to Immunizations Yes Speech Problems Yes Seizures/Convulsions Yes Unsuccessful past medication(s): No No No No Vision Problems No Comments No No No Yes For girls, age of first menstrual period: Problems: Hospitalizations or Operations Regular? Age Where 1. 2. 3. Is your child receiving? Physical Therapy? Occupational Therapy? Speech Therapy? Where? Where? Where? Behavior Problems: Short Attention Span Poor Concentration Sleep Problems Eating Problems Depressed Compulsive Oppositional Previous Testing Psychological Testing EEG CT Scan MRI Metabolic Chromosomes Fragile X Hyperactive Restless Inattention Destructive Angry Fearless Head Banging / / / / / / / Distractible Fidgety Aggressive Self-injurious Anxious Defiant Rocking Date Impulsive Talks out Violent Fire Setting Obsessive Dangerous Lacks Remorse Results / / / / / / / 3 Enuresis Encopresis Temper Tantrums Noncompliant Sibling Problems Peer Problems Excessive crying or upset Pica Lies Cruel to Animals Steals Truant Family History Child lives with: Biological Father: Highest Grade Completed: Medical Problems: Biological Mother: Highest Grade Completed: Medical Problems: Other family members on medications? Occupation: Occupation: Height Age Height Age If yes, list medication and family member Please identify any family members with any of the following: Cancer Poor Coordination Cerebral Palsy Psychiatric Disorder ADD/ADHD Panic Attacks Bipolar________________________________ Other:_________ Stroke Epilepsy Headaches Hearing Loss Depression Mental Retardation Seizures Migraine Vision Loss Tic or Movement Disorder Anxiety Disorder Sleep Problems ______________ Obsessive-compulsive Disorder_________________ ___________________________________ For Physician Usage 4 For Physician Usage General Exam: Appearance: Skin: Resp/Chest: Extremities: Edema/Pulses Abdomen EENT Neck Eyes Heart GU Back Mental Status: Cranial Nerves I, III-XII 2nd Cranial Nerve Fundus:___________ Muscle Tone Bulk Strength DTRs (see above) Sensation Cerebellum / Coordination: Gait: Neurologic Exam: Fields Color Acuity: OS OD Tests Ordered/Reviewed: Assessment: Plan: Problem Focused Expanded Problem Focused Detailed Comprehensive = 1 – 5 elements identified by a bullet = At least 6 elements identified by a bullet = At least 12 elements identified by a bullet = Perform all elements by a bullet and document at least 2 elements identified by a bullet from each of nine areas/systems Counseling: min. Level 2 = 10 min; 1 = 5 min; Total Visit: 3 = 15 min; min. (Document time and summarize if > 50% of visit) 4 = 25 min; 5 = 40 min; Signature Date 5 Child and Adolescent Neurology Date of Service Patient Label or MRN, Patient Name, DOB, REVIEW OF SYSTEMS Please answer the following questions about your child’s present health YES NO COMMENTS Eyes Head Ears, Nose & Throat Cardiovascular Respiratory Gastrointestinal Genitourinary Musculoskeletal Skin Neurological Psychiatric Immunologic Sleep Tests Blurring or Loss of vision? Eye surgery Headaches? Head injuries? Hearing difficulties? Ear surgery? Ear infections? Chest pain? Heart palpitations? Heart murmur? Rheumatic fever or Lyme disease? Swollen ankles Sore throats? Nosebleeds, runny nose, sinus infections Problems breathing through nose? Spitting up blood Any problems with teeth, gums, or sores in the mouth? Problems with shortness of breath? Chronic cough or wheezing? History of pneumonia? Exposure to TB? Chest X-rays? Does your child eat poorly? Chronic diarrhea? Recent weight change? Frequent vomiting? Chronic constipation? Problems urinating? Blood in the urine? Urinary tract infections? Discharge from the penis or vagina? Has your child’s menstrual cycle started? Are her periods painful or irregular? Is she using birth control? Muscle or joints that are swollen? Weakness? Cramps? Any body parts that do not move freely? Rashes? Skin markings or birth marks? Learning problems? Attention problems? Failing grades or classes? Loss of skill or function? Moody? Anxious? Antisocial? Angry? Obsessive? Compulsive? Sad? Depressed? Sleep problems? Are your child’s immunizations up to date? Sleep walking? Night Terrors? Bedwetting? Has your child had any tests done since their last visit? If so, please list. Learning readiness/barriers identified per protocol: Staff Initials:__________________ Reviewed and discussed with parent/legal guardian _________________________________________Physician _________________________________________Date 6