The Reducing Hospital Mortality “Diagnostic”
advertisement
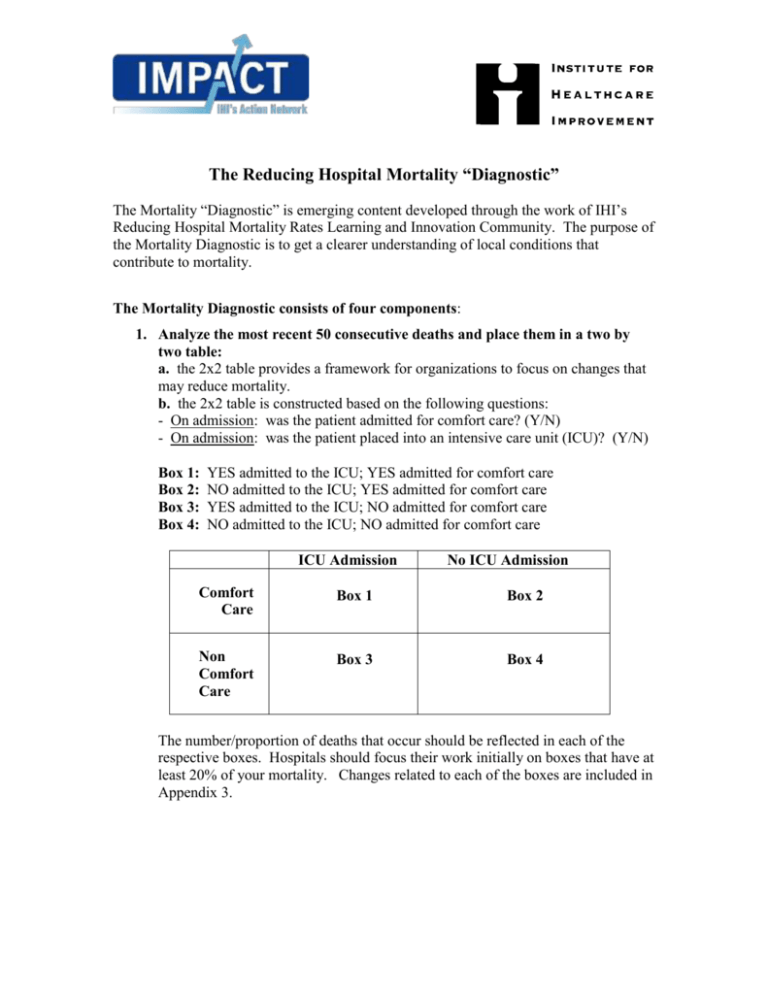
The Reducing Hospital Mortality “Diagnostic” The Mortality “Diagnostic” is emerging content developed through the work of IHI’s Reducing Hospital Mortality Rates Learning and Innovation Community. The purpose of the Mortality Diagnostic is to get a clearer understanding of local conditions that contribute to mortality. The Mortality Diagnostic consists of four components: 1. Analyze the most recent 50 consecutive deaths and place them in a two by two table: a. the 2x2 table provides a framework for organizations to focus on changes that may reduce mortality. b. the 2x2 table is constructed based on the following questions: - On admission: was the patient admitted for comfort care? (Y/N) - On admission: was the patient placed into an intensive care unit (ICU)? (Y/N) Box 1: Box 2: Box 3: Box 4: YES admitted to the ICU; YES admitted for comfort care NO admitted to the ICU; YES admitted for comfort care YES admitted to the ICU; NO admitted for comfort care NO admitted to the ICU; NO admitted for comfort care ICU Admission No ICU Admission Comfort Care Box 1 Box 2 Non Comfort Care Box 3 Box 4 The number/proportion of deaths that occur should be reflected in each of the respective boxes. Hospitals should focus their work initially on boxes that have at least 20% of your mortality. Changes related to each of the boxes are included in Appendix 3. 2. Review the deaths in Box 3 and Box 4 to determine if there was evidence of failure to recognize, plan, communicate during the entire hospitalization: - failure to recognize: any situation in which a patient has died and there was evidence that an intervention could have been made anytime prior to the patient’s death (in this hospitalization) that potentially would have impacted the patient’s outcome. Example criteria that could be considered in reviewing the medical record include: staff was worried, change in heart rate, change in respiratory rate, change in blood pressure, change in O2 saturation or change in consciousness or neurological status that was not responded to. - failure to plan, such as: diagnosis, treatment, or calling a rescue team - failure to communicate: Patient to staff, clinician to clinician, inadequate documentation, inadequate supervisor, leadership (no quarterback for the team), etc. 3. Evaluate the first 20 deaths in Box 3 and Box 4 to determine if there is any evidence of adverse events, using the Global Trigger Tool. 4. Evaluate ALL deaths in Box 3 and Box 4 to assess the estimated impact of our care on mortality: *As you review the deaths in Box 3 and 4, ask yourself the questions honestly (focusing on learning, not judgment): Was perfect care rendered? If perfect care wasn’t rendered, could the outcome of death have been prevented if the care had been better? - What number of deaths could have been prevented? Institute for Healthcare Improvement Reducing Hospital Mortality Rates Learning and Innovation Community: The Mortality “Diagnostic” (updated August 2006) 2 Appendix 1: Initial Screening Tool – Mortality Analysis INITIAL SCREENING TOOL MORTALITY ANALYSIS BOX Patient ID Med Record # Admitting Unit Admit Date Unit When Death Occurred Discharge Date Patient admitted from: Home Skilled Care Transferring hospital Other Admitting Diagnosis (without looking at discharge diagnosis) Principal ICD-9 Code and Diagnosis at Discharge Did the admission and discharge diagnosis match? Yes No Was patient admitted for “comfort care”? Yes No Was patient admitted to the ICU? Yes No Was the patient transferred to a higher level of care? (at any point during their stay) Yes No Institute for Healthcare Improvement Reducing Hospital Mortality Rates Learning and Innovation Community: The Mortality “Diagnostic” (updated August 2006) 3 Appendix 2: Mortality Analysis Tool MORTALITY ANALYSIS In the work on mortality, we have encouraged all hospitals to develop measurement/learning systems for mortality analysis. All hospitals have a peer review system that looks at mortality but those systems have focused on measurement for judgment. To be successful, you need to have something more. We have looked at the work of a variety of organization, the work of Charles Vincent and our own work and have come up with a list of the main categories that should be considered in a mortality analysis. The following worksheet should be completed for each death in Box 3 and Box 4 to determine if there is evidence of: Failure to recognize, plan and/or communicate. The goal of this tool is not to provide an exercise in categorization but an opportunity for you to more fully understand your own hospital. Failure to Recognize: any situation in which a patient has died and there was evidence that an intervention could have been made anytime prior to the patient’s death (in this hospitalization) that potentially would have impacted the patient’s outcome. Example criteria that could be considered in reviewing the medical record include: staff was worried, change in heart rate, change in respiratory rate, change in blood pressure, change in O2 saturation or change in consciousness or neurological status that was not responded to. Failure to Plan, such as: diagnosis, treatment, or calling a rescue team Failure to Communicate, such as: Patient to staff, clinician to clinician, inadequate documentation, inadequate supervisor, leadership (no quarterback for the team), etc. Failure to Recognize Comments: Failure to Plan Comments: Failure to Communicate Comments: Institute for Healthcare Improvement Reducing Hospital Mortality Rates Learning and Innovation Community: The Mortality “Diagnostic” (updated August 2006) 4 Appendix 3: Changes related to the 2 x 2 table Hospitals should focus their work initially on boxes that have at least 20% of your mortality. COMFORT CARE ONLY Box 1 changes: Clarity of ICU admission/transfer criteria Box 2 changes: NOT COMFORT CARE ONLY Box 3 changes: Glycemic Control Sepsis Intervention Ventilator Bundle Multidisciplinary rounds in the ICU/Shared Goal Sheet Communication & Handoffs Central Line Bundle Appropriate tidal volume for ARDS patients* Advanced Directives Alternatives to hospital care at the end of life Palliative Care Team Community outreach for Advanced Directives Box 4 changes: Rapid Response Team Communication & Handoffs (tools, such as SBAR) Early Warning System Multidisciplinary rounds outside the ICU Glycemic Control outside the ICU Central line bundle outside the ICU Advanced training for Rapid Response Team – incorporating Sepsis & early warning* * Change ideas marked with * are still consider early work. Institute for Healthcare Improvement Reducing Hospital Mortality Rates Learning and Innovation Community: The Mortality “Diagnostic” (updated August 2006) 5