Pulse Oximetry
advertisement

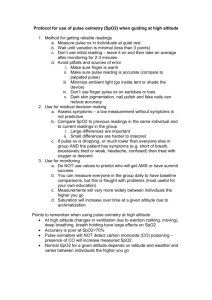
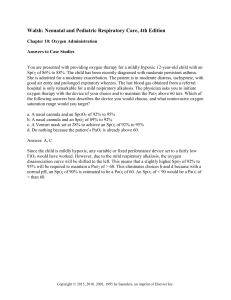
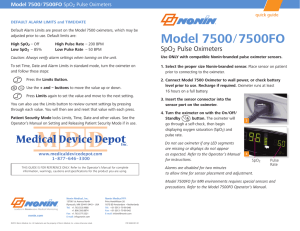
MU PT 7890 Case Management I Pulse Oximetery Pulse Oximetry (SpO2) is an inferred measurement of tissue perfusion. It is less costly, non invasive, and more convenient than an arterial “stick” (ABG), but it is less accurate than an ABG reading of oxyhemoblogin saturation (SaO2). Nomenclature: Blood draw / ABG value = SaO2 Pulse Oximeter = SpO2 For cellular respiration to occur: Adequate Ventilatory pump function (central control, unobstructed airways, and proper lung and chest wall compliance / flexibility) Adequate diffusion of O2 & CO2 across the alveolar-capillary membrane (DLCO) Adequate Cardiac pump function + vascular delivery system + healthy vascular bed in tissue Adequate Blood components: Adequate # hemoglobin / RBC [normal Male:14-16.5; Femal:12-15] [anemia: < 8] Adequate # RBC / volume of whole blood Adequate amount of iron contained in Hgb molecules (Hematocrit) Adequate # Hgb molecules that are carrying their full capacity / saturation of O2 Instructions from the Onyx II Pulse Oximeter manual: Fingernail side up Keep at heart or chest level Observe 4 seconds of green indicated pulse reading before taking a number If continues to blink yellow or red, try another finger (without fingernail polish) Wipe inside finger surfaces with alcohol, or if needed, a 10% bleach solution. Minimize movement Potential causes for an inaccurate reading: Motion artifact (keep arm still) External bright light source (and possibly from strong radio frequency source) Potential causes for a TRUE low reading: Tissue hypoxia (chronic or exercise induced) Age (see table) Potential causes for a FALSE low reading: poor perfusion (cold fingers, arterial insufficiency) fingernail polish callouses increased sweaty or oily hands arrhythmia Raynaud’s Potential causes for a misleading high reading: Anemia: decreased # of Hgb molecules in each RBC, but the ones that are there may have all 4 available sites bound with O2, so the PulsOx reads it as normal O2 saturation Carbon monoxide poisoning (PulsOx can’t distinguish between O2 and CO) Nonin Onyx II ®, Pulse Oximeter accuracy for readings in the 70-100 SpO2 range is + 2 digits Low reading range Medicare xxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxx Hi Kyle, More thoughts about Puls Oximetry, SpO2 It is an inferred measurement of tissue perfusion. age 30 - 95-97% age 50 - 93-95 age 70 - 92-93 age 90 - 90-92 Therapeutically want to keep it above 85-88% (supplemental oxygen can be involved at this level). Consider the normal 30y.o.: if they are exercising at 13/20 on the Borg, their SpO2 values should stay steady. If they exercise at a higher Borg, they will eventually exceed their ventilatory threshold and go anaerobic, with lactic acid production, etc. At this point, tissue perfusion would drop, so a drop in SpO2 could occur. For a frail person, (who may have pulmonary deficits in addition to decreased cardiac reserve) they will "spend their reserve" earlier, but theoretically if they are no higher than a Borg 13/20 their muscle tissue will continue to be perfused and SpO2 steady. With multi system involvement, I suspect it would be prone to dropping, even at lower Borg levels, but don't have a lot of clinical experience to back that up. Evan Also, when ventilatory threshold is reached, PaCO2 rises, (PaO2 falls) and this causes a shift to the right of the Oxyhemoglobin dissociation curve. In other words, as PaO2 falls, Hgb gives up more of its O2 to compensate for homeostasis. Also the PaCO2 circulates to the respiratory centers in the medulla which stimulate the muscles of respiration to work harder (unsure if these have a direct catecholamine / neurohumoral effect on the heart rate)