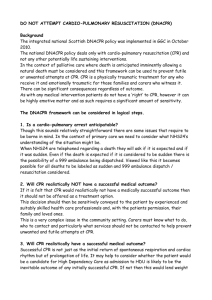
Do Not Attempt Resuscitation (DNAR) Evaluation
advertisement
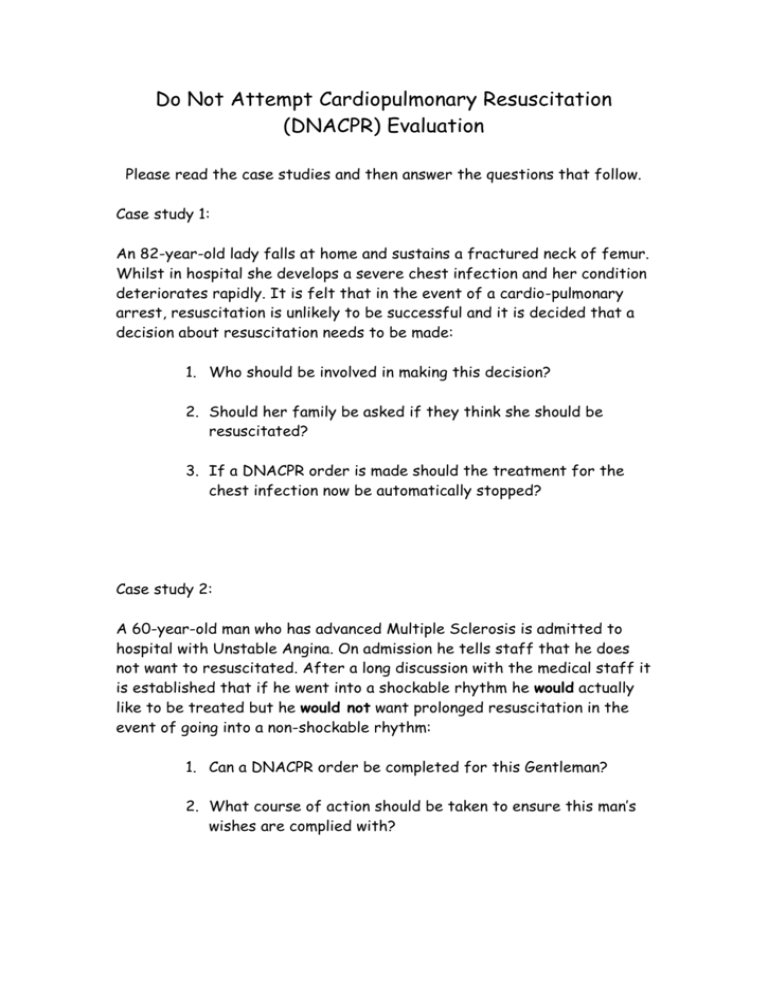
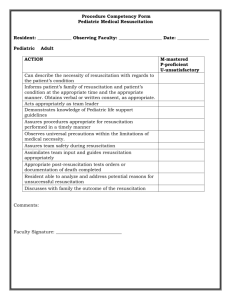
Do Not Attempt Cardiopulmonary Resuscitation (DNACPR) Evaluation Please read the case studies and then answer the questions that follow. Case study 1: An 82-year-old lady falls at home and sustains a fractured neck of femur. Whilst in hospital she develops a severe chest infection and her condition deteriorates rapidly. It is felt that in the event of a cardio-pulmonary arrest, resuscitation is unlikely to be successful and it is decided that a decision about resuscitation needs to be made: 1. Who should be involved in making this decision? 2. Should her family be asked if they think she should be resuscitated? 3. If a DNACPR order is made should the treatment for the chest infection now be automatically stopped? Case study 2: A 60-year-old man who has advanced Multiple Sclerosis is admitted to hospital with Unstable Angina. On admission he tells staff that he does not want to resuscitated. After a long discussion with the medical staff it is established that if he went into a shockable rhythm he would actually like to be treated but he would not want prolonged resuscitation in the event of going into a non-shockable rhythm: 1. Can a DNACPR order be completed for this Gentleman? 2. What course of action should be taken to ensure this man’s wishes are complied with? Case Study 3: A 30-year-old man is brought to the Emergency Department after breaking his leg play rugby: 1. Should he be asked if he wants to be resuscitated? 2. In the unlikely event of him having a cardiac arrest what should you do? Case Study 4: A 79-year-old lady with moderate dementia is admitted to hospital having a heart attack. It is decided that a decision about resuscitation needs to be made. Although she has a poor mental state, she is still fairly physically active and it is felt that CPR is likely to be successful: 1. Who should decide if she is to be resuscitated? 2. Who should be included in this discussion? 3. Do the relatives legally have a say in the final decision? Case Study 5: A 56 year old man with lung cancer, bone, liver and brain mets is admitted to hospital severely jaundiced and agitated. His family wanted him to die at home but couldn’t cope with the agitation. On the ward round it is acknowledged that he is dying and is for comfort measures only. While he is on the commode he suddenly collapses. The staff nurse then realises that the doctor has forgotten to fill out the DNACPR form. 1. Should the nurse call the resuscitation team? Answers: Case study 1: 1. The whole team including relevant others should be involved with the discussion but the final decision lies with the Consultant/GP. 2. Relatives should not be burdened with making a DNACPR decision but they may have useful information that helps to reach the decision. 3. A DNACPR order only refers to cardio-pulmonary resuscitation and not to other treatments. Case study 2: 1. A DNACPR order cannot be completed on this gentleman. 2. He should be encouraged to have an advanced directive completed with all his preferred treatment options. In the meantime the discussion and treatment plan should be well documented and communicated to all staff. Case Study 3: 1. Cardiac arrest cannot be anticipated so he should not be asked. 2. Resuscitate. Case study 4: 1. The most senior member of the medical team at that time. 2. All staff and any relevant others. 3. Only any officially appointed proxy’s or welfare guardian’s legally have a say – not relatives. Case study 5 1. No. If no DNACPR documentation exists CPR should be attempted unless the patient is in the terminal phase of an illness. An experienced nurse can make this judgement in an emergency.