Pharmacology Objectives 13
advertisement

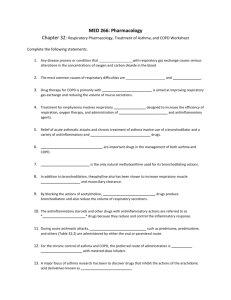
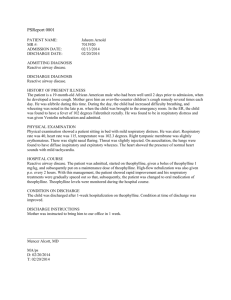
Pharmacology Lecture 13 Pulmonary Drugs “Pharmacologic Therapy of Obstructive Lung Disease” 1) Describe the major categories of drugs used to treat obstructive lung diseases. Bronchodilators Beta-adrenergic agonists – activate β2-adrenergic receptors in airway smooth muscle and produce functional antagonism of bronchoconstriction in airways of all sizes. Anticholinergics - produce bronchodilation by directly antagonizing the effects of acetylcholine on the muscarinic receptors in airway smooth muscle. Theophylline - the mechanism of action remains unclear. Pharmacologic effects include improved diaphragmatic contraction, smooth muscle relaxation, and increased mucociliary clearance. Leukotriene modifiers - prevent the synthesis or action of cysteinyl leukotrienes, by either blocking at the receptor or blocking the formation of leukotrienes by inhibiting 5-lipooxygenase or the 5-lipooxygenase activating protein. Anti-inflammatory Corticosteroids - enter cells, primarily by diffusion, and bind to glucocorticoid receptors (GRs), which are predominantly localized to the cytoplasm of target cells. (Cromolyn/Nedocromil) - mechanism is not well understood, these agents prevent the release of preformed mediators and arachidonic acid metabolites from a number of cells including mast cells, T-lymphocytes, eosinophils and macrophages. 2) Be able to distinguish the mechanisms of action for beta-adrenergic agonist and anticholinergic bronchodilators. Beta-adrenergic agonist - act by activating β2-adrenergic receptors, which activate adenylyl cyclase, resulting in an increase in cyclic AMP, activation of protein kinase A, and relaxation of airway smooth muscle through the cyclic AMP/protein kinase A phosphorylnation cascade. Anticholinergic bronchodilators - cholinergic control of airway smooth muscle tone is mediated by nerves that travel in the Vegas. Cholinergic nerves release acetylcholine, which acts on the muscarinic receptors in the airways to produce cholinergic effects. Anticholinergics block only bronchoconstriction mediated through cholinergic nerves, they are not very protective against some stimuli. Although anticholinergic agents have been shown to be effective in patients with COPD, β-agonists are more effective in patients with chronic asthma. 3) Identify the major side effects of beta-agonists and understand how they occur. Tremor and palpitations are the most common side effects, tremor results from stimulation of beta-2 adrenergic receptors in skeletal muscle, and palpitations occur primarily from stimulation of beta-2 adrenergic receptors in the peripheral vasculature, resulting in vasodilation with reflex increase in the force and rate of cardiac contraction. They may also produce a number of metabolic side effects, including hypokalemia when given in high doses, this occurs because catecholamines stimulate potassium uptake by skeletal muscle. 4) Understand the basic pharmacokinetics of theophylline and be able to describe the major factors that decrease theophylline clearance. Theophylline is well absorbed from the GI tract. The volume of distribution is relatively constant between individuals at 0.5 L/kg so that 1 mg/kg will raise the serum level 2 mcg/ml. Theophylline’s clearance, however, varies markedly between individuals and also may vary in the same individual over time. Only 10% is eliminated unchanged by the kidney. The major route of clearance is metabolism by the cytochrome microsomal enzyme system in the liver, and therefore, several drugs and related conditions that affect hepatic metabolism may alter its clearance. Decreased elimination Congestive heart failure, liver disease, Cor pulnonale, hypothyroidism, sustained fever, flu vaccine, high carbohydrate, low-protein diet, allopurinol (high-dose), Cimetidine, ciprofloxacin, Erythromycin, methotrexate, propranolol, Thiabendazole, Verapanil Increased elimination Cigarette smoking, charcoaled broiled meats, hyperthyroidism, low carbohydrate, high protein diet, carbamazepine, phenobarbital, phenytoin, rifampin 5) Describe why there are side effects with inhaled atropine but not with inhaled ipratropium. The therapeutic usefulness of atropine is limited by side effects, due to its high absorption rate it produces systemic effects such as tachycardia, blurred vision, dry mouth, and urinary retention due to blockade of muscarinic receptors outside the lung. Ipratropium is a quaternary ammonium analogue of atropine which has resolved the problem of side effects with inhaled anticholinergic therapy. This is because the positive charge on the quaternary ammonium group makes ipratropium poorly absorbed into the circulation and thus, produces no significant side effects. 6) Be able to describe the mechanism of corticosteroid action at the receptor level. Corticosteroids enter the cells by diffusion and bind to glucocorticoid receptors (GR) which are localized to the cytoplasm of target cells. GR exist as part of a larger heteromeric receptor complex that includes two subunits of heat protein 90 (hsp 90), which dissociate after the corticosteroid binds, thus activating the GR complex and allowing it to enter the nucleus. GR forms a Homo dimer and binds to glucocorticoid response to the elements (GREs), which are DNA sequences located in and around BG our target genes. This results in transcriptional regulation of specific target genes producing either induction or repression of gene transcription. 7) Describe the major potential side effects associated with chronic oral corticosteroid therapy and understand how they can be avoided by use of the inhaled route for administration. Organ system Endocrine Musculoskeletal Ophthalmologic Cardiovascular Psychiatric General Gastrointestinal Cutaneous Adverse effects Adrenal insufficiency, Glucose intolerance Osteoporosis/compression fractures, myopathy, Osteonecrosis Cataracts, glaucoma Hypertension, lipoprotein abnormalities, atherosclerosis Psychosis, depression, mania Cushingoid appearance, obesity, hypokalemia, immune suppression/infection Pancreatitis, Diverticular rupture Purpura, atrophy/fragility, hirsutism, delayed wound healing, acne 8) Understand the general approach to therapy (first line drugs) in patients with asthma and COPD. Asthma therapy - patients at start treatment at the step most appropriate to the initial severity of the condition. Establish control; and decreased treatment to do the least medication necessary to maintain control. All patients receive an inhaled "short acting" beta-2 agonist to be used as needed for attacks of SOB and wheeze. For acute exacerbations, a rescue course of oral prednisone may be needed at any time. Severity class Step 4 severe persistent Step 3 moderate persistent Step 2 mild persistent Step 1 mild persistent Symptoms/Day Symptoms/Night Continual Frequent Daily >1 night/week >2/week but <1 x/day >2 nights/month ≤ 2 days/week ≤ 2 nights/month PEF or FEV1 PEF variability <60% >30% >60%-<80% >30% ≥ 80 20%-30% ≤ 80% <20% Daily medications Preferred treatment: high-dose ICS plus LADA and, if needed, or corticosteroid tablets or syrup long-term Low to medium dose ICS plus LABA Low dose inhaled corticosteroid No daily medication needed COPD - bronchodilators are given either on an as needed basis for relief of persistent or worsening symptoms, or a regular basis to prevent or reduce symptoms. These bronchodilators include beta-2 agonists, anticholinergics, and theophylline (less common). COPD patients are often treated with a combination of beta-2 agonist and anticholinergic bronchodilators. For acute COPD exacerbations: inhaled beta-2 agonist and inhaled anticholinergic.