Fluorescein Angiography
advertisement
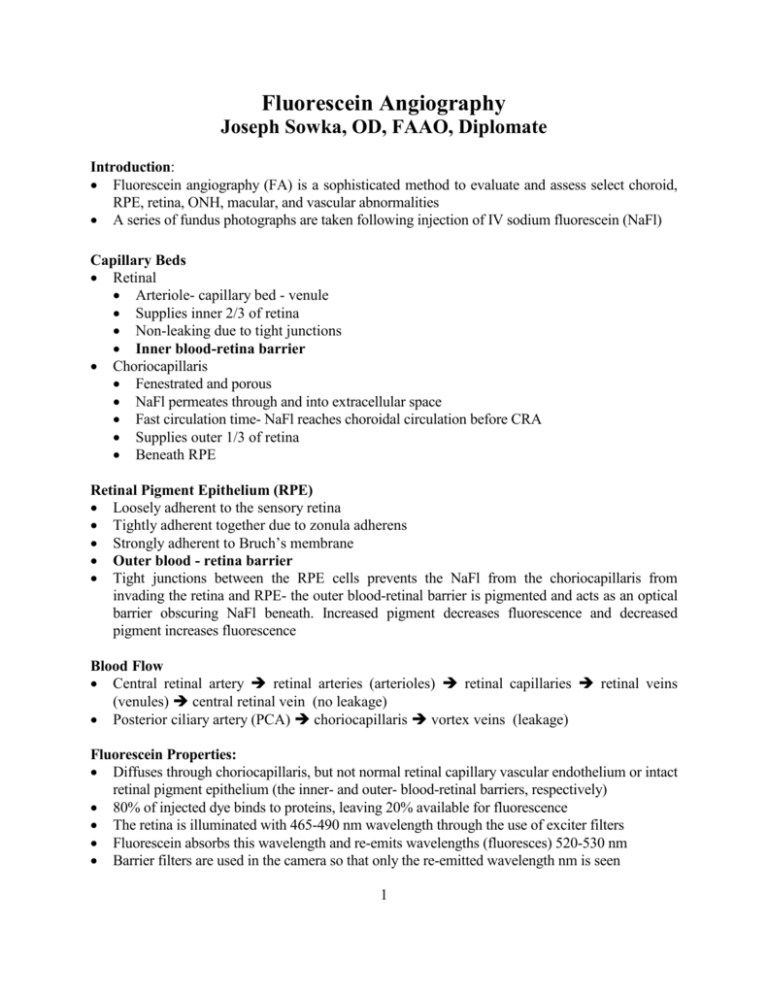
Fluorescein Angiography Joseph Sowka, OD, FAAO, Diplomate Introduction: Fluorescein angiography (FA) is a sophisticated method to evaluate and assess select choroid, RPE, retina, ONH, macular, and vascular abnormalities A series of fundus photographs are taken following injection of IV sodium fluorescein (NaFl) Capillary Beds Retinal Arteriole- capillary bed - venule Supplies inner 2/3 of retina Non-leaking due to tight junctions Inner blood-retina barrier Choriocapillaris Fenestrated and porous NaFl permeates through and into extracellular space Fast circulation time- NaFl reaches choroidal circulation before CRA Supplies outer 1/3 of retina Beneath RPE Retinal Pigment Epithelium (RPE) Loosely adherent to the sensory retina Tightly adherent together due to zonula adherens Strongly adherent to Bruch’s membrane Outer blood - retina barrier Tight junctions between the RPE cells prevents the NaFl from the choriocapillaris from invading the retina and RPE- the outer blood-retinal barrier is pigmented and acts as an optical barrier obscuring NaFl beneath. Increased pigment decreases fluorescence and decreased pigment increases fluorescence Blood Flow Central retinal artery retinal arteries (arterioles) retinal capillaries retinal veins (venules) central retinal vein (no leakage) Posterior ciliary artery (PCA) choriocapillaris vortex veins (leakage) Fluorescein Properties: Diffuses through choriocapillaris, but not normal retinal capillary vascular endothelium or intact retinal pigment epithelium (the inner- and outer- blood-retinal barriers, respectively) 80% of injected dye binds to proteins, leaving 20% available for fluorescence The retina is illuminated with 465-490 nm wavelength through the use of exciter filters Fluorescein absorbs this wavelength and re-emits wavelengths (fluoresces) 520-530 nm Barrier filters are used in the camera so that only the re-emitted wavelength nm is seen 1 Just the Facts: Fluorescein injected into a patient is excited by light coming from the camera and flash (filters allow only specific light to enter the eye) and causes the dye to fluoresce. Only light emitted from the fluorescing fluorescein reaches the camera (due to filters that block all other light). All you can see on an angiogram is fluorescein. The Procedure: Color and red free control photographs are taken prior to injection 5cc of NaFl (10%) or 2 cc (25%) is injected into the antecubital vein (second choice: vein at back of hand) over 2-4 sec Using high-speed 35 mm black and white film (or a digital imaging system), rapid serial photographs are taken at approximately 5 to 20 seconds after NaFl is injected. A timer on the camera is started at the time of injection and records the time that each photo is taken (approximately 1 ½ sec) Late stage photos are taken 5 to 15 minutes later NaFl typically reaches the central retinal artery 10-15 sec after injection. This ranges from 5 to 30 sec depending on cardiac disease, cardiac output, blood viscosity, vascular occlusion, hypertension, renal disease, vessel caliber, etc. Toxicity: NaFl is relatively safe 140-210 gms are needed in order to achieve lethal dose for average sized person Clinical dose is 100 x less than the lethal dose Ophthalmology 1991;98:1139-1142- > 2,000 pts.- No incidence of anaphylaxis, MI, or seizure However, there have been deaths attributed to this procedure Side Effects Skin color changes (temporary) Urine discoloration (temporary) Nausea (2-4%)- occurs 30 sec post injection, lasts 1-3 min. Extravasation and skin necrosis Bronchospasm Laryngeal edema Syncope Anaphylaxis: MI/ cardiac arrest Cardiac arrhythmia Death (1/250,000) Contraindications: Known history of allergy to dye, iodine, shellfish Previous anaphylaxis to FA First trimester of pregnancy (although there are no reported complications) Relative contraindication. Most doctors just have anxiety over invasive diagnostic tests on a pregnant patient 2 Severe renal impairment Recent CVA, MI, unstable angina H/O heart disease, arrhythmia, pacemakers are not complications The Normal Fluorescein Angiogram: Baseline photos (autofluorescence/pseudofluorescence) are taken 0 sec. Inject fluorescein 9.5 sec. Posterior ciliary arteries fill 10 sec. "choroidal flush"- background choroidal fluorescence 10-12 sec. Retinal arterial stage 13 sec. Capillary transition stage 14-15 sec. "Early venous stage", lamellar flow stage", "arterial-venous stage" 16-17 sec. Venous stage 18-20 sec. Late venous stage 5 min. Retrofluorescence, late staining Arterial stage ranges from 2-30 seconds depending on cardiac disease, cardiac output, blood viscosity, and vessel caliber. Choroidal flush can be delayed in a variety of diseases, such as decreased cardiac output, congestive heart failure, giant cell arteritis, hypertension, etc. Clinical Pearl: Giant cell arteritis will give patchy, delayed choroidal filling. Fluorescein Angiography: Definitions Autofluorescence/ pseudofluorescence: Fluorescence seen in the eye prior to fluorescein injection. The fundus is dark unless there is a substance that can convert retinal illumination of 485-500nm to 525-530 nm wavelengths. Example: ONH drusen. This is why photos are taken with filters in place prior to fluorescein injection. Identifies confounding artifacts Transition time: Circulation time. Arm-to-Retina Time. The time it takes fluorescein to reach the central retinal artery after injection. From 5-10 sec., but may be much greater depending on cardiac and vascular status Choroidal flush: Approx. 1 sec after PCA fill and 1 sec prior to retinal arterial phase. PCA fill and flow leads to the choriocapillaris, which are fenestrated and leaky. The fluorescein extravasates into the extravascular space and background fluorescence emerges. Typically described as a ground glass appearance. Pigment acts as an optical barrier and affects the amount of background fluorescence seen. Choroidal fluorescence will eventually be overshadowed by retinal capillary fluorescence. Retinal arterial phase: Fluorescein is in the central retinal artery and appears confluent and white, while the central retinal vein is still black 3 Capillary stage: Engorgement of the capillaries is maximal during the venous stage, and minute details of the retinal capillaries becomes observable, esp. around the foveal avascular zone and optic nerve head Early venous stage AKA lamellar stage, arterial venous stage. Initial appearance of fluorescein in veins is different than in arteries. 1-2 sec after the arterial phase, the veins have a lamellar appearance as fluorescein collects from smaller capillaries and is pushed against the wall of the larger vessels due to flow dynamics. The central lumen remains dark while the wall fluoresce Venous stage: Loss of lamellar appearance to the veins A-V transition time: The time between the arterial phase and venous phase-typically 7-10sec. Increased time indicates vascular occlusion Late venous stage: Retinal veins have a greater concentration of fluorescein than arteries. Fluorescein has circulated and is being removed by the kidneys, while the artery is re-perfusing with blood in greater concentrations than fluorescein. Retrofluorescence: Late choroidal pooling and scleral staining. Considered the "late phase" Macular hypofluorescence: The macula hypofluoresces due to the elevated concentration of RPE and xanthophyll pigment blocking the choroidal fluorescence. There are no retinal capillaries in the area Foveal avascular zone: Retinal capillary free zone (500 microns). Slightly larger than the foveola (350 microns) Clinical Pearl: With the exception of pseudo-and autofluorescence, the only thing that you should see during a fluorescein angiogram is fluorescein. The Abnormal Fluorescein Angiogram: Analyzed: Sequentially Anatomically Morphologically There are only two fundamental principles in angiography: Things will either hyperfluoresce or hypofluoresce. Hyperfluorescence: Hyperfluorescence is caused by: 1. Things that leak (microaneurysm, intra-retinal microvascular abnormality (IRMA), neovascularization, capillary leakage, retinal edema) 2. Things that pool (serous detachment of the RPE or retina) 4 3. Things that stain (sclera, ONH, drusen, vessels after vascular occlusion) 4. Transmission defects (RPE window defects) 5. Abnormal vessels (IRMA, neovascularization, microaneursyms, macroaneurysms, vein occlusions, tumor feeder vessels) Hypofluorescence: Hypofluorescence is caused by: 1. Optical barriers (pigment, blood, exudate, CWS) 2. Filling defects (capillary closure, retinal vascular occlusions) Angiography and Alternatives: Indocyanine Green Angiography (ICG) ICG is a dye that absorbs and emits light near the IR range; this allows for a better penetration of the melanin pigment in the RPE and choroid. ICG also has better penetration of nuclear cataracts, vitreous hemorrhage, and sub-retinal blood and fluid. 98% of ICG is bound to protein, so there is very little leakage from the choriocapillaris. ICG is iodinated, so if the patient has an allergy to contrast dye or shellfish, then they should not undergo this test. ICG is excreted by the liver, so a patient with liver disease should also avoid this test. ICG may be better than fluorescein angiography in the following situations: Occult choroidal neovascular membranes (CNVM) Borders are more easily located CNVM associated with serous detachment of the retina Can better identify CNVM under fluid Limitations: Requires extensive imaging system Quality of image is poor Detailed capillaries are difficult to identify 5