PROTOCOL GOG-0262/ACRIN 6695
advertisement
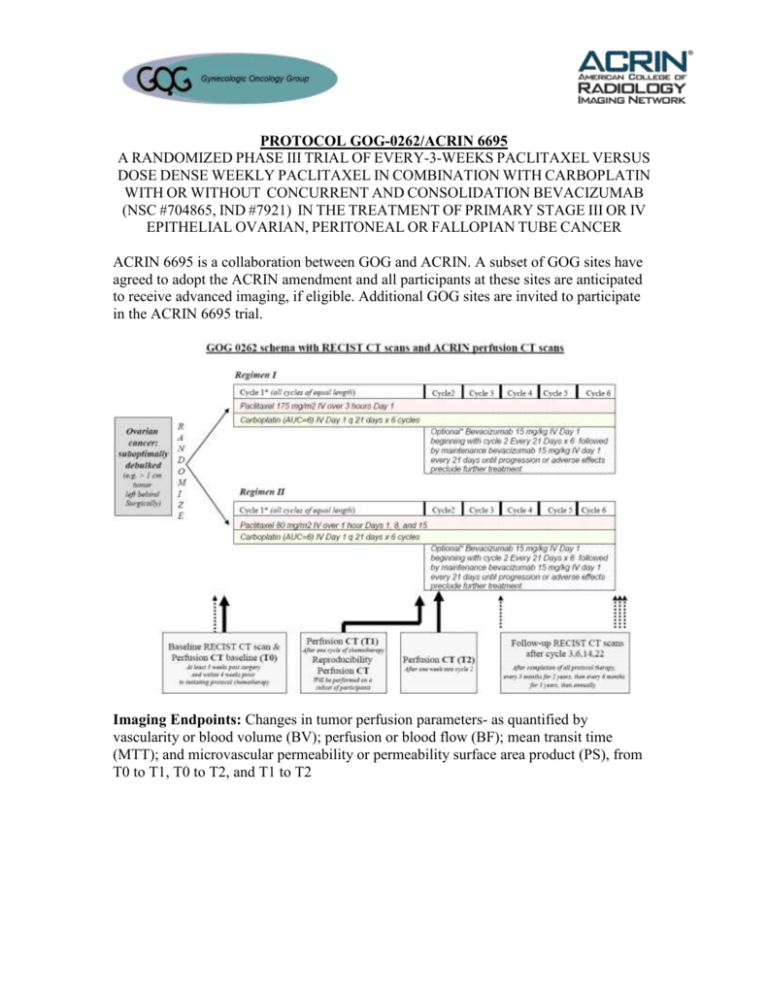
PROTOCOL GOG-0262/ACRIN 6695 A RANDOMIZED PHASE III TRIAL OF EVERY-3-WEEKS PACLITAXEL VERSUS DOSE DENSE WEEKLY PACLITAXEL IN COMBINATION WITH CARBOPLATIN WITH OR WITHOUT CONCURRENT AND CONSOLIDATION BEVACIZUMAB (NSC #704865, IND #7921) IN THE TREATMENT OF PRIMARY STAGE III OR IV EPITHELIAL OVARIAN, PERITONEAL OR FALLOPIAN TUBE CANCER ACRIN 6695 is a collaboration between GOG and ACRIN. A subset of GOG sites have agreed to adopt the ACRIN amendment and all participants at these sites are anticipated to receive advanced imaging, if eligible. Additional GOG sites are invited to participate in the ACRIN 6695 trial. Imaging Endpoints: Changes in tumor perfusion parameters- as quantified by vascularity or blood volume (BV); perfusion or blood flow (BF); mean transit time (MTT); and microvascular permeability or permeability surface area product (PS), from T0 to T1, T0 to T2, and T1 to T2 Objectives: Imaging Primary Objectives To determine whether larger changes in the tumor perfusion parameters from baseline T0 to T2 are prognostic of higher progression-free survival (PFS) rate at 6 months in patients treated with weekly paclitaxel regimen or every-3-week paclitaxel regimen, who are receiving carboplatin with or without bevacizumab. Imaging Secondary Objectives To determine whether larger changes in tumor perfusion parameters from baseline T0 to T1 are prognostic of higher progression-free survival (PFS) rate at 6 months in patients treated with weekly paclitaxel regimen or every-3-week paclitaxel regimen, who are receiving carboplatin with or without bevacizumab. To determine whether larger changes in tumor perfusion parameters values from T0 to T1, T0 to T2 and T1 to T2 are prognostic of better overall survival in all treatment arms. To assess the association between changes in tumor perfusion parameters before and after chemotherapy and subsequent best tumor response according to standard anatomic response evaluation criteria (RECIST). To assess the association between tumor perfusion parameters before chemotherapy and subsequent best tumor response according to standard anatomic response evaluation criteria (RECIST), progression free survival at 6 months and overall survival. To test the assumption that tumor perfusion parameters are reliable, user-independent and reproducible parameters of tumor microvascular characteristics. A subgroup of 15 patients will have repeat CT Perfusion studies at T1 to achieve this objective. Rationale for Imaging in Current Study Traditional biomarkers for ovarian carcinoma has included tumor size and levels of the surface glycoprotein antigen CA125, but these biomarkers are less than optimal for following patients on chemotherapy. Both WHO and/or RECIST morphological criteria do not lend themselves easily to new therapies which often induce lesion necrosis without reducing tumor volume. Tissue biopsy remains an invasive technique that is neither practical nor desirable in ovarian cancer patients and therefore, the identification of non-invasive biomarkers for ovarian carcinoma is of critical importance.1 Advances in new therapeutic modalities present additional challenges. As anti-angiogenic agents largely produce cytostatic effects, traditional measures of efficacy such as response rate (RR) or time-to-progression might overlook an important clinical effect of these agents. Primary endpoints of progression-free survival (PFS) and overall survival (OS) remain the most valid and least ambiguous endpoint for clinical efficacy in antiangiogenic therapies but require significant time and expense to reach. Therefore, the identification of alternative early efficacy biomarkers that may guide drug choice with appropriate dosing, evaluate the pharmacologic response, and assess any drug resistance is of paramount importance.2 The challenge in the development of reliable non-invasive imaging biomarkers in ovarian carcinoma and other gynecological malignancies is the requirement that they document the clinical relevance of pharmacologic response. CT continues to be the mainstay for all anatomical imaging in oncology. The advent of new technologies offers functional evaluation of changes in tumor vascularity before any decrease in tumor volume by morphological evaluation using WHO or RECIST criteria. The advantage of dynamic contrast enhanced or perfusion CT is that it can be readily incorporated into existing CT protocols. Additionally, perfusion CT can provide quantitative (versus relative) functional information for diagnosis, staging, and assessment of tumor grade. The basis for the use of perfusion CT is that the microvascular changes in angiogenesis, as reflected by the derived functional parameters: blood flow (BF), blood volume (BV), mean transit time (MTT) and capillary permeability surface product (PS), may assist in prognosis and therapy monitoring.3 Microvascular functional parameters will be derived from the kinetic analysis of perfusion CT data using CT Perfusion software (GE Healthcare). Perfusion CT has seen a wide spectrum of clinical applications in oncology providing prognostic information based on tumor vascularity and predicting therapeutic effects of the various treatment regimens, including chemoradiation and antiangiogenic drugs.4 Preliminary data from metastatic colon cancer studies have suggested an association of progressive disease and a poor response to chemotherapy with perfusion parameters. 5-6 In head and neck cancers, perfusion CT has been able to identify tumors that are likely to have a favorable outcome following radiotherapy.7 Further head and neck studies have shown the role of perfusion CT in predicting local and regional failure in patients receiving radiotherapy, linking lower perfusion as an independent indicator beside tumor volume to poor response to radiotherapy.8 Similarly, Gandhi et al found that the presence of high tumor perfusion parameters predicted a favorable response to induction chemotherapy as evaluated by tumor volume. 9-10 However, the true value of perfusion CT may be found in the monitoring of the response to new anti-angiogenic drugs. In rodent liver cancer, Kan et al reported that perfusion CT was able to assess changes in liver tumor perfusion in response to antiangiogenic treatment.11 In a clinical trial of patients who had rectal cancer treated with bevacizumab, Willett et al found that CT perfusion characteristics of tumor were correlated with MVD.12 More importantly, perfusion CT was able to detect antiangiogenic changes within 2 weeks after initiation of treatment. As these agents produce disease stabilization (cytostatic) rather than tumor regression (cytotoxic), conventional imaging strategies that rely on changes in tumor size are no longer appropriate.13 Specifically, in hepatocellular carcinoma (HCC) patients, Zhu et al confirmed a reduction of BF, BV and PS but an increase in MTT values after bevacizumab treatment; moreover, baseline MTT and changes in MTT after therapy correlated with the clinical outcome.14 Because the pharmacokinetics, imaging approaches, and clinical outcomes differ by disease site, evaluation of perfusion CT as a biomarker of the response to chemotherapy in treating recurrent ovarian epithelial carcinoma and other gynecological disorders is of paramount importance. While RECIST criteria offer a simplified extraction of imaging data for wide application in clinical trials, the development and validation of clinical trial-acceptable methods and standards to incorporate perfusion CT imaging for derivation of angiogenesis related functional parameters will improve RECIST methodology. If successful, the use of functional imaging parameters as surrogate endpoints in clinical trials could facilitate earlier “go/no go” decisions on drug compounds, faster regulatory approval for new drugs, and earlier use in clinical care. Additionally, early validation of non-response to costly novel therapeutic agents may allow re-allocation of these limited resources. Microvascular functional parameters in tumor can also be derived by dynamic contrast enhanced MRI.15-16 and ultrasound (US) imaging.17 Although MRI offers the advantage of superior contrast resolution without the burden of radiation exposure, the absolute quantification of tumor microvascular functional parameters is difficult because the relationship between signal intensity and contrast (gadolinium) concentration, especially in arteries, is nonlinear.18 Color/power Doppler US with/out (microbubble) contrast provides qualitative rather than quantitative assessments of blood flow and volume, in addition, the reproducibility of US is strongly dependent on operator skills.19 In contrast, perfusion CT can be easily incorporated into routine RECIST imaging protocols without extensive training of personnel and can provide quantitative functional information about the tumor vasculature albeit at the expense of radiation exposure. However, newer image reconstruction techniques can reduce current perfusion CT radiation exposure by 5-10 times without sacrifice of image quality of the derived functional maps.20-21 If this proof-of-concept study is successful, future studies will be performed with the reduced dose technique such that repeated studies on the same patient without concern for excessive radiation dose is feasible. By adding an imaging arm to the main study, there is a potential to identify the quantitative functional parameters of perfusion CT that may act as early predictors of patient response to therapy, progression-free survival and overall survival in ovarian cancer. The data obtained from early imaging is important to the development of early quantitative markers of tumor response and patient outcome to chemotherapy. This proof-of-concept study will demonstrate that derived functional parameters from perfusion CT imaging may act as surrogate markers of ovarian cancer response to chemotherapy and as predictors of patient outcomes. Eligibility for ACRIN 6695 In addition to the eligibility outlined in the GOG 0262 protocol, eligible patients for ACRIN 6695 must include the following criteria: Patients must have at least one tumor/metastasis satisfying the following criteria: (a) lesion size larger than 1 cm residual (“suboptimally debulked” disease) in both the short and long axis in the abdomen or the pelvixs as determined by non-contrast enhanced CT at first radiographic imaging; (b) at least half of the lesion has an attenuation of a least 10 HU in the qualifying pre-contrast CT scan; (c) at least half of the lesion has a maximum enhancement of at least 5HU in the first CT perfusion scan Additionally, patients will be ineligible for the ACRIN 6695 trial if the: (a) patients with contraindication to iodinated contrast for perfusion CT imaging. (b) patients take Metformin. Evaluation of tumor for CT perfusion (Appendix VII) Patients who are enrolled in the GOG-0262 study at ACRIN 6695 participating institutions will be coenrolled in both studies. If the patient declines to participate in the ACRIN 6695 study, the patient will not receive the perfusion CT (at T0), but will continue with the treatment in the GOG-0262 study. If the participant agrees to participate in the ACRIN 6695 study, the patient will be evaluated for eligibility by a noncontrast CT. If ineligible, the patient will be considered off study, but will continue with the treatment in the GOG-0262 study. If eligible, the patient will receive the perfusion CT to evaluate the presence of a target lesion. If no target lesion is present, the patient will be considered off study, but will continue with the treatment in the GOG-0262 study. If eligible, the patient will continue on the ACRIN 6695 study. Patients will be administered water-based oral contrast to avoid the possible confusion between lesion and bowel in the pre-contrast qualifying CT scan. Positive contrast is avoided because of possible motion artifacts from peristalsis in the perfusion CT scan. References 1. Holash J et al. (1999) New model of tumor angiogenesis: dynamic balance between vessel regression and growth mediated by angiopoietins and VEGF. Oncogene 18:5356–5362. 2. Jubb AM et al. (2006) Predicting benefit from antiangiogenic agents in malignancy. Nat Rev Cancer 6: 626–635 3. Lee TY, Purdie TG, Stewart E. CT imaging of angiogenesis. Q J Nucl Med. 200 Sep;47(3):171-87.) 4. Miles KA, Charnsangavej C and Lee FT et al., Application of CT in the investigation of angiogenesis in oncology, Acad Radiol 7 (10) (2000), pp. 840–850. 5. Leggett DA, Kelley BB, Bunce IH, Miles KA. Colorectal cancer: diagnostic potential of CT measurements of hepatic perfusion and implications for contrast enhancement protocols. Radiology 1997;205:716–20. 6. Sommerfeld N, Miles K, Dugdale P, Leggett D, Bunce I. Colorectal cancer: progressive disease is associated with altered liver perfusion on functional CT. In 50th Annual Meeting of the Royal Australia & New Zealand College of Radiologists. 1999 7. Hermans R, Lambin P, Van den Bogaert W, Haustermans K, Van der Goten A, Baert AL. Non-invasive tumour perfusion measurement by dynamic CT: preliminary results. Radiother Oncol 1997;44:159–62 8. Hermans R, Meijerink M, and Van den Bogaert W et al., Tumor perfusion rate determined noninvasively by dynamic computed tomography predicts outcome in head-and-neck cancer after radiotherapy, Int J Radiat Oncol Biol Phys 57 (5) (2003), pp. 1351–1356. 9. Gandhi, E.G. Hoeffner and R.C. Carlos, Computed tomography perfusion of squamous cell carcinoma of the upper aerodigestive tract. Initial results, J Comput Assist Tomogr 27 (5) (2003), pp. 687–693. 10. Gandhi D, Chepeha DB and Miller T et al., Correlation between initial and early follow-up CT perfusion parameters with endoscopic tumor response in patients with advanced squamous cell carcinomas of the oropharynx treated with organ-preservation therapy, AJNR Am J Neuroradiol 27 (1) (2006), pp. 101–106. 11. Kan Z, Phongkitkarun S and Kobayashi S et al., Functional CT for quantifying tumor perfusion in antiangiogenic therapy in a rat model, Radiology 237 (1) (2005), pp. 151–158. 12. Willett CG, Boucher Y and di Tomaso et al., Direct evidence that the VEGF-specific antibody bevacizumab has antivascular effects in human rectal cancer, Nat Med 10 (2) (2004), pp. 145–147 13. Spannuth WA, Sood AK and Coleman RL, Angiogenesis as a strategic target for ovarian cancer therapy Nature Clinical Practice Oncology April 2008 Vol 5, No 4 14. Zhu A.X., Holalkere N.S. and Muzikansky A. et al., Early antiangiogenic activity of bevacizumab evaluated by computed tomography perfusion scan in patients with advanced hepatocellular carcinoma, Oncologist 13 (2) (2008), pp. 120–125. 15. Henderson E, Sykes J, Drost D, Weinmann HJ, Rutt BK, Lee TY. Simultaneous MRI measurement of blood flow, blood volume, and capillary permeability in mammary tumors using two different contrast agents. J Magn Reson Imaging. 2000 Dec;12(6):991-1003 16. Hylton N. Dynamic contrast-enhanced magnetic resonance imaging as an imaging biomarker. J Clin Oncol. 2006 Jul 10;24(20):3293-8 17. Delorme S, Krix M. Contrast-enhanced ultrasound for examining tumor biology. Cancer Imaging. 2006;6:148-52 18. de Bazelaire C, Rofsky NM, Duhamel G, Zhang J, Michaelson MD, George D, et al. Combined T2* and T1 measurements for improved perfusion and permeability studies in high field using dynamic contrast enhancement. Eur Radiol. 2006 Sep;16(9):2083-91 19. Pallwein L, Mitterberger M, Pelzer A, Bartsch G, Strasser H, Pinggera GM, et al. Ultrasound of prostate cancer: recent advances. Eur Radiol. 2008 Apr;18(4):707-15. 20. Thibault JB, Sauer KD, Bouman CA, Hsieh J. A three-dimensional statistical approach to improved image quality for multislice helical CT. Med Phys. 2007 Nov;34(11):4526-44; 21. Lee TY, Bauman G, Hsieh J, Thibault JB, Kozak R. Reducing effective dose from CT Perfusion with adaptive statistical iterative reconstruction (ASIR). RSNA Scientific Assembly and Meeting Program, p696. 2009.