Lecture Notes 18-Blood - People Server at UNCW

THE CARDIOVASCULAR SYSTEM: THE BLOOD
There are three major reasons why a cell becomes less capable of an independent existence as it becomes more specialized? Identify these reasons.
1. It becomes less able to protect itself from temperature changes, toxic chemicals, and changes in pH.
2. The cell loses the ability to seek and devour food.
3. If it is embedded within a tissue, as most body cells are, it cannot move away from its own waste products.
What, then are cells in multicellular animals completely dependent upon for survival?
The internal environment, which must be always kept within physiological limits.
What is the internal environment?
The substance that bathes the differentiated cells, the interstitial fluid,
(intercellular or tissue fluid), carries out these vital processes for the cells and constitutes the internal environment.
What is the relationship between interstitial fluid, plasma, and lymph?
When interstitial fluid enters blood vessels, it is called the blood plasma; when it enters the lymphatic system it becomes lymph. Therefore, interstitial fluid, blood plasma, and lymph are all but the same fluids; along with a few other fluids of the body, they form the extracellular fluid (ECF).
What are the cardiovascular and lymphatic systems?
The blood, blood vessels, and heart form the cardiovascular system.
The lymph, lymphatic vessels, and structures and organs that contain lymphatic tissue form the lymphatic system.
Since blood services all tissues of the body, it is an important medium for the transport of disease-producing organisms throughout the body. Briefly, describe the role of the lymphatic system in protecting the body from such spread of disease.
The lymphatic system receives interstitial fluid, which includes wastes and possibly microorganisms, cancer cells, etc. and filters it through specialized structures called lymph nodes. This in effect concentrates disease-producing organisms, and provides defensive mechanisms for the body, prior to returning the cleansed fluid to the blood for another pass through the body.
191
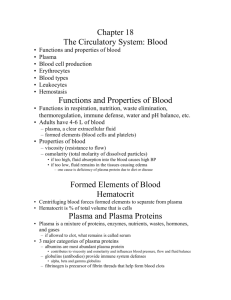
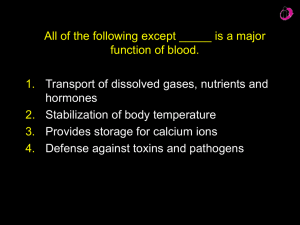
A. COMPONENTS OF THE BLOOD
Name the two main components of whole blood?
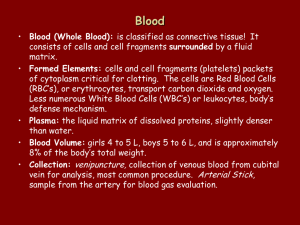
Whole blood consists of a cellular or cell-like portion called the formed elements and a straw-colored liquid portion called the plasma.
1. BLOOD PLASMA
What are the two major components of plasma?
Approximately 55% of whole blood is plasma: 91.5% of this is water.
The remaining 8.5% is solutes, primarily plasma proteins, as well as a multitude of other solutes, all of which are maintained at specific concentrations.
Describe the plasma proteins?
The plasma proteins, formed mainly by the liver, are divided into three large groups: albumins (54%) globulins (38%) fibrinogen (7%)
What is the hematocrit?
The formed elements can be separated from the plasma by placing a sample of blood in a capillary tube and spinning if for a few minutes in a centrifuge. RBCs, being denser than other blood components, become packed into the bottom of the tube and on average constitute about 45% of the total volume of blood. This value is the hematocrit.
Laying atop the packed RBCs is the buffy coat. Making up less than 1% of the total, this layer is composed of leukocytes and platelets.
Above it all is the plasma, a pale yellow fluid that accounts for about
55% of the total.
192
2. FORMED ELEMENTS
What are the three main groups of formed elements in blood?
The formed elements (cells and cell fragments of blood), comprise approximately 45% of whole blood and are classified into three large groups:
1. erythrocytes (red blood cells, RBCs)
2. leukocytes (white blood cells WBCs)
3. thrombocytes (platelets)
How are the leukocytes subdivided?
Leukocytes are divided as follows:
1. granulocytes (granular leukocytes) a. neutrophils b. eosinophils c. basophils
2. agranulocytes (agranular leukocytes) a. lymphocytes b. monocytes
B. FORMATION OF BLOOD CELLS
What is hematopoiesis?
The process by which blood cells are formed is called hematopoiesis
(hemopoiesis) and occurs in three phases during a normal lifespan.
Phase 1 -- Yolk sac stage -- during embryonic life, between weeks 2 - 8, the yolk sac of the embryo produces all blood cells.
Phase 2 -- Hepatic phase - beginning at about the 6 th week of embryonic life and continuing until the birth (peak at about 6 months), the liver primarily, and the spleen, take over all blood cell formation.
Phase 3 -- Myeloid phase -- beginning in the 5 th -8 th month, and then continuing throughout postnatal life, red bone marrow and lymphoid tissues take over all blood cell formation.
Adult life -- Through the ages of 20 years, all bones of the body have red marrow and participate in hematopoiesis. After this, only the flat bones of the skull, the vertebrae, ribs, sternum, and pelvis continue to produce blood cells.
193
What are hemocytoblasts?
In hematopoiesis, stem cells called hemocytoblasts, which reside in bone marrow, give rise to two stem cells, one of the myeloid line and the other of the lymphoid line. From these two precursor cell types all of the seven types of adult formed elements arise.
What are hematopoietic growth factors?
Several hematopoietic growth factors stimulate differentiation along particular developmental paths and cause proliferation of certain progenitor cells so that a particular cell type is made.
C. ERYTHROCYTES (RED BLOOD CELLS)
1. RBC ANATOMY
Describe the erythrocyte anatomy?
What is erythropoietin?
Erythropoietin, a hormone produced mainly by the kidneys, stimulates proliferation and differentiation of the myeloid stem cell along the red blood cell pathway, resulting in increased erythrocyte release into the blood.
More than 99% of the formed elements are erythrocytes (RBCs).
Each is approximately 8 microns (8x10 -6 meters) in diameter and in the shape of a biconcave disc.
Why is RBC shape important?
This flexible biconcave shape:
1. provides the cell with a great deal of surface area for diffusion
2. allows the cells to be squeezed through narrow capillaries, some of which are as small as 3 um in diameter.
Why are RBCs not true cells?
Mature RBCs are not true cells in that they contain no nucleus or other organelles, are incapable of mitosis, and cannot carry out extensive metabolic activities.
RBCs are, instead, membrane bound sacs of hemoglobin, with approximately 280 million hemoglobin molecules per cell.
194
2. RBC PHYSIOLOGY
Describe the hemoglobin molecule?
The hemoglobin molecule consists of a protein portion called globin made up of four chains (alpha1 and 2, beta1 and 2) and four nonprotein iron-containing pigments called heme groups. Each heme is capable of binding to a single oxygen molecule (O
2
).
How does hemoglobin carry and deliver oxygen?
As blood passes through the lung capillaries, each hemoglobin molecule combines reversibly with 4 molecules of O
2
(1 O
2
per heme group). It is carried in this state to the tissues where the iron-
O
2
reaction is reversed. Hemoglobin releases its 4 O
2
molecules, allowing them to diffuse into the interstitial fluid and thus to the cells.
How is the globin portion of hemoglobin used in gas transport?
The globin (protein) portion of the hemoglobin molecule is responsible for carrying 23% of blood carbon dioxide. In the lungs this reaction is reversed to liberate the carbon dioxide for exhalation.
3. RBC LIFESPAN AND NUMBER
What is the normal RBC lifespan?
RBCs live only about 120 days because of wear-and-tear on their membranes as they squeeze through capillaries. Since they cannot repair themselves, they must be removed from the general circulation.
How are they removed from the circulation?
As tattered RBCs pass through the liver, spleen, and bone marrow, they are recognized by macrophages as damaged and are removed from the circulation by phagocytosis.
What is recycled or excreted?
The breakdown products of hemoglobin are either recycled or excreted. Iron recycles as hemosiderin, the globin portion is converted to amino acids for use, and the pigmented portion of the heme is excreted as bilirubin.
195
What are normal RBC values?
To maintain normal numbers of RBCs, new RBCs must enter the circulation from bone marrow at the rate of at least 2 million per sec to maintain balance between production and destruction. males = 5.4 million/ mm 3 females =4.8 million/mm 3
D. LEUKOCYTES (WHITE BLOOD CELLS)
1. WBC ANATOMY AND TYPES
2. WBC PHYSIOLOGY
3. WBC LIFESPAN AND NUMBER
Name and give a brief description of each of the two main categories of leukocytes, then list each cell type and the normal percentage of said cell in the general circulation.
1. granulocytes -- lobed nuclei, conspicuous granules a. neutrophils -- 60-70% b. eosinophils -- 2-4% c. basophils -- 0.5-1%
2. agranulocytes -- rounded, indented nuclei; granules not conspicuous d. lymphocytes -- 20-25% e. monocytes -- 3-8%\
Describe the functions of each of the following blood cell types: neutrophils -- Neutrophils respond to tissue destruction by bacteria most rapidly, providing a first line of defense for the body.
Their defense role is to engulf by phagocytosis microorganisms, cell debris, dying and dead cells. eosinophils -- Eosinophils mediate inflammatory and allergic responses by secreting antihistamines. They also phagocytize antigen-antibody complexes and are effective against certain parasites (exactly how is not known). basophils -- Basophils intensify inflammatory and allergic reactions by releasing histamines (cause increased capillary permeability), heparin (anticoagulant), and serotonin
(mediates pain response).
196
lymphocytes -- Lymphocytes are of two types:
1. T cells are responsible for cell mediated immunity.
2. B cells are responsible for antibody-mediated immunity.
They come in a variety of sizes, from about the size of an
RBC to just smaller than the other WBCs (more later with the lymphatic system. monocytes -- Monocytes leave the blood and enter the tissues after
1-2 days to become wandering or fixed macrophages. They perform the same work as neutrophils, but are more efficient.
They also play an important role in presentation of antigens to lymphocytes during immunity.
Describe the following: chemotaxis -- All WBCs have, to some extent, the ability to leave the blood and enter the tissue spaces to arrive at a site of inflammation and infection. The cells are attracted to an infected area in response to various chemicals, called chemotactic factors that are released by damaged tissue cells. Their movement along this “path” is called chemotaxis. margination/pavementing -- At the point where chemotactic factors are diffusing into the blood, the WBCs are attached to the capillary lining and line up along it, moving out oft the general circulation. This process is called margination and pavementing. diapedesis/emigration -- WBCs then begin to move between the capillary lining cells to enter the tissue spaces (diapedesis and emigration). WBCs literally squeeze between two adjacent cells of the capillary wall, then migrate by ameboid motion along the diffusion gradient created by the chemotactic factors, to finally reach the site of inflammation.
WBC lifespan/number -- The average lifespan of WBCs is only a few days since they are constantly waging a battle against invading microorganisms and other pathogens. The blood normally has 5,000-10,000 WBCs/mm 3 .
197
E. THROMBOCYTES (PLATELETS)
What is the origin of thrombocytes?
Thrombocytes are formed in the bone marrow from the stem cell known as the hemocytoblast. Upon proper stimulation (thrombopoietin), the hemocytoblast enters the developmental pathway that gives rise to the megakaryocyte. The megakaryocyte, lying in the bone marrow, sheds fragments of cytoplasm enclosed in cell membrane, each fragment being a thrombocyte (not true cells).
Describe the basic structure of a thrombocyte and give its normal numbers and lifespan in the circulating blood?
Each thrombocyte is a biconvex disc filled with blood clotting factors but without normal cellular organelles. There are 250,000-400,000/mm 3 of blood. They have a lifespan of 5-9 days in the general circulation.
F. HEMOSTASIS
What is hemostasis? stoppage of bleeding.
When a blood vessel is ruptured, what three conditions must the hemostatic response meet?
The hemostatic response must be 1) quick, 2) localized to the injured area, and 3) carefully controlled.
Name the three hemostatic processes which are initiated with each break in the circulation.
1. vascular spasm
2. platelet plug formation
3. coagulation
1. VASCULAR SPASM
Describe the vascular spasm response of hemostasis?
In response to any physical insult, the circular smooth muscle fibers in the walls of blood vessels, particularly arteries and arterioles, contract immediately. This vascular spasm reduces the diameter of the blood vessel and reduces the amount of blood flowing through the vessel. During this time (minutes to hours), the other hemostatic mechanisms exert their effects in the damaged area.
198
2. PLATELET PLUG FORMATION
Describe each of the following: initiation of plug formation --Platelet plug formation is initiated when collagen receptors on the surface of thrombocytes come into contact with ragged collagen fibers exposed in the damaged vessel wall. platelet adhesion -- Binding of the platelets to the exposed collagen fibers is called platelet adhesion, and results in the accumulation of thrombocytes at the wound site. platelet release reaction -- As a result of platelet adhesion, the thrombocytes begin to stick to one another at the wound site and release the contents of their granules. This process is called the platelet release reaction. platelet aggregation -- The various liberated factors initiate a process called platelet aggregation in which other nearby thrombocytes are attracted to the wound site and also stick, forming a loosely-woven plug.
Other factors enhance vascular spasm, are involved in the coagulation process, and are used later to destroy the clot in a process called fibrinolysis.
3. COAGULATION (CLOTTING)
Blood normally remains liquid as long as it stays within its vessels. What happens when it is drawn from the body?
When it is drawn from the body, blood will thicken to form a gel called a clot, leaving a straw-colored fluid called the serum (plasma minus its clotting proteins).
Of what does a clot consist?
The clot consists of a network of insoluble protein fibers called fibrin in which the formed elements become trapped.
The process of gel formation (clotting) is known as what? coagulation
199
Describe the basic clotting mechanisms. Include the three basic steps involved and the process of clot retraction.
Clotting involves several enzymes, a number of factors, and vitamins that work together in a cascade of events that acts in a positive feedback manner to form a large quantity of product.
In general, the clotting mechanism involves four basic stages that occur after the tissue injury. There are two reaction pathways to coagulation. One reaction pathway is called the extrinsic mechanism which is initiated by clotting factors released by the damaged blood vessel and surrounding tissue. (Extrinisic means clotting factors don’t come from the blood itself) The other reaction pathway is called the intrinsic mechanism in which blood may also clot without tissue factors. In most cases of bleeding, both pathways are activated.
1. In the extrinsic mechanism, thromboplastin from damaged tissues in combination with another clotting factor and Ca2+ activates the plasma protein factor X. In the intrinsic mechanism, platelets release a clotting factor that leads to a cascade of other clotting factors being activated which ultimately along with Ca2+ activates protein factor X.
2. Protein factor X in combination with factor V and Ca 2+ , forms
prothrombinase (prothrombin activator) in the blood.
3. Prothrombinase (prothrombin activator) converts the inactive plasma protein prothrombin to its active form, thrombin.
Thrombin has 3 effects: cause more prothrombinase formation, activate more platelets, and activate fibrin.
4. Thrombin converts the soluble inactive plasma protein fibrinogen to the insoluble fibrin. Fibrin forms the threads of clots by cross-linking with others of its kind to become interwoven between the aggregated platelets.
Once the basic clot is formed, the fibrin threads undergo the process of clot retraction (syneresis), in which they contract and pull the clot, along with the platelets and attached blood vessel walls together into a tight mass.
Once syneresis has occurred, the bleeding is permanently stopped and the vessel can begin to repair itself. (Elapsed time = 1 minute for a basic finger prick).
200
4. FIBRINOLYSIS
Define fibrinolysis. dissolution of a clot
What is plasminogen-activating factor (PAF)(kallikrein) and what does it do?
When a clot forms it incorporates into itself an inactive plasma protein known as plasminogen. The substance plasminogen activating factor (PAF) or (kallikrein), an enzyme eventually formed from the release of a clotting factor from platelets when they rupture, slowly converts plasminogen into its active form, plasmin.
What is the function of plasmin?
Plasmin acts as an enzyme to slowly digest the fibrin threads formed during coagulation and allows the clot to dissolve. Clot removal time coincides with the time when vessel wall repair has been completed.
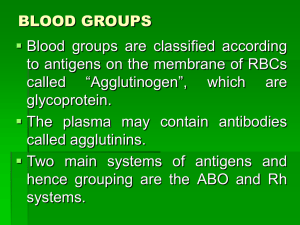
G. GROUPING (TYPING) OF BLOOD
The current blood grouping (typing) system relies on the identification of agglutinogens. What are they?
The cell membrane surface of erythrocytes bears genetically determined glycolipid molecules called agglutinogens.
How many different agglutinogens and grouping systems are there?
There are at least 100 blood group systems and more than 500 agglutinogens have been found on the RBCs.
What are the two most commonly used blood typing systems?
ABO and Rh.
1. ABO
Describe how a person’s blood type could be each of the following: type A -People whose RBCs bear the A agglutinogen, but not the
B agglutinogen, are said to have type A blood. type B -- People whose RBCs bear the B agglutinogen, but not the
A agglutinogen, are said to have type B blood.
201
type AB -- People whose RBCs bear both the A agglutinogen and the B agglutinogen are said to have type AB blood. type O -- People whose RBCs bear neither the A agglutinogen nor the B agglutinogen are said to have type O blood.
What are agglutinins and which are in the following blood types:
Most people’s blood plasma contains genetically determined antibodies called agglutinins (anti-A and anti-B) that will react with either the A agglutinogen or the B agglutinogen if the two are mixed. type A -- People with type A blood have on their RBCs the A agglutinogen and in their plasma the anti-B agglutinin. type B -- People with type B blood have on their RBCs the B agglutinogen and in their plasma the anti-A agglutinin. type AB -- People with type AB blood have on their RBCs the A and B agglutinogens and in their plasma they have neither the anti-A not anti-B agglutinin. type O -- People with type O blood have on their RBCs neither the
A nor the B agglutinogen and in their plasma they have both the anti-A and the anti-B agglutinins.
Describe agglutination and the consequences of hemolysis?
In an incompatible blood transfusion, agglutinins bind to their agglutinogens, causing the RBCs to agglutinate (clump) and undergo hemolysis. The liberated hemoglobin from hemolysis causes kidney damage and can result in death; therefore, it is vital to know who can receive which blood component from whom.
2. RH
What is the basis of the Rh system of blood grouping?
Like the ABO system, Rh is based on the presence of the agglutinogen Rh (called the Rh factor) on the surface of RBCs. A person who is Rh+ bears the agglutinogen, while a person who is
Rh- does not.
Unlike the ABO system, there are no Rh agglutinins in plasma.
202
What is the concern with the Rh factor when considering blood transfusions?
An Rh+ person can receive blood from an Rh- donor, but not vice versa. Introduction of Rh+ RBCs into Rh- blood results in an immune reaction, resulting in hemolysis, and possibly anaphylactic shock and death.
Describe the Rh incompatibility that leads to erythroblastosis fetalis.
1. Mother must be Rh-negative. With an Rh+positive father, the baby has a 50% or 100% chance or being Rh-positive.
2. Before or during delivery of the first Rh-positive baby, Rh- positive RBCs from the fetus enter the blood of the Rhnegative mother through a tear in the placenta.
3. The mother becomes immunologically sensitized to the
Rh-positive RBCs, producing antibodies against the Rh factor. This usually happens after delivery so it poses no threat to the first child.
4. During a subsequent pregnancy with another Rh-positive fetus, some Rh-positive RBCs may enter the maternal blood through minute tears in the placenta. These stimulate the mother to rapidly produce antibodies against the fetal RBCs.
Since antibodies freely cross the placenta, they enter the fetal blood, causing agglutination and hemolysis of the fetal
RBCs.
203