CHAPTER 29 Clostridium, Peptostreptococcus

CHAPTER 29
Clostridium, Peptostreptococcus, Bacteroides, and
Other Anaerobes
The bacteria discussed in this chapter are united by a common requirement for anaerobic conditions for growth. Organisms from multiple genera and all Gram stain categories are included. Most of them produce endogenous infections adjacent to the mucosal surfaces, where they are members of the normal flora. The clostridia form spores that allow them to produce diseases, such as tetanus and botulism, following environmental contamination of tissues or foods.
G ENERAL F EATURES : A NAEROBES AND A NAEROBIC
I INFECTION
I. BACTERIOLOGY: ANAEROBIC BACTERIA
A. THE NATURE OF ANAEROBIOSIS
1. Anaerobes require low oxygen to initiate growth
2. Oxygen tolerance is a continuum
3. Low redox potential is required
4. Hydrogen peroxide and superoxide defense against oxygen products is lacking
5. Pathogens often have catalase and superoxide dismutase
B. CLASSIFICATION
1. Biochemical, cultural, and molecular criteria define many species a. Anaerobic Cocci
1. Gram (+) = Peptostreptococcus
2. Gram (–) = Veillonella b. Clostridia
1. The clostridia are large, spore-forming, Gram-positive bacilli
2. Spores vary in shape and location
3. Hemolysin, neurotoxin, and enterotoxin production cause disease c. Nonsporulating Gram-positive Bacilli
1. Propionibacterium is a genus of small pleomorphic
2. Eubacterium is a genus that includes long slender bacilli commonly found in the colonic flora
3. Usually benign members of the normal flora d. Gram-negative Bacilli
1. Most common bacteria isolated from abdominal anaerobic infections are in the genus Bacteroides
2. Others include Fusobacterium, Porphyromonas, and
3. B. fragilis group produces
β
-lactamase and superoxide dismutase
II. ANAEROBIC INFECTIONS
A. EPIDEMIOLOGY
1. Low redox normal flora sites are the origin of most infections
2. Spore-forming clostridia also come from the environment
B. PATHOGENESIS
1. Anaerobes displaced from normal flora to deeper sites may cause disease
2. Trauma and host factors create the opportunity for infection
3. Flora may be aspirated or displaced at a distance
4. Brain abscess typically involves anaerobic bacteria
5. Capsules and toxins are known for some anaerobes
6. Survival in oxidized conditions can be a virulence factor
7. Mixed infections may facilitate an anaerobic microenvironment
III. ANAEROBIC INFECTIONS: CLINICAL ASPECTS
A. MANIFESTATIONS
1. Abscesses are usually caused by Bacteroides, Fusobacterium, or peptostreptococci
2. Foul-smelling pus suggests anaerobic infection
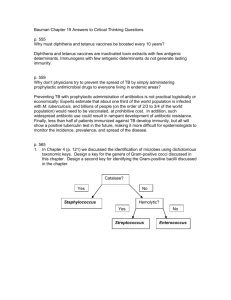
B. DIAGNOSIS
1. Specimens must be direct from the lesion and protected from oxygen
2. Gram staining is particularly useful
3. Anaerobic incubation jar provides proper atmosphere
4. Selective media inhibit facultative bacteria
C. TREATMENT
1. Drainage of the purulent material is the primary treatment
2. Mixed infections and slow growth dictate empiric therapy
3. Abdominal infections require β -lactamase–resistant antimicrobics
4. Metronidazole, imipenem, azethreonam, or ceftriaxone are effective
C
LOSTRIDIUM
P
ERFRINGENS
I. BACTERIOLOGY
1. C. perfringens is a large, Gram-positive, nonmotile rod with square ends
2. Hemolysis and gas production are characteristic
3. Typing system is based on toxins
4. Phospholipase
α
-toxin, pore-forming θ -toxin, and enterotoxin cause disease
II. C. perfringens DISEASE
A. EPIDEMIOLOGY a. Gas Gangrene
1. Gas gangrene develops in traumatic wounds with muscle
2. Spores from the host or environment contaminate wound
3. Delays allow bacterial multiplication b. Clostridial Food Poisoning
1.
C. perfringens can cause food poisoning if spores of an enterotoxinproducing strain contaminate food
2.
Bacteria multiply in meat dishes
B. PATHOGENESIS a. Gas Gangrene
1. Low redox favors multiplication and
α
-toxin production
2. Toxins lead to shock b. Clostridial Food Poisoning
1. Spores survive cooking
2. Vegetative cells produce enterotoxin
III. C. perfringens: CLINICAL ASPECTS
A. MANIFESTATIONS a. Gas Gangrene
1.
Gas gangrene usually begins 1 to 4 days after the injury but may start within 10 hours
2.
Severe wound pain evolves to edema and sometimes tissue crepitance
3.
Systemic findings are those of shock with intravascular hemolysis, hypotension, and renal failure b. Anaerobic Cellulitis
1. Anaerobic cellulitis is a clostridial infection of wounds and surrounding subcutaneous tissue
2. Gas is more likely than in gas gangrene
c. Endometritis
1. C. perfringens gains access to necrotic products of conception retained in the uterus
2. Nonsterile abortion is greatest risk d. Food Poisoning
1. The incubation period is 8 to 24 hours
2. Diarrhea without fever or vomiting is most common
B. DIAGNOSIS
1. Isolation of clostridia alone is not sufficient
2. Diagnosis is based ultimately on clinical observations
3. In clostridial food poisoning, isolation from ingested food confirms
C. TREATMENT AND PREVENTION
1. Surgical treatment is essential for gas gangrene and endometritis
2. Antibiotics and hyperbaric oxygen are useful
3. Debridement of dead tissue is best
4. Prevention of food poisoning involves good cooking hygiene and adequate refrigeration
C
LOSTRIDIUM
B
OTULINUM
I. BACTERIOLOGY
1. Botulinum toxin is the most potent toxin known in nature
2. Cells germinating from spores produce neurotoxin in food
3. Blockage of synaptic acetylcholine release causes paralysis
4. Toxin is destroyed by boiling
II. BOTULISM
A. EPIDEMIOLOGY
1. Spores are widely distributed in nature
2. Alkaline foods favor toxin production
3. Inadequately heated home-canned foods are most common source
B. PATHOGENESIS
1. Food-borne botulism is an intoxication, not an infection
2. Preformed toxin is readily absorbed
3. Acetylcholine block leads to paralysis and autonomic effects
III. BOTULISM: CLINICAL ASPECTS
A. MANIFESTATIONS
1. Food-borne botulism usually starts 12 to 36 hours after ingestion of the toxin
2. Blurred vision progresses to symmetrical paralysis a. Infant Botulism
1. Nonsterile honey introduces spores to intestine
2. Ingested spores yield vegetative bacteria which produce small amounts of toxin in the infant’s colon
3. Lethargy, poor feeding occur in addition to adult signs b. Wound Botulism
1. Contaminated wounds of drug users are sites of toxin production
B. DIAGNOSIS
1. Toxin can be detected in reference laboratories
C. TREATMENT AND PREVENTION
1. Supportive measures and antitoxin allow survival
2. Cooking food inactivates toxin
3. Botox removes wrinkles
C
LOSTRIDIUM
T
ETANI
I. BACTERIOLOGY
1. Gram-positive rods with drumstick-like spore
2. Tetanospasmin or tetanus toxin, has structural and pharmacologic features similar to botulinum toxin
3. Toxin blocks release of neurotransmitters
4. Neurotransmitters are ones which affect inhibitory neurons
5. Result is unopposed firing of the active motor neurons,
6. Formaldehyde treatment removes toxicity but retains antigenicity
II. TETANUS
A. EPIDEMIOLOGY
1. Spores from environment germinate in wounds
2. Nonsterile technique can lead to tetanus
B. PATHOGENESIS
1. Trauma provides growth conditions
2. Tetanospasmin produced at the local site ascends through nerves to anterior horn
3. Blockage of reflex inhibition causes spasmodic contractions
III. TETANUS: CLINICAL ASPECTS
A. MANIFESTATIONS
1. Incubation period varies with distance from injury site to CNS
2. Masseter muscle contraction causes lockjaw
3. Respiratory failure leads to death
B. TREATMENT
1. Specific treatment of tetanus involves neutralization of any unbound toxin with human tetanus immune globulin (HTIG)
2. Supportive treatment required until axons regenerate
C. PREVENTION
1. Childhood toxoid immunization prevents disease
2. Tetanus toxoid, combined with diphtheria toxoid and pertussis vaccine (DTaP) for primary immunization
3. Boosters required every 10 years
4. Passive immunization used when immunization is neglected
C
LOSTRIDIUM
D
IFFICILE
I. BACTERIOLOGY
1.
C. difficile is a Gram-positive rod that readily forms spores
2.
A and B toxins disrupt cytoskeleton signal transduction
3.
A is a enterotoxin
4.
B is a cytotoxin
II. C. difficile DIARRHEA
A. EPIDEMIOLOGY
1.
Source is endogenous or environmental
2.
C. difficile is present in the stool of 2 to 5% of the general
3.
Most frequent cause of antibiotic-associated diarrhea
4.
Major cause of pseudomembranous colitis (PMC)
B. PATHOGENESIS
1. Systemic antimicrobial treatment selects for C. difficile
2. Increased numbers increase toxin production
3. An enterotoxin stimulates watery diarrhea
C. IMMUNITY
Antitoxin antibodies have protective effect
III. C. difficile DIARRHEA: CLINICAL ASPECTS
A. MANIFESTATIONS
1. Diarrhea ranges from mild to PMC
B. DIAGNOSIS
1. Stool toxin detection is the primary diagnostic tool
C. TREATMENT
1. Oral metronidazole or vancomycin reach bacteria in the intestine
B
ACTEROIDES
F
RAGILIS
I. BACTERIOLOGY
1. These slim, pale-staining, Gram-negative rods
2. Oxygen-tolerant species produces superoxide dismutase
3. Polysaccharide capsule is present
II. B. fragilis DISEASE
A. EPIDEMIOLOGY
1. Endogenous infection mixed with other intestinal bacteria
B. PATHOGENESIS
1. Pili and oxygen-tolerance aid initial stages
2. Capsule resists phagocytosis and stimulates abscess production
3. Diarrheal enterotoxin is possible
C. IMMUNITY
1. Cell-mediated immunity may be protective
III. B. fragilis: CLINICAL ASPECTS
A. MANIFESTATIONS
1. Abdominal pain and fever may evolve to peritonitis
2. Abscesses combined with other anaerobes and Enterobacteriaceae
TREATMENT
1. B. fragilis isolates almost always produce a
β
-lactamase, which not only inactivates penicillin but other
β
-lactams, including many cephalosporins
2. Cephalosporin resistant to β -lactamase is required