Abdominal Pain Protocol
advertisement
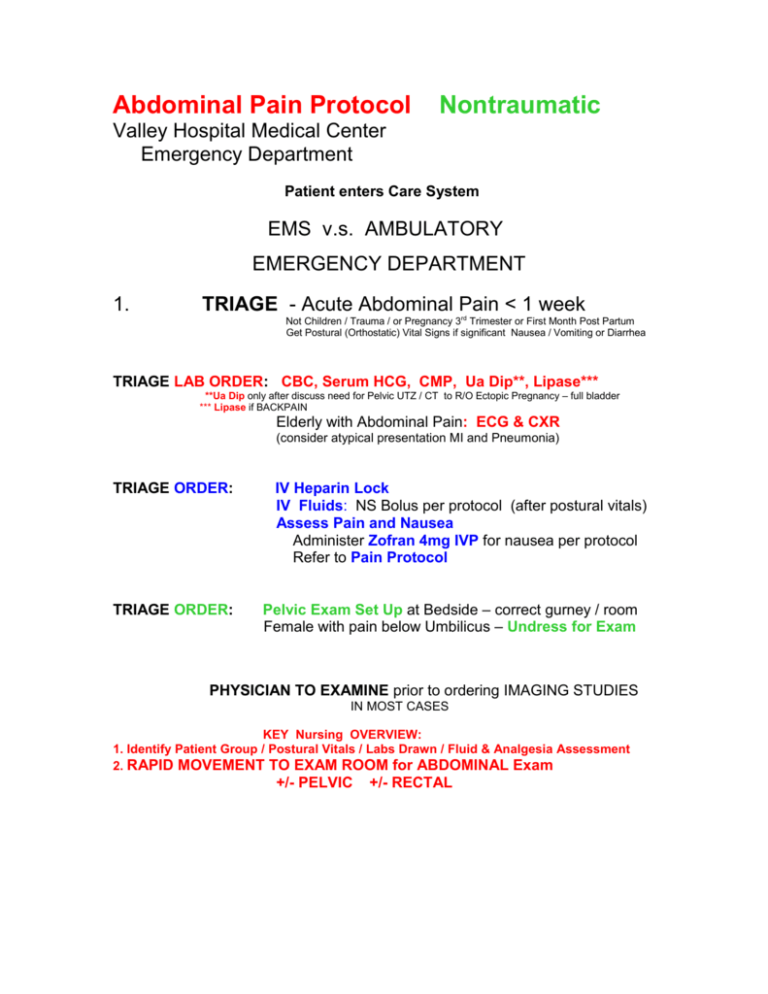
Abdominal Pain Protocol Nontraumatic Valley Hospital Medical Center Emergency Department Patient enters Care System EMS v.s. AMBULATORY EMERGENCY DEPARTMENT 1. TRIAGE - Acute Abdominal Pain < 1 week Not Children / Trauma / or Pregnancy 3rd Trimester or First Month Post Partum Get Postural (Orthostatic) Vital Signs if significant Nausea / Vomiting or Diarrhea TRIAGE LAB ORDER: CBC, Serum HCG, CMP, Ua Dip**, Lipase*** **Ua Dip only after discuss need for Pelvic UTZ / CT to R/O Ectopic Pregnancy – full bladder *** Lipase if BACKPAIN Elderly with Abdominal Pain: ECG & CXR (consider atypical presentation MI and Pneumonia) TRIAGE ORDER: TRIAGE ORDER: IV Heparin Lock IV Fluids: NS Bolus per protocol (after postural vitals) Assess Pain and Nausea Administer Zofran 4mg IVP for nausea per protocol Refer to Pain Protocol Pelvic Exam Set Up at Bedside – correct gurney / room Female with pain below Umbilicus – Undress for Exam PHYSICIAN TO EXAMINE prior to ordering IMAGING STUDIES IN MOST CASES KEY Nursing OVERVIEW: 1. Identify Patient Group / Postural Vitals / Labs Drawn / Fluid & Analgesia Assessment 2. RAPID MOVEMENT TO EXAM ROOM for ABDOMINAL Exam +/- PELVIC +/- RECTAL Acute Abdominal Pain Protocol 2. Nontraumatic Emergency Dept Provider Evaluation History & Physical with Abdominal +/- Pelvic +/- Rectal Exams: Classical Appendicitis - RLQ Pain onset within 24 hours steadily worsening Call Surgeon on Call (May be in-house and see immediately) v.s. CT Abd/Pelvis + IV Contrast Check Basic Lab / Fluids / Analgesia / Antiemetic – at Triage Left Sided Lower Abdominal Pain & Sick – consider CT Abdomen / Pelvis with IV Contrast Consider Enema Contrast. (Oral Route = 2 to 3 hours average prior to doing the study)*** Renal Colic – Spiral (Stone) CT Screen urine for stone / Tordal 30mg IV max * Tordal - caution in elderly / renal failure / dehydration Upper Abdominal Pain - DO NOT LIMIT DIFFERENTIAL in very ill, or elderly patient, or pregnant Generally RUQ Ultrasound for GB Disease / Liver Disease & best for GB stones CT ABDOMEN / PELVIS considered superior study overall. DO NOT limit the Diagnosis – may still be atypical Appendicitis / Perforation / other Life Threat KEY: ATYPICAL APPENDICITIS in Elderly – NEGATIVE CT DOES NOT RULE OUT DX ! Rectal Exam - In general – Still listed in ACEP protocol + Hemacult Little help in Appendicitis Pelvic Exam - In general – In female with Lower Abdominal / Pelvic Pain. Acute Abdominal Pain Protocol Nontraumatic 3. Confirmatory Studies LAB Provider Order - consider ABG PT / PTT Type & Hold v.s. Type and Cross if bleeding - Hemodynamic Instability or Co-Morbidity with GI Bleed Do not base order on the Hgb/HCT which may not have equilibrated yet. Lipase if Backpain Check Anion Gap (If Elevated consider differential and potential poisoning as cause of Abd Pain) Order Lactate if Elevated AG or possible Sepsis – if > 4 consider Sepsis & high risk patient. Serum Ketones & Lactate if DKA + ECG and Cardiac Enzymes (MI is Key cause of DKA, and DKA often presents as Acute Gastroenteritis) Urine Micro and Culture if indicated Blood Cultures for Fever / Hypotension / Shock / Hypothermia & Tachypnea in elderly Additional Studies as Indicated XRAY Provider Order – Consider as Indicated CT Abd / Pelvis Without Contrast / IV Contrast / Enema Contrast / PO Contrast ** UTZ Abd / Pelvis Pregnant UTZ RUQ Gallbladder / Liver AAS Acute Abdominal Series: Free Air / Obstruction / stones Appendicolith < 10% Acute Appendicitis but very suggestive CXR pneumonia Remember : #1 Diagnosis on “Missed Appy” = AGE #1 Diagnosis on “Missed DKA” = AGE #1 Life-Threat triggering DKA in Adult Type I DM = MI ALWAYS look for atypical presentations in this group ALWAYS consider Mesenteric Ischemia prior to Discharge. Acute Abdominal Pain Protocol 4. Nontraumatic Discharge Planning KEY: a. ALL Patients discharged with ongoing NON-Traumatic Abdominal Pain are advised that a repeat exam in 12 hrs is required. b. ALL Patients discharge with abdominal pain whether resolved or not, are advised that they must: “Return for 2 to 3 hours of steady, progressive, persistant Abdominal Pain, Fever > 100, vomiting, or problems.” c. ALL Patients discharged with NON-Traumatic Abdominal Pain are placed at “Bowel Rest” for 24 hours = Clear Liquids with emphasis on small amounts frequently (2 tsp or 2 sips q 10 min) Inability to keep fluids down constitutes rationale for immediate re-evaluation & return to E.D. d. ALL Patients are advised that a Normal Abdominal CT Scan DOES NOT GUARANTEE the absence of Appendicitis ! e. ALL Patients must be monitored for the next 24 to 48 hours, and return to E.D. for ongoing, progressive or new problems. Generally they will be observed at home by family members. Acute Abdominal Pain Protocol Nontraumatic 5. Admitting the Patient ADMIT TO: Surgeon Admit Surgical Floor Admit to O. R. Consult in E.Dept. Hospitalist Admit to Observation Admit to Medical Floor Admit to Surgical Floor Admit to PCU Admit to ICU Gastroenterologist GI Bleed / PUD / ERCP Biliary Disease Pancreatic Disease Liver Disease Consult in E. Dept. INTERQUAL OBSERVATION CRITERIA VITAL SIGNS Temp > 101 for 3 weeks or > 103 or < 95 Pulse > 100/min or < 60/min Respiratory Rate > 24/min or < 12/min Systolic B/P < 100 mmHg RESPIRATORY LABS Arterial Blood Gas pH > 7.45 or < 7.30; p02 < 60; pCO2 > 45 O2 Sat < 91%; PEF 50 to 70%; CO 25 – 29%; supplemental 02 > 28% LAB HCT < 25; Blood Sugar > 400 or < 50; BUN > 35; Creat > 3.0 K > 5.5 or < 3.0; Sodium > 150 or < 120 INTERQUAL INPATIENT ADMISSION CRITERIA VITAL SIGNS Temp > 104 or < 91 Pulse > 120 or < 45 Respiratory Rate > 35 or < 8 Systolic BP < 90 mmHg RESPIRATORY LABS Arterial Blood Gas pH > 7.50 or < 7.25; p02 < 56 or pC02 > 50 O2 Sat < 89%; PEF < 50%; CO > 30%; supplemental 02 > 40% LAB HCT < 18 or < 25 if over 65 Y/O; Platelets > 1 Million or < 75,000; INR > 2 PT > 1.5; PTT > 1.5; Blood Sugar > 500 or < 40; BUN > 65; Creatinine > 5.0 Potassium > 6.0 or < 2.5; Sodium > 160 or < 110; Calcium > 15 or < 5 Blood > 4 Units/24hrs; IV Fluids > 4 Liters/24hrs MEDICATIONS Analgesics > 3x in 24hrs Bronchodilators > 6x in 24hrs Diuretics > 2x in 24 hrs Antibiotics > 3x in 24 hrs







