doc - School of Medicine

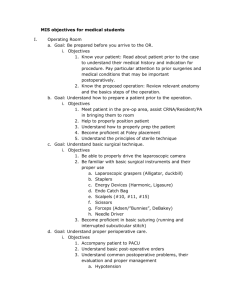
Goals and Objectives
The programs goals and objectives are best laid out in a systems-based format. The fellowship is a broad-based experience with two primary SICU’s with differing patient populations At the completion of the fellowship the fellow should have acquired the following knowledge and skills.
1.
Respiratory: airway management, including endoscopy and management of respiratory systems.
In additional to what has already been learned while in general surgery training, the resident will acquire additional knowledge of airway management from the SCC faculty who are boarded in Surgery and Anesthesia as well as double boarded in Surgical Critical Care. The SICU service is involved with airway and ventilatory management. Approximately 75% of all patients in the MCLANO West Charity Hospital SICU are intubated and mechanically ventilated at any given time so there is ample patient exposure. Once the patient’s primary service and the SICU service have determined a patient management plan, most of the moment-to-moment ventilator management decisions are made by the SICU service. The indications for and techniques of intubation and bronchoscopy are taught on rounds and in patient management situations. In addition, during the SICU rotation the SCC resident will have access to the METI
Human Patient Simulator to enhance competencies and airway management, mask ventilation, tracheal and bronchial intubation, cricothyotomy, and transtracheal jet ventilation. The SCC resident will also have the opportunity to rotate through Anesthesia as an elective.
2.
Circulatory : invasive and noninvasive monitoring techniques, including transesophageal and precordial cardiac ultrasound and application of transvenous pacemakers; computations of cardiac output and of systemic and pulmonary vascular resistance; monitoring electrocardiograms and management of cardiac assist devices. Swan-Ganz catheters (continuous cardiac output, oximetric, right ventricular end-diastolic volume) are commonly used in our SICU. Placement of these catheters, interpretation of the data obtained from them, and patient management based on hemodynamic information obtained from these catheters are daily events taught by the SCC faculty during work and teaching rounds.
Monitoring and interpretation of 12-lead electrocardiograms and rhythm strips on the physiologic monitors are performed daily on every patient in the SICU. At the VA Hospital and MCLANO East-University Hospital cardiac ultrasound
(transesophageal and precordial), and intra-aortic balloon pumps are used. The
SCC resident is exposed to all of these devices and should be skilled in their use by the completion of his/her SCC residency.
3.
Neurological: the performance of complete neurological examinations; use of intracranial pressure monitoring techniques and of the electroencephalogram to evaluate cerebral function; application of hypothermia in the management of cerebral trauma. All patients with multi organ injury including neurosurgery
trauma patients needing critical care services at MCLANO West Charity Hospital are admitted to the SICU. Intracranial pressure monitoring is common as well as practicing the techniques of lowering intracranial pressure. EEG technology is used in a variety of patients in the SICU including patients undergoing carotid vascular procedures, head trauma, questions of brain death, etc. As such, the SCC resident and the SICU service learn to perform complete neurologic examinations and use the above-mentioned technology.
4.
Renal: the evaluation of renal function; peritoneal dialysis and hemofiltration; knowledge of the indications and complications of hemodialysis. Renal failure and dialysis (whether peritoneal, hemo-dialysis or A-V hemofiltration) are discussed on rounds and in small group discussions with the focus being on the indications for dialysis and the differences between the various techniques available. The primary service and SICU service make the decision to consult the renal service. The SICU service monitors responses to dialysis and in conjunction with the renal service selects the method of dialysis and adjusts modality as needed. The renal service administers dialysis or hemofiltration when a patient requires such.
5.
Gastrointestinal: utilization of gastrointestinal intubation and endoscopic techniques in the management of the critically ill patient; application of enteral feedings; management of stomas, fistulas, and percutaneous catheter devices.
Indications, techniques and complications of gastrointestinal tubes are discussed with all surgical Critical Care and general surgery residents. Upper and lower gastrointestinal endoscopy are available and utilized in the SICU for such problems as upper GI bleeding, questions of bowel ischemia, placement of feeding tubes, etc. Virtually all patients in the SICU for longer 48-72 hours receive nutritional supplementation. Stomas and fistulas are common in our general surgical patient population and the SCC resident learns management techniques and skills in dealing with these problems. Also, nutrition in critically ill patients, stress ulceration and bleeding, and fluid/electrolyte management of fistulas are all topics covered in the small group discussions and on rounds.
6.
Hematologic: application of autotransfusion; assessment of coagulation status; appropriate use of component therapy. Various autotransfusion devices are available in the SICU and utilized when appropriate. The indications for their use, evaluation of coagulation parameters, and the use of blood and blood products are discussed on rounds and in small group discussions. Because of our trauma patient population, coagulopathies are common and the SCC resident on the SICU service will become an expert in their diagnosis and treatment.
7.
Infectious disease: classification of infections and application of isolation techniques, pharmacokinetics, drug interactions, and management of antibiotic therapy during organ failure; nosocomial infections; indications for applications of hyperbaric oxygen therapy. The diagnosis and management of infections is one of the central themes of our SICU. Additionally, with the increasing
incidence of tuberculosis and hepatitis the practice of universal precautions have heightened our awareness of isolation techniques. The issues of diagnosis and treatment of infections and other ancillary techniques such as isolation, hyperbaric oxygen, pharmacokinetics, etc. are dealt with on rounds, in small group discussions, in conferences, and in Journal Club. We expect our SCC resident to become an expert in those areas.
8.
Nutritional: application of parenteral and enteral nutrition; monitoring and assessing metabolism and nutrition. As indicated above, most patients in the
SICU receive nutritional supplementation if they remain in the SICU more than 2-
3 days. The SICU service performs an assessment of every patient’s nutritional needs daily and helps to determine the best means of achieving the nutritional goals. The SICU service is responsible for placing most of the feeding tubes and central venous catheters used for nutritional support. In addition, the SCC resident will participate in a week-long LSUHSC senior clinical nutrition course.
The course outline is presented below.
9.
Monitoring/bioengineering : use and calibration of transenducers, amplifiers, and recorders. The SCC resident will receive continuous instruction on the use of bedside calibration of transducers and setting up systems for intravascular hemodynamic monitoring as well as how to handle problems at the patientmachine interface.
1.
Cardiothoracic-respiratory resuscitation
All residents applying to the Surgical Care Residency Program must start with ACLS and
ATLS certification. If not certified, certification classes can be taken the week prior to the start of the training program. With certification the SCC resident assumes the leadership management role for all cardiopulmonary resuscitation in the SICU until the primary surgeon arrives.
2.
Physiology, pathophysiology, diagnosis, and therapy of disorders of the cardiovascular, respiratory, gastrointestinal, genitourinary, neurologic, endocrine, musculoskeletal, and immune systems as well as of infectious diseases.
The surgical critical care residency will encompass the practice of total patient care.
Furthermore, the SICU/SICA admits patients from all surgical disciplines. Charity
Hospital, a MCLANO primary teaching center is the Level 1 trauma center for Southern
Louisiana. It affords optimal conditions for complete management of the injured patient.
Both units also admit patients with urologic, neurosurgical, and ENT disorders.
Although there is no trauma at the VA, there is good general and cardio-thoracic exposure, as well as admission of patients with urologic, neurosurgical, and ENT ailments. Therefore, the SCC residents will be exposed to and care for a variety of patients with complex musculoskeletal, neurologic and other traumatic injuries. Daily work rounds/teaching rounds are run on an organ system approach. This requires review of basic physiology and pathophysiology of each organ system.
3.
Metabolic, nutritional, and endocrine effects of critical illness.
Nutrition and Metabolic discussions will occur on a daily basis during work and teaching rounds. Support in developing nutritional expertise for critically ill patients is given from the Nutrition Department and a Registered Dietician rounds with the team three times weekly. The Pharm D also rounds three times weekly and has added qualifications in nutritional support in the critically ill.
4.
Hematologic and coagulation disorders
Due to Charity’s status as a Level 1 trauma center, a large number of complex hematologic and coagulation disorders are seen. Topics on coagulopathy and its treatment are discussed on daily work and teaching rounds as well as small group discussions utilizing textbooks and other educational materials.
5.
Critical obstetric and gynecologic disorders
Pregnant patients who suffer traumatic injuries receive care in the SICU prior to stabilization and transfer to University Hospital. The SICU team monitors and manages medical problems with the mother and fetus with help from the Obstetrics/Gynecology team. An agreement to consult with the SCC team for obstetric/gynecologic critical care has been arranged. The SCC Fellow will also attend lectures regarding the care of the critically ill Ob/Gyn patient given by the attending staff in that department.
6.
Trauma, thermal, electrical and radiation injury
Over 4000 trauma patients are seen and 2500 admitted to Charity Hospital of New
Orleans yearly with most requiring complex decision making processes. The SICU/SICA admits about 45 burn patients yearly with the more significant burn injuries being transported to Baton Rouge General Burn Center. Often serious burn trauma cases are admitted to the SICU and stabilized under the SCC resident and attending prior to transport to the Baton Rouge Burn Center. The Baton Rouge Burn Center admits over
250 burn patients per year and the resident has the option to work at the Burn Center as an elective.
7.
Inhalation and immersion injuries
Over the course of a year, Charity hospital of New Orleans admitted 13 inhalation injuries and 4 near-drownings to the SICU/SICA areas. The Critical Care Fellow will be
intimately involved in caring for these patients in conjunction with the primary team and the Critical Care attending. If the resident chooses he may get more exposure to inhalation injuries by taking the Burn Center elective. These topics are also discussed on rounds and in small group sessions.
8.
Monitoring and medical instrumentation
The SCC resident will manage the invasive and non-invasive monitoring equipment in each ICU rotated through. Education concerning patient care interfaced with machines is an integral part of the SCC residency program. Special attention is given to the education in the proper use of Swanz-Ganz catheters, central venous pressure monitors, intracranial pressure monitoring devices, arterial-lines, and capnography.
9.
Critical pediatric surgical conditions
As noted previously, the medical center is a Level 1 trauma center. A large number of critically ill pediatric trauma patients are managed in the SICA in conjunction with the pediatric ICU and general surgery service. The SCC resident acts in consultation to the primary service. Supplemental teaching in pediatric critical care is taught via textbooks, other published materials, didactic discussions, and interactions with the Pediatric
Intensive Care Service.
10.
Pharmacokinetics and dynamics of drug metabolism and excretion in critical illness
A PharmD is dedicated full time to the SICU units and makes daily work and teaching rounds with the critical care team 3 to 4 times weekly. Pharmacokinetics and drug metabolism are discussed daily during bedside rounds. These formal and informal rounding lectures are supplemented by formal lecture series.
11.
Ethical and legal aspects of surgical critical care
Ethical and legal aspects of surgical critical care will be discussed daily during work and teaching rounds. On a case-by-case basis end of life and no code orders are tracked. The
SCC resident will be encouraged to interact with patient family members, other healthcare professionals and primary surgical teams in the decision making process for no code and end of life situations. In addition, ethical and legal aspects of surgical critical care will be enhanced by Dr.’s Hunt and Harrison’s continued teaching involvement in the ethics course sponsored by LSUHSC College of Medicine.
12.
Principles and techniques of administration and management
The SCC resident will participate in all administrative and management decisions concerning the SICU/SICA. This includes the quality assurance issues, quality outcomes meeting and quality improvement endeavors. The SCC resident is also expected to update and improve existing protocols under attending supervision. It is expected that this knowledge will prepare the SCC resident to direct a surgical critical care unit after
completion of this program.
13.
Biostatistics and experimental design
The SCC Journal Club serves as a venue to examine biostatistics and experimental design. Statistical and experimental design techniques are discussed. The SCC resident will also participate in a clinical research project under supervision of a SCC attending during the program year. The intent of this research project is to give the resident first hand experience with statistical methodologies and experimental design as well as the planning and execution of a research project.