Malignant
advertisement
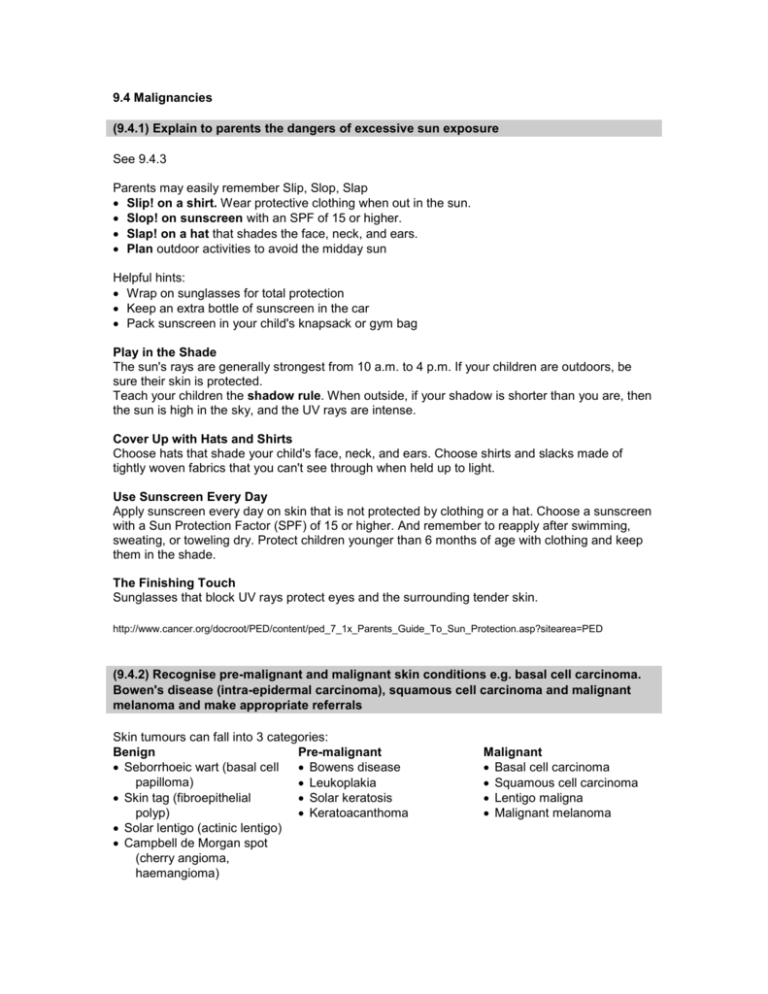
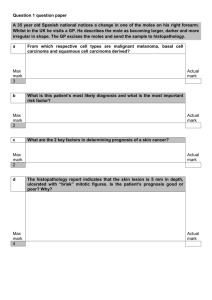
9.4 Malignancies (9.4.1) Explain to parents the dangers of excessive sun exposure See 9.4.3 Parents may easily remember Slip, Slop, Slap Slip! on a shirt. Wear protective clothing when out in the sun. Slop! on sunscreen with an SPF of 15 or higher. Slap! on a hat that shades the face, neck, and ears. Plan outdoor activities to avoid the midday sun Helpful hints: Wrap on sunglasses for total protection Keep an extra bottle of sunscreen in the car Pack sunscreen in your child's knapsack or gym bag Play in the Shade The sun's rays are generally strongest from 10 a.m. to 4 p.m. If your children are outdoors, be sure their skin is protected. Teach your children the shadow rule. When outside, if your shadow is shorter than you are, then the sun is high in the sky, and the UV rays are intense. Cover Up with Hats and Shirts Choose hats that shade your child's face, neck, and ears. Choose shirts and slacks made of tightly woven fabrics that you can't see through when held up to light. Use Sunscreen Every Day Apply sunscreen every day on skin that is not protected by clothing or a hat. Choose a sunscreen with a Sun Protection Factor (SPF) of 15 or higher. And remember to reapply after swimming, sweating, or toweling dry. Protect children younger than 6 months of age with clothing and keep them in the shade. The Finishing Touch Sunglasses that block UV rays protect eyes and the surrounding tender skin. http://www.cancer.org/docroot/PED/content/ped_7_1x_Parents_Guide_To_Sun_Protection.asp?sitearea=PED (9.4.2) Recognise pre-malignant and malignant skin conditions e.g. basal cell carcinoma. Bowen's disease (intra-epidermal carcinoma), squamous cell carcinoma and malignant melanoma and make appropriate referrals Skin tumours can fall into 3 categories: Benign Pre-malignant Seborrhoeic wart (basal cell Bowens disease papilloma) Leukoplakia Skin tag (fibroepithelial Solar keratosis polyp) Keratoacanthoma Solar lentigo (actinic lentigo) Campbell de Morgan spot (cherry angioma, haemangioma) Malignant Basal cell carcinoma Squamous cell carcinoma Lentigo maligna Malignant melanoma 9.4: Skin Malignancies 2 Benign Lesions Seborrhoeic wart (basal cell carcinoma) Dangerous differential Often familial and common in both sexes in middle age + Usually on trunk Increases in number and size with age Yellow-brown / black and greasy with a rough craggy edge Note the two distinct shades in the melanoma Solar lentigo (senile or actinic lentigo) From excessive exposure to sunlight Light brown macules – often multiple – occurring on light-exposed skin Campel de Morgan spot Skin tag Often familial and common in both sexes middle age + Often familial. May arise with obesity / pregnancy Multiple, small, bright red spots. Trunk Multiple soft, round and peduncular Typically neck, axillae and groins Often with seb. warts 9.4: Skin Malignancies 3 Premalignant conditions Prev exposure to UVL / arsenic or other carcinogens Ulceration suggests invasive growth Chronic exposeure to UV Backs of hands, forehead, scalp, temples, nose, cheeks and ears Rough adherent crusts on erythematous base Anywhere on the skin Asymptomatic, erythematous, welldemarcated, scaly White patches on mucosal surface Mainly middle aged, on areas exposed to sun Flesh coloured papule enlarges rapidly over 8-10 weeks with central keratin-filled crater 9.4: Skin Malignancies 4 Malignant conditions: Melanoma The majority of malignant melanomas are brown-to-black pigmented lesions. Warning signs include change in size, shape, color, or elevation of a mole. The appearance of a new mole during adulthood, or new pain, itching, ulceration, or bleeding of an existing mole should be checked. The following easy-to-remember guideline, “ABCD,” is useful for identifying malignant melanoma: Asymmetry - One side of the lesion does not look like the other. Border irregularity - Margins may be notched or irregular. Color - Melanomas are often a mixture of black, tan, brown, blue, red, or white – see below for some pictures) Diameter - Cancerous lesions are usually larger than 6 mm across (about the size of a pencil eraser), but any change in size may be significant. Note that some lesions have little black pigment - all those shown have changes in colouration across the lesion. 9.4: Skin Malignancies 5 Lentigo Maligna Intraepidermal, pre-invasive malignant melanoma in middle age + Most commonly on the face Starts as flat brown stain with irregular but well-demarcated edge. Slowly enlarges with variable pigmentation May lead to nodular malignant melanoma Basal cell Carcinoma (BCC, rodent ulcer) Squamous cell carcinoma (SCC) Chronic sun damage / exposure to arsenics or radiotherapy in middle age + Chronic sun damage / industrial carcinogens or longstanding ulcers predispose Common. Very slow growing (years) Pearly rolled edge Central ulceration May occur de novo or with a backgound of solar keratosis, Bowens disease or leukoplakia Commonest on hands and face – esp lower lip and ear 9.4: Skin Malignancies 6 (9.4.3) Describe the mechanisms by which ultra-violet light leads to the development of skin malignancies http://dermatology.about.com/cs/beauty/a/suneffect.htm What is UV Radiation? The sun gives off ultraviolet radiation that we divide into categories based on the wavelength. UVC - 100 to 290 nm: almost completely absorbed by the ozone layer UVB - 290 to 320 nm: affects outer layers of skin - responsible for sunburn. Does not penetrate glass. UVA - 320 to 400 nm: penetrates deep into the skin (melanocytes are deep cells), more constant than UVB without the variations during the day and throughout the year. Penetrates glass. Carcinogenic Effects of UVA and UVB: Free Radicals: UV radiation is one of the major creators of free radicals. Free radicals are unstable oxygen molecules that have only one electron instead of two. Because electrons are found in pairs, the molecule must scavenge other molecules for another electron. When the second molecule looses its electron to the first molecule, it must then find another electron repeating the process. This process can damage cell function and alter genetic material. Free radical damage causes wrinkles by activating the metalloproteinases that break down collagen. They cause cancer by changing the genetic material, RNA and DNA, of the cell. DNA Repair: UV radiation can affect enzymes that help repair damaged DNA. Immune System Effects: The body has a defense system to attack developing cancer cells. These immune system factors include white blood cells called T lymphocytes and specialized skin cells in the dermis called Langerhans cells. When the skin is exposed to sunlight, certain chemicals are released that suppress these immune factors. Cell Death: The last line of defense of the immune system is apoptosis. There are certain factors, including UV exposure, that prevent this cell death allowing cells to continue to divide and possibly become cancerous. In addition, UV radiation causes collagen to break down at a higher rate than with just chronologic aging. Sunlight damages collagen fibers and causes the accumulation of abnormal elastin resulting in wrinkles, and aging skin disorders. It is worth mentioning these to patients as many care more about this than the possibility of cancer! 9.4: Skin Malignancies 7 Examine a patient with skin malignancy with particular reference to the detection of spread of the disease As well as examination and recording (photography + ruler) of the dimensions of the lesions, the relevant lymph nodes must be examined for lymphadenopathy. Describe to patients in outline the potential benefits and possible side effects of surgery and radiotherapy To be done soon Surgery Benefits Side-effects Benefits Radiotherapy Side-effects Work with primary care, hospice and Macmillan nurse services in the care of patients with disseminated skin malignancy