Treatment of Keratitis (see references 2 & 3)
advertisement

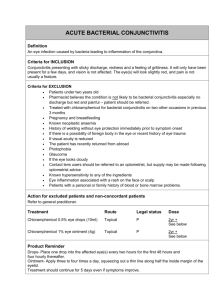
The Red Eye and Selected Ocular Emergencies Thursday May 28, 2009 American College Health Association 2009 Annual Meeting San Francisco, CA Supplemental Handout Frederick H. Bloom, O.D. Director, Eye Care Services University Health Services University of Massachusetts Amherst, MA 01003 413-577-5383 fbloom@uhs.umass.edu 1 Guidelines for Treatment of Conjunctivitis Bacterial Conjunctivitis (other than chlamydial conjunctivitis) - Prescribe a broad spectrum topical antibiotics Tobrex drops– 1 drop 4 x day x 7 days or Polytrim drops – 1 drop every 3 hrs up to maximum dose of 6 x day x 7 days (approved for greater than 2 months of age) Ilotycin ointment (Erythromycin ointment) – apply 4 x day x 7 days (most patients do not like ointment as it blurs vision) *Vigamox – 1 drop 3 x day x 7 days *Zymar -1 drop every 2 hours (days 1 and 2) then 1 drop 4 x day (days 3 to 7) * It is recommended to reserve 4th generation fluoroquinolones, Vigamox and Zymar, for keratitis, corneal ulcers, or contact lens wearers with suspicion of keratitis; approved for use in people greater than 1 year of age Note: If you decide to prescribe a fluoroquinolone, it is recommended to prescribe a 4th generation fluoroquinolone rather than, the less expensive, 2nd or 3rd generation fluoroquinolones such as Ocuflox, Ciloxan, and Quixin, due to the 4th generation fluoroquinolones’ enhanced drug delivery capabilities, the improved activity against gram positive bacteria, and their lowered likelihood of causing resistance. Chlamydial Conjunctivitis Adult Inclusion Conjunctivitis Laboratory testing – Aptima Genprobe Assay (proprietary test of Genprobe – uses TMA transport mediated amplification – DNA probe looking for RNA target (very specific) Systemic antibiotics: Azithromycin 1G x 1 day single dose by mouth, Doxycycline 100mg orally 2 x day x 14 days or Erythromycin 500 mg orally 4 x day x 14 days to patient and sexual partners Topical medication (erythromycin ophthalmic ointment) 4 x per day x 3 weeks * Tetracyclines are contraindicated in children under 8 years, pregnant women, and nursing mothers Warm compresses 2 Viral Conjunctivitis - Educate the patient in appropriate infection control and hygiene to prevent the spread of the infection to others Apply appropriate infection control procedures in your office to prevent spread of the infection to you, your staff and your other patients Warm or cold compress, artificial tears, decongestant/antihistamine (Naphcon A) Adjunct po medications Allergic Conjunctivitis Avoidance Cold compress OTC artificial tear lubricants (Eye wash or Theratears or Genteal or Systane eye drops) 1 drop 4 x day OTC Vasoconstrictors (e.g. visine or murine) Topical antihistamines?, otc: Zaditor or Alaway (ketotifen fumarate) Vasoconstrictor/Antihistamines (Naphcon A) 1 drop 4 x per day Oral antihistamines – beware of ocular dryness side effect Topical Mast cell stabilizers/Antihistamines: Patanol (Olopatadine 0.1%) 1 drop 2 x day at intervals of 6 to 8 hrs and Pataday (Olopatadine 0.2%) 1 drop 1 x per day each eye * Non-steroidal anti-inflammatory agents (Ibuprofen or topical Acular LS 0.4%. However, topical Acular LS (1 drop 4 x per day) is generally not comfortable for patients with allergic conjunctivitis and I generally do not prescribe Acular for allergic conjunctivitis Steroids – refer In very mild cases of allergic conjunctivitis, when it seems appropriate for the patient to wear contact lenses for short periods, it is recommended that patients wait 10 to 15 minutes after instilling Patanol/Pataday, Naphcon A, or other eye drops before inserting their contact lenses 3 Recommendations for Culturing and Lab Testing for Most Conjunctivitis Routine bacterial culturing of conjunctivitis is not recommended. However, it is recommended in cases of conjunctivitis not responding to standard treatment after 2-3 weeks, recurrent conjunctivitis, or severe purulent conjunctivitis Chlamydial assaying (Aptima/Genprobe - transport mediated amplification (proprietary test of genprobe) uses a DNA probe looking for RNA target, very specific, for Chlamydia Trachomatis and Neisseria Gonorrhoeae) is also recommended in cases of chronic follicular conjunctivitis i.e. lasting longer than 2-3 weeks in individuals who are sexually active Conjunctivitis Pearls • A red eye with pain, tearing, and/or decreased vision is usually not conjunctivitis • Chronic follicular conjunctivitis, greater than 2 weeks, especially in sexually active individuals, rule out chlamydial conjunctivitis, check sexual partners – genital symptoms, asymptomatic at least 50% of time • Preauricular adenopathy is usually viral although can be present in acute hordeolum • Systemic medications: e.g. Ask if patient is taking Accutane – rule out dry eye, conjunctivitis, night vision problems • Medicamentosa – e.g. Aminoglycocides (Tobrex, Gentamicin, Neomycin) toxic to cornea • Remember hygiene for patient and you; advise patients to wash hands if they touch their eyes, use a separate towel or pillow at home, don’t wear or share make-up, and don’t go swimming 4 Classical Presentation of the Differential Diagnosis of the Red Eye CONJUNCTIVITIS Viral INCIDENCE Bacterial IRITIS ACUTE GLAUCOMA KERATITIS* EPISCLERITIS SCLERITIS Common Uncommon Extremely common Uncommon Allergic Extremely Common Serous Mucopurulent Whitish, stringy, ropy mucus Watery Watery Watery Usually none Grittiness Grittiness Itching Pain, Photophobia Severe pain, photophobia, vomiting Moderate pain, photophobia Varies Most common causes: Staphylococcus aureus Streptococcus pneumoniae Haemophilus species - Papillae often present - May have chemosis (swelling of conjunctiva) R/O allergy to medication R/O chemical injury (usually obvious by Hx) Not blurred Usually slightly blurred Markedly blurred May be blurred Usually not affected initially Conjunctival or Diffuse Ciliary Diffuse Ciliary Segmental or diffuse Clear, if pure conjunctivitis Keratitic, precipitates Steamy, corneal edema Not clear, possible infiltrates or staining Usually clear initially PUPIL SIZE Normal Usually small (miotic) Can have traumatic mydriasis (dilated) Mid-dilated Normal Normal PUPILLARY LIGHT RESPONSE Normal Poor Fixed, no response Normal Normal Normal (Don’t do on infected eye) Normal to low Elevated Normal Normal Normal Cells and flares Shallow Normal Clear DISCHARGE DISCOMFT OR PAIN - Follicles often present COMMENTS - Often has tender preauricular adenopathy - May have URI VISION INJECTION CORNEA INTEROCULAR PRESSURE ANTERIOR CHAMBER Always compare 2 eyes * For the purpose of this chart, keratitis refers to any inflammation or infection of the cornea: corneal abrasions, corneal inflammations, corneal ulcers that could be bacterial, viral including herpes simplex with the classic epithelial dendritic staining, herpes zoster, fungal, or parasitic such as acanthemoeba, or even sterile inflammations Note: There may be reduced corneal sensitivity with herpes simplex keratitis and with herpes zoster if the tip of the nose is involved usually there is a higher risk of ocular involvement due to the distribution of the nasociliary branch of the ophthalmic division of the trigeminal, fifth cranial nerve 5 Treatment of Keratitis - (see references 2 & 3) In general, refer to eye doctor after initial treatment Bacterial Keratitis * - “Small Infiltrates (<2 mm): broad spectrum topical antibiotic (gatifloxacin [Zymar], moxifloxacin [Vigamox], or Levofloxacin 1.5% [Iquix] q1h initially, then taper slowly) - Large ulcers >2mm and/or more central corneal ulcers should be referred for culturing and more aggressive medical treatment * The most common causes of bacterial keratitis are staphylococcus, streptococcus, pseudomonas, and moraxella species Viral Keratitis - “HSV Epithelial Keratitis: Refer to eye doctor. Topical antiviral (trifluridine [Viroptic] (the treatment recommended for viroptic is 9 times/day but many doctors start at 5 times/day because it has been shown to be equally effective and less toxic in most cases) 9 times/day or vidarabine monohydrate [Vira-A] 5 times/day for 10-14 days; consider oral antiviral agent (acyclovir 400mg po tid for 10-21 days, then prophylaxis with 400mg bid for up to 1 year [or longer after penetrating keratoplasty]), ? debride dendrite.” - “HZV: Refer to eye doctor. Systemic antiviral agent (acyclovir 800 mg po 5 times a day for 7-10 days, or famciclovir 500 mg po or valacyclovir 1 g po tid for 7 days), topical steroids (prednisolone acetate 1% qid to q4h, then taper slowly over months), cycloplegic agent (scopolamine 0.25% bid to qid); add topical antibiotic ointment (erythromycin or bacitracin tid) if conjuctival or coneal involvement. Consider tricyclic antidepressants, Neurontin, pain medications, capsaicin cream, or Lidoderm patches for postherpetic neuralgia.” - May require treatment of increased inter ocular pressure Sterile Keratitis - Symptoms usually less severe, infiltrate often more peripheral cornea - Treatment similar to bacterial keratitis Fungal Keratitis* - Satellite lesions surrounded by primary lesion, associated with vegetative corneal abrasion, especially in corneal abrasion and some contact lens solution - Treatment – Natomycin 5% or Amphotericn B (additional treatment beyond the scope of this talk) 6 Acanthomoeba Keratitis* (parasite) - Associated with contact lens wear; hot tub use?, swimming in fresh water? - At 3 to 8 weeks corneal stromal ring infiltrates (treatment beyond scope of this talk) * more rare Clinical Pearls With a corneal ulcer there is often a presence of an infiltrate – loss of clarity of cornea- white patch representing cellular inflammation - Discontinue contact lens wear - Never patch a corneal ulcer - There is a greater risk of gram negative infection with contact lens wear, and with keratitis compared with conjunctivitis, therefore cover with anti-pseudomal eye medication e.g. Vigamox or Zymar - Cycloplegics may be needed (usually used sparingly as they may have a big impact on patient functions) - P.O pain medication may be needed - Immunosuppressant patients are at greater risk of infection - Smokers and contact lens wearers are at a greater risk of keratitis - Contact lens wearers who sleep in contact lenses have a 10x greater risk of infection - Ulcers require daily follow-up initially, and severe ones require hospital admission. Most keratitis at UHS is relatively mild and can be treated with 4th generation fluoroquinolones e.g. Vigamox or Zymar, usually hourly initially - If organism is in doubt, treat as a bacterial ulcer until culture results return 7 Table 1: Antivirals Mechanism of Action (MOA): Inhibit DNA replication Generic acyclovir valacyclovir famciclovir Trade Zovirax (GlaxoSmithKline) Valtrex (GlaxoSmithKline) Famvir (Novartis) Formulations 200mg capsule; 400mg and 800mg tablets; 200mg/5ml suspension 500mg 1000mg (1g) caplets 125mg 250mg 500mg tablets Condition VZV Dosage 800mg 5x/d for 7 to 10 days HSV 400mg 5x/d for 7 days HSV (pediatric) 20mg/kg/d divided q.i.d. for 7 days HSV prophylaxis 400mg b.i.d. VZV 1g t.i.d. for 7 to 10 days HSV 500mg t.i.d. for 7 days HSV prophylaxis 500mg *once per day VZV 500mg t.i.d. for 7 to 10 day HSV 250mg t.i.d. for 7 days HSV prophylaxis 250mg b.i.d. The information in the tables is meant as a guide and is intended for healthy adults who have no contraindications to the medication. Review of Optometry MAY 15, 2005 and *amended after discussion with Jimmy D. Bartlett, OD April 26, 2009 8 Anterior Uveitis (Iritis, Iridocyclitits) (see references 2 & 3) Possible Symptoms – red eye, pain, photophobia, decreased vision Possible Signs – cells and floaters in anterior chamber, ciliary flush, and keratic precipitates, or high intra ocular pressure, and usually miosis, unless traumatic mydriasis, eye pain if shine a light in the non involved eye usually from ciliary spasm “Classifications – acute, chronic, recurrent granulomatous vs. non granulomatous traumatic vs. non traumatic location in uveal tract Etiology – Most commonly idiopathic or autoimmune, but it is critical to rule out causes such As infection, malignancy, medication, and trauma - Idiopathic - Traumatic - Herpes simplex and Herpes Zoxter Ophthalmicus - Lyme Disease - Syphilis - Tuberculosis - HLA- B27 associated anterior uveitis o Ankylosing Spondylitis o Reiter’s Syndrome o Psoriatic Arthritis o Inflammatory Bowel Disease - Whipple’s Disease - Behcet’s disease (acute) - Glaucomatocyclitic crisis (Posner-Schlossman syndrome, acute) - Kawasaki’s disease (acute) - Drug use (acute) - Interstitial nephritis - Other autoimmune disease (acute and chronic) - Juvenile rheumatoid arthritis (chronic) - Fuchs’ heterochromic iridocyclitis (chronic) - Postoperative or trauma (chronic) - HLA associations (located on chromosome 6) - Sarcoid” Treatment - Refer to the eye doctor for consideration of the following: - Topical steroids Cyclopegics Treat elevated intra ocular pressure PO NSAI PO steroids and/or subtenon steroid injection Treat underlying systemic disease Immunosuppression chemotherapy and other treatment Prognosis Depends on etiology. Most have good visual prognosis. Traumatic iritis is generally easier to treat unless there is concomitant ocular injury to other structures 9 Papilledema (may be life threatening) (see references 2,3 & 4) Definition Optic nerve swelling caused by increased intracranial pressure Symptoms Asymptomatic; may have headache, nausea, emesis, transient visual obscurations (lasting seconds), diplopia, altered mental status, or other neurologic deficits Signs Critical. Bilaterally swollen, hyperemic discs, blurred disc margins and elevated discs, And the absence of optic cup. Other. Papillary or peripapillary retinal hemorrhages (often flame shaped); loss of venous Pulsations (20% of the normal population do not have venous pulsations); dilated, Tortuous retinal veins; loss of physiological cup, concentric folds or lines Management: Refer and/or work up stat as an emergency and then treat underlying cause Etiology of Papilledema – optic nerve swelling due to increased intracranial pressure - Primary and metastatic intracranial mass Pseudotumor cerebri (often occurs in young, overweight females) (idiopathic intraocular hypertension) Aqueductal stenosis producing hydrocephalus Subdural and epidural hematomas (From trauma) Subarachnoid hemorrhage Arteriovenous malformation Brain abscess Meningitis Encephalitis Intracranial venous sinus thrombosis Differential Diagnosis of other causes of disc swelling without increased intracranial pressure - Pseudopapilledema Papillitis Hypertensive optic neuropathy Central retinal vein occlusion Ischemic optic neuropathy Optic disc vasculitis Infiltration of the optic disc Leber optic neuropathy Orbital optic nerve tumors Diabetic papillitis Graves ophthalmopathy Uveitis 10 Optic disc swelling in a patient with a history of leukemia is often a visually threatening sign of leukemic infiltration of the optic nerve. Immediate radiation therapy is usually required to preserve vision” Clinical Pearls: - papilledema is a medical emergency - work up stat - approximately 80% of the normal population has spontaneous venous pulsations (SVP) - SVP usually disappears at approximately 225mm water cerebral spinal fluid pressure. The opening pressure reading as measured by lumbar puncture (always preceded by a head scan to rule out a true mass) in patients with benign intracranial hypertension (a.k.a pseudo tumor cerebri) is usually between 250 and 600 mm H20 - loss of previously seen SVP is the earliest ophthalmoscopic sign of papilledema - papilledema may develop over 8 to 24 hours and the optic nerve swelling usually slowly decongests over a number of weeks or months” - Not all cases of pseudo tumor cerebri are in overweight women, in fact, most of the cases I have seen at the UHS were not in overweight women. Rule out that pseudo tumor cerebri is not caused by some systemic medication e.g. tetracycline 11 References 1. Duane’s Clinical Ophthalmology. New York: Lippincott Williams, & Wilkins. 2. Kaiser MD, Peter, Neil Friedman, MD, & Roberto Pineda II, MD. The Massachusetts Eye and Ear Infirmary Illustrated Manual of Ophthalmology. Philadelphia: Saunders, 2004. 3. Kunimoto, MD, Derek, Kunal Kanitkar, MD, & Mary Makar, MD. The Willis Eye Manual. Philadelphia: Lippincott Williams & Wilkins, 2004. 4. Smith, MD, J. Lawton. The Optic Nerve. Miami: Neuro-Ophthalmology Tapes, 1995. 5. My own clinical experience of seeing over 100,000 patients over 30 years and consulting with over 35 ophthalmologists (for patients I referred). Many of those 35 ophthalmologists have sub specialties in cornea, pediatric ophthalmology, strabismus, uveitis, cataract surgery, retina, oculo plastics and orbits, laser refractive surgery, and neuro ophthalmology 6. American Academy of Ophthalmology Cornea/External Disease Panel. (2003) “Preferred Practice Pattern: Conjunctivitis.” American Academy of Ophthalmolgy 7. American Optometric Association Consensus Panel on Care of the Patient with Conjunctivitis. (2002) “Care of the Patient with Conjunctivitis” American Optometric Association 8. The Willis Eye Manual, Office and Emergency Room Diagnosis and Treatment of Eye Disease. Kunimoto et al. Lippincott Williams & Wilkins, 2004. 9. The Massachusetts Department of Public Health – Division of STD Prevention – 2006 Sexually Transmitted Diseases Treatment Guidelines 10. Huang, David G. (2004). “Fluoroquinolone Resistance in Ophthalmology and the Potential Role for Newer Ophthalmic Fluoroquinolones.” Survey of Ophthalmology, 49, Supplement 2, S79. 11. Parmar, Pragya, Amjad Salman, Catti Munusamy Kalavathy, Jayaraman Kaliamurthy, Duraisamy Arvind Prasanth, Philip Aloysius Thomas, and Christdas Arul Nelson Jesudasan. (2006). “Comparison of Topical Gatifloxacin 0.3% and Ciprofloxacin 0.3% for the Treatment of Bacterial Keratitis.” Am J Ophthalmology, 141, 282-286. Disclosure and acknowledgement of source of colored eye slides: Most of the slides I took myself and were of patients I personally examined. A small number of slides were either lent to me by my colleagues or obtained from MedCom, a professional slide service. Additionally, a few slides were also taken from the World Wide Web to enhance learning. If you have any questions about the sources of the slides, please contact me. Thank you. A special acknowledgement and heartfelt thank you to Emily Wegner, Karen Dunbar-Scully, and Pierre Rouzier M.D. for their excellent and superb assistance with the typing, editing, technical, and clinical aspects of preparing this PowerPoint presentation. 12