CONNECTIVE TISSUE - III: CELLS & FIBERS
advertisement
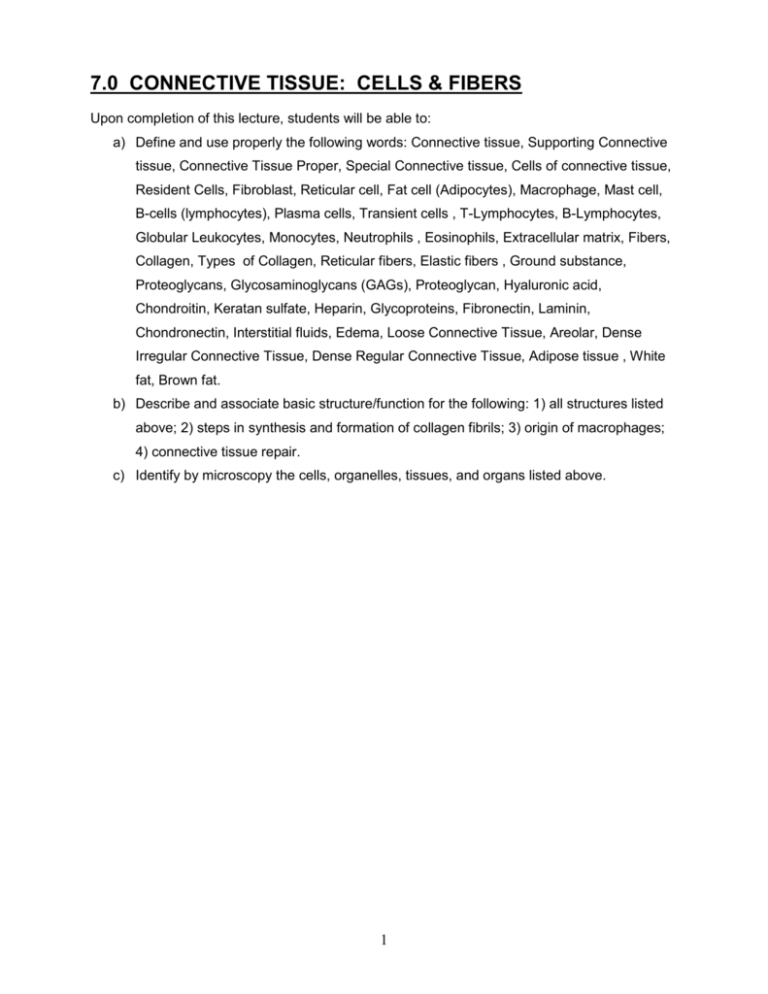
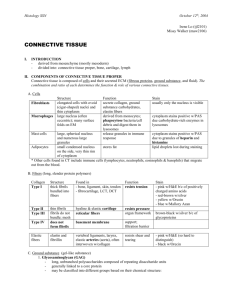
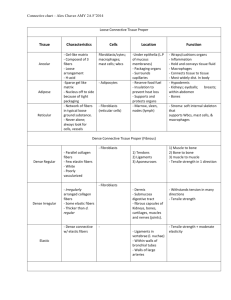
7.0 CONNECTIVE TISSUE: CELLS & FIBERS Upon completion of this lecture, students will be able to: a) Define and use properly the following words: Connective tissue, Supporting Connective tissue, Connective Tissue Proper, Special Connective tissue, Cells of connective tissue, Resident Cells, Fibroblast, Reticular cell, Fat cell (Adipocytes), Macrophage, Mast cell, B-cells (lymphocytes), Plasma cells, Transient cells , T-Lymphocytes, B-Lymphocytes, Globular Leukocytes, Monocytes, Neutrophils , Eosinophils, Extracellular matrix, Fibers, Collagen, Types of Collagen, Reticular fibers, Elastic fibers , Ground substance, Proteoglycans, Glycosaminoglycans (GAGs), Proteoglycan, Hyaluronic acid, Chondroitin, Keratan sulfate, Heparin, Glycoproteins, Fibronectin, Laminin, Chondronectin, Interstitial fluids, Edema, Loose Connective Tissue, Areolar, Dense Irregular Connective Tissue, Dense Regular Connective Tissue, Adipose tissue , White fat, Brown fat. b) Describe and associate basic structure/function for the following: 1) all structures listed above; 2) steps in synthesis and formation of collagen fibrils; 3) origin of macrophages; 4) connective tissue repair. c) Identify by microscopy the cells, organelles, tissues, and organs listed above. 1 CONNECTIVE TISSUE: CELLS & FIBERS I. INTRODUCTION Connective tissues consist of cells separated by an abundance of intercellular material (fibers and ground substance). CT is found in every organ; it surrounds all the other tissue types, and is a general classification for: cartilage, bone, blood, adipose tissue, lymphatic tissue (tissues of the immune system) II. CLASSIFICATION OF CONNECTIVE TISSUES A. Supporting CT 1. Cartilage & Bone 2. support for soft tissues of the musculoskeletal system B. Connective Tissue Proper 1. Loose (areolar, reticular) 2. Dense (Regular, irregular) 3. lies beneath epithelia, binds tissues & organs together C. Special CT 1. Adipose tissue 2. Blood (liquid extracellular matrix 3. Lymphatic tissue (defense of body) 4. Embryonic (Mucous, mesenchyme) II. CELLS OF CONNECTIVE TISSUE RESIDENT Cells that are seeded during development and renew by mitosis or arrive by blood vessels and camp in CT A. Fibroblast 1. elongated cell (stellate) 2. synthesizes Tropocollagen 3. the most common cell of CT proper 4. fibrocytes are the inactive cell type name 5. has prominent RER (basophilia) and a Golgi apparatus 6. can survive anoxic conditions and respond to chronic injury 7. they repair CT matrix by phagocytizing old collagen 8. fibrosis or scarring is caused by excessive production of collagen 9. same as reticular cells, except that reticular cells synthesize a smaller fibril B. Reticular cell (specialized fibroblasts) 1. spindle shaped cells in lymphatic organs (spleen, lymph nodes, thymus) and in hemopoietic tissue (bone marrow) 2. similar to the fibroblast; synthesizes collagen & ground substance 3. reticular fibers are Type III collagen 4. forms a meshwork C. Fat cell 1. Adipocytes are associated with loose CT 2. triglycerides are unbound by a membrane and fill the cytoplasm 2 3. Found in small areas to cushion organs and tissue 4. Found in large areas for energy storage D. Macrophage 1. large cells, often having a foamy appearance with oval to c-shape nucleus 2. blue-gray cytoplasm 3. derived from blood monocytes; 4. often these cells migrate, but others may be fixed in place 5. Location of macrophages: a. Macrophage (CT, lymph nodes, spleen, peritoneum, bone marrow) b. Kupffer cell (Liver) c. alveolar macrophage (lung) d. osteoclasts (bone) e. microglial cells (central nervous system) 6. Functions of the macrophage: a. phagocytize bacteria, foreign particles, and damaged cells b. contains numerous lysosomes with hydrolytic enzymes c. can fuse to form multinucleated giant cells that attempt to wall off foreign bodies. d. Histiocytes (resident macrophages) e. associated with the formation of granulomas f. processes antigens and presents to Plasma cell for antibody production E. Mast cell 1. cytoplasm is filled with large basophilic granules (H&E) 2. Stained with: a. metachromatic stains (purple), PAS (red), or Alcian blue stains for proteoglycans (heparin sulphate) 3. round nucleus sometimes obscured by blue-purple granules 4. derived during development from stem cells in bone marrow or from basophils 5. found in many tissues: i.e. bone marrow, dermis, digestive and respiratory tracts, reproductive tract 6. Mast cell granules contain: a. heparin (anticoagulant; blood clotting problems associated with mast cell tumors) b. chondroitin sulfate c. histamine (causes contraction of smooth muscle.. anaphylactic shock.. bronchioles) d. eosinophilic chemotactic factor F. B-cells (lymphocytes) differentiate into PLASMA cells (antibodies) 1. large cell with a distinct nucleus 2. basophilic cytoplasm 3. prominent Golgi body near the nucleus 4. found at sites susceptible to bacteria & foreign proteins... a. (i.e. intestinal mucosa, respiratory & urogenital tracts) 5. can be transient or resident depending upon their need for immune reaction 3 TRANSIENT CELLS White blood cells that migrate from the blood to the connective tissue (diapedesis)... especially during inflammation... do not move back to the blood, will die in CT or move to the lymphatics often found in normal tissues 1. T-Lymphocytes 1. T cells have a long life (cell mediated immunity) 2. very little cytoplasm, somewhat heterochromatic nucleus 3. also found among epithelial cells 2. B-Lymphocytes 1. differentiate into PLASMA cells (antibodies) 2. large cell with a distinct nucleus 3. basophilic cytoplasm 4. prominent Golgi body near the nucleus 5. found at sites susceptible to bacteria & foreign proteins... a. (i.e. intestinal mucosa, respiratory & urogenital tracts) G. Globular Leukocytes 1. Red granules, round nucleus 2. may be confused with the eosinophil H. Monocytes 1. form macrophages I. Neutrophils 1. Polymorphonuclear leukocytes or PMN 2. dark heterochromatic, segmented nucleus (lobulated) 3. responds to a "chemotactic agent" (endotoxin, cigarette smoke, seminal proteins) 4. migrate (chemotaxis) toward the substance 5. become phagocytic and tries to destroy antigens 6. to prevent macrophages from identifying and processing antigens for plasma cell antibody synthesis 7. can cause abscess (pus) formation 8. has myeloperoxidase enzyme, which is excellent against bacteria J. Eosinophils 1. large red (eosinophilic) granules fill the cytoplasm 2. granules are lysosomes 3. nucleus has 2 lobes 4. increased in CT during allergic and parasitic diseases 5. attracted to CT by Chemotactic Factors released by Mast cells 6. phagocytizes antigen-antibody complexes & stimulates collagen synthesis 7. tunes down the inflammatory response by decreasing Mast cell degranulation K. COMMENT: Transient Cell types will depend upon the CT type and location. The fibroblast is the most common cell and most widely spread and is found nearly everywhere in connective tissues. 4 III. EXTRACELLULAR MATRIX Mostly fibers & ground substance make up the matrix and are found throughout the CT in various concentrations and in various forms. Blood is an exception to the normal form of CT. Blood does not contain collagen fibers (fibrinogen could be considered a soluble fiber) and it has a considerably different ground substance (blood plasma). A. FIBERS: 1) collagen, 2) reticular, 3) elastin a. Collagen: a. most abundant fiber b. most abundant protein of body c. collagen makes up >70% of skin > 90% of bone dry wt d. flexible but tensile strength of steel (1 mm fiber will support 80 lbs) e. Stains PAS+; Eosin +; Masson’s Trichrome stain: collagen + reticular fibers + bone = blue, muscle + cytoplasm = red, nuclei = black f. at least 13 types of collagen, but only 3 produce fibers g. Collagen produced by the fibroblast is a good example of structure/biochemical correlations in a cell: i. Nucleus transcribes the RNA message for pro-collagen that is translated. Hydroxyproline is the marker amino acid. ii. In the RER pro-collagen is synthesized and modified to become the triple-helix tropocollagen molecule iii. In the Golgi apparatus the tropocollagen molecules are further modified by the addition of carbohydrates (glycosylation) and packaged for secretion iv. Secretory vesicles move along microtubular paths to the plasmalemma where tropocollagen is released along with proteases that clip the terminal peptides. v. In the CT the tropocollagen molecules polymerize into the collagen fibril (seen only at the Electron microscopic level). vi. Collagen fibrils grow in size under the influence of organ pressures and surrounding ground substances to form collagen fibers, which then form collagen bundles. Fibroblast h. Types of Collagen (Most important of the 12 types) 5 i. ii. iii. iv. v. I II III IV V skin, bone, tendon, ligament, dentine cartilage reticular collagen basal lamina placenta basement membrane b. RETICULAR FIBERS a. Small diameter collagen fibrils (15-20 nm) of Type III. b. Not stained well, but are PAS+ c. found beneath some basal lamina, surrounds blood vessels d. help to form filters or webs of fibers in bone marrow and lymph nodes c. ELASTIC FIBERS a. arranged randomly b. irregular amorphous in structure c. consists of a protein called elastin d. stains pink with H&E; resorcin fuchsin stains elastin black e. There is an Elastic CT i. (e.g., elastic ligaments of spinal column, large elastic arteries) B. GROUND SUBSTANCE a. General information a. Fills the space between cells and fibers b. forms a viscous barrier, serves as a molecular filter c. functions as a lubricant d. absorbs large amounts of water (which protects joints from stress of impact) e. sometimes lost in processing for Light microscopy (unless frozen) f. components are large molecules of proteins and sugars b. Proteoglycans a. these molecules are sugars with proteins b. Sugars = glycosaminoglycans (GAGs) c. Protein cores = attached to GAGs d. GAGs are repeating disaccharides with one sugar containing an amine group & most are sulphated e. Proteoglycan Structure i. Like a bottle brush... ii. GAGs serving as the bristles... protein as the wire core iii. Hyaluronic acid connects the Linking proteins along the core iv. water is absorbed between the GAG bristles 1. 2. 3. 4. 5. 6. 7. GAGs Hyaluronic acid Chondroitin Chondroitin-4-sulfate Chondroitin-6-sulfate Keratan sulfate Dermatan sulfate Heparin Location most tissues cartilage cartilage, bone cartilage cartilage, bone skin Mast cells of CT 6 8. Heparin sulfate cell surfaces c. Glycoproteins (proteins with sugars) a. Fibronectin : i. synthesized by fibroblasts & epithelial cells.. ii. binding sites for cells, collagen, GAGs b. Laminin: i. located in the basal lamina (Seen only by EM); ii. separates CT from non-CT iii. adhesion of epithelial cells to type IV collagen of basal lamina c. Chondronectin: i. located in cartilage; functions in adhesion IV. TISSUE FLUID Most of interstitial fluids are bound to proteoglycans. They are very important in the movement of water from capillaries. Dehydration of tissues causes damage. In contrast, edema is the enlargement of spaces in CT induced by an increase in water content of interstitial spaces (outside of the cell). V. CLASSIFICATION OF CONNECTIVE TISSUE PROPER A. Loose Connective Tissue 1. Areolar (much space) 2. Highly cellular with loose fibers 3. In some areas can be very high cellularity i. Between epithelia of small intestine ii. Areas where there is exposure to foreign bodies 4. reticular and/or Type I collagen fibers 5. found beneath epithelium; around blood vessels & nerve; between muscle layers; and with fat cells B. Dense Irregular Connective Tissue 1. more fibers than cells 2. Type I collagen fibers 3. thick random weave of collagen fiber bundles 4. the scattered fibroblasts synthesize collagen fibrils 5. found in dermis of skin; capsules of organs; sheaths of nerve and tendon C. Dense Regular Connective Tissue 1. fibers are arranged in parallel arrays (elastic fibers in ligaments) 2. long flat fibroblasts are interspersed between fibers 3. found in tendon and ligaments, capsules of organs 4. Look-a-like: thick smooth muscle bundle (big differences is the string of nuclei) VI. ADIPOSE TISSUE A. White fat 1. very large cells (~200 µm) 2. Signet ring appearance 7 3. partitioned into lobules surrounded by CT 4. sparse blood supply to white fat & little to no innervation 5. subcutaneous (thermal & mechanical insulation); footpad; interspersed in B. Brown fat 1. smaller cells 2. many lipid droplets (multilocular); more cytoplasmic organelles 3. highly vascularized; synapses with autonomic nervous system; 4. especially prominent in rodents & hibernating animals, and birds; 5. found especially in the neck region in newborn humans 6. provides rapid energy and food for hibernating animals VII. REGENERATION AND REPAIR OF CONNECTIVE TISSUE A. B. C. D. The Fibroblast or fibroblast-like cell (astrocytes of CNS) is the primary cell of repair Macrophages and neutrophils remove old cells and debris by phagocytosis Capillaries invade the tissue, bringing in progenitors of fibroblasts. Fibroblasts replace themselves by division or differentiate from mesenchymal cells in the CT E. Fibroblasts secrete matrix (collagen & ground substance) helping to form Granulation Tissue F. The process can be excessive causing Fibrosis, or an abundance of fibrous tissue, referred to as "Proud flesh" in horses. VIII. Summary Think Connective Tissue Proper Fibroblasts Collagen bundles Type I Blood vessels and nerve Resident cells Fibroblasts Histiocytes Mast cells Reticular cells Transient cells All White blood cells 8