REFERRAL RECOMMENDATIONS : PAEDIATRIC SURGERY
advertisement
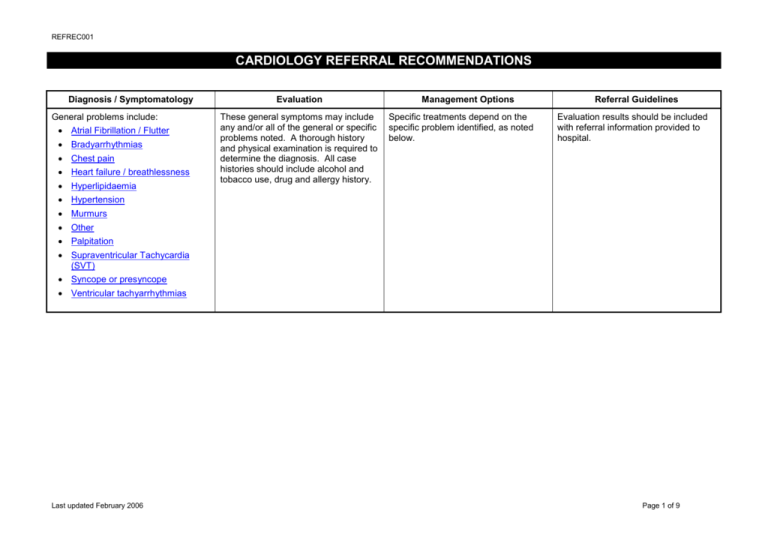
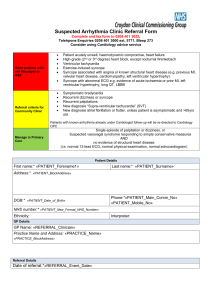
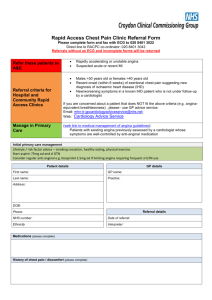
REFREC001 CARDIOLOGY REFERRAL RECOMMENDATIONS Diagnosis / Symptomatology General problems include: Atrial Fibrillation / Flutter Bradyarrhythmias Chest pain Heart failure / breathlessness Hyperlipidaemia Evaluation These general symptoms may include any and/or all of the general or specific problems noted. A thorough history and physical examination is required to determine the diagnosis. All case histories should include alcohol and tobacco use, drug and allergy history. Management Options Specific treatments depend on the specific problem identified, as noted below. Referral Guidelines Evaluation results should be included with referral information provided to hospital. Hypertension Murmurs Other Palpitation Supraventricular Tachycardia (SVT) Syncope or presyncope Ventricular tachyarrhythmias Last updated February 2006 Page 1 of 9 REFREC001 Diagnosis / Symptomatology Atrial Fibrillation/Flutter Evaluation History – duration of symptoms. Evidence of underlying lung disease/HT/cardiac disease/thyroid disease/strokes/TIAs/diabetes. Drug history including alcohol and tobacco. Associated symptoms, eg. angina, dyspnoea, syncope and presyncope. Management Options Chronic or recurrent paroxysmal. Consider anti-arrhythmia and anticoagulation therapy after discussion with specialist, as required. Acute AF/Atrial Flutter. Discuss or refer immediately for management. Referral Guidelines Refer all patients for assessment after discussing options. Acute AF – Category 1 – admission for haemodynamic compromise. Admission may not be required if stable. Chronic AF – Category 3 – routine. ECG. Thyroid Function Tests, UEC. CXR. Echocardiogram Diagnosis / Symptomatology Bradyarrhythmias, eg: – Heart block – Sinus Bradycardia – Sick Sinus syndrome Last updated February 2006 Evaluation History – duration of symptoms. Evidence of underlying cardiac disease. Drug history (including eye drops). Associated symptoms, eg. syncope, SOB, dizziness, palpitations. Consider 24 hour ambulatory ECG recording or event recorder if paroxysmal. ECG. Thyroid function tests. Consider echocardiography. Management Options Asymptomatic: Discuss. Symptomatic: Referral Guidelines Complete heart block and syncope – Category 1. Bradyarrhythmia with dizziness – Category 2. Refer for outpatient assessment. Consider acute assessment if symptoms severe. Page 2 of 9 REFREC001 Diagnosis / Symptomatology Chest pain Evaluation History – duration, precipitants, type, radiation, response to treatment. Evidence of underlying cardiac/ respiratory/gastric disease. Drug history. Associated symptoms, eg. SOB, palpitations, GI symptoms. ECG. Cardiac enzymes if acute. Lipids. FBC. Management Options Referral Guidelines Acute or suspected MI – aspirin and immediate admission. Refer management options which defines referral guidelines. Unstable symptoms or rest pain – refer for immediate admission. Acute MI Probable stable angina, commence aspirin and nitrolingual spray and BBlockers if no contraindication. (Ultimately will require ACE I and statin as well). Risk factor modification. Refer for outpatient opinion. } Category 1. Acute unstable angina } New onset angina } Angina CCS 3-4 } Category 2. Stable angina CCS 1-2 – Category 3. UEC. Glucose. CXR. Exercise stress testing. Possible chronic angina – consider trial of medication (aspirin, beta blockers and nitrates). Consider referral to appropriate service. Risk factor evaluation. Immediate admission – Category 1. Suspected pulmonary embolus/aortic dissection – immediate admission to appropriate specialty. Last updated February 2006 Page 3 of 9 REFREC001 Diagnosis / Symptomatology Heart failure/breathlessness Last updated February 2006 Evaluation Management Options History – duration, PND, orthopnoea, NYHA class. Evidence of underlying cardiac/ respiratory/thyroid disease. Drug history. Associated symptoms, eg. angina, palpitations. ECG. FBC, U&E, blood glucose, lipid profile, TFTs, LFTs. CXR. Echocardiography. Weight. Risk factor evaluation. Alcohol history. If acute heart failure, refer for assessment/admission. Oxygen, nitrate patch and IV Frusemide prior to transfer. Referral Guidelines Acute heart failure – Category 1 All non-acute patients – initial assessment – Category 3. If evaluation suggests heart failure, commence diuretics and other treatment as appropriate. This includes ACE I (if no aortic stenosis), carvedilol, spironolactone, and digoxin with atrial fibrillation. Management of precipitating conditions, eg. obesity, thyroid disease, alcohol consumption and anaemia. Page 4 of 9 REFREC001 Diagnosis / Symptomatology Hyperlipidaemia Last updated February 2006 Evaluation Rick factor evaluation: Family history, particularly age of onset. Smoking. Hypertension. Diabetes. Cardio-vascular disease. Obesity. Age. Fasting lipids (at least two specimens). Blood sugar. Thyroid function / Liver function Management Options Refer to current guidelines – National Heart Foundation, particularly dietary advice. Referral Guidelines Referral letter for consideration of lipid lowering therapy according to NHF guidelines. Management of other risk factors. Page 5 of 9 REFREC001 Diagnosis / Symptomatology Hypertension Evaluation History – duration. Evidence of underlying cardiac/renal/ endocrine disease. Management Options Lifestyle modification. Family history. Antiypertensive treatment should be individualised according to comorbid conditions Associated symptoms, eg. angina, SOB, palpitations, neurological. eg. angina and hypertension (BBlocker). ECG. Diabetes and hypertension – ACE inhibitors. Drug history, including alcohol. FBC, U&E, blood glucose, lipid profile. CXR. Referral Guidelines Refractory hypertension – patients on three or more medications with BP greater than 140/90. Secondary hypertension should be referred to appropriate service, ie. endocrinology, renal or cardiac service. Hypertension in pregnancy should be referred initially to obstetricians. MSU. Malignant hypertension – Category 1. Risk factor evaluation. Consider investigation of secondary causes, eg. co-arctation, phaeochromocytoma, Cushing’s, Conn’s syndrome, renal artery stenosis. Last updated February 2006 Severe hypertension > 200/120 – Category 2. Other hypertension – Category 3. Page 6 of 9 REFREC001 Diagnosis / Symptomatology Murmurs Evaluation Management Options Referral Guidelines Suspected endocarditis – Category 1. History – duration, rheumatic fever. If evaluation suggests innocent (benign flow) murmur – reassure. Associated symptoms, eg. angina. Otherwise, refer. Cardiac enlargement Developmental, gestational history. Family history. } Category 3. Non-innocent murmurs } SOB, palpitations, syncope. Any other stigmata of congenital anomaly? ECG. CXR (if not pregnant). Echocardiography. Diagnosis / Symptomatology Other, eg. Asymptomatic cardiomegaly. Asymptomatic patients with abnormal ECGs. Transfers of patients from other hospitals into local care. Last updated February 2006 Evaluation History – duration: post treatments. Evidence of underlying cardiac disease. Drug and alcohol history. ECG. CXR. Consider echocardiography. Weight. Risk factor evaluation. Management Options Discuss with cardiologists if required. Referral Guidelines Referral if appropriate – Category 3. Page 7 of 9 REFREC001 Diagnosis / Symptomatology Palpitation – including SVT Evaluation History – duration of symptoms (careful description of attack, onset/offset, character of palpitation etc). Evidence of underlying cardiac/thyroid disease/HT. Drug history including caffeine and alcohol. Management Options Referral Guidelines If evaluation negative or suggests only ectopic beats or sinus tachycardia – reassurance. In the presence of underlying cardiac disease, significant symptoms, abnormal ECG, or ongoing palpitations, refer to Cardiologist – Category 3 – routine. Letter of referral for ECG if prolonged or ECG to be sent/faxed from GP practice for opinion. (Category 2 – urgent if syncope present.) Associated symptoms, eg. syncope, presyncope, chest pain and dyspnoea. ECG (during if possible). Thyroid Function Tests, FBC and U&E. Consider 24 hour ambulatory ECG recording and echocardiography. Diagnosis / Symptomatology Supraventricular Tachycardia (SVT) Last updated February 2006 Evaluation History – duration of symptoms. Evidence of underlying cardiac/thyroid disease. Drug history. Consider 24 hour ambulatory ECG recording or event recorder if paroxysmal. ECG. Thyroid function tests. Echocardiography. Management Options If isolated in the absence of syncope/ haemodynamic compromise: Reassure. Consider vagolytic manoeuvres. If recurrent or abnormal ECG – refer. Referral Guidelines In the presence of underlying cardiac disease, significant symptoms, abnormal ECG, or ongoing palpitations, refer to cardiologist. SVT – continuous – Category 1. SVT – other – Category 3. Page 8 of 9 REFREC001 Diagnosis / Symptomatology Syncope or presyncope Evaluation History – duration of symptoms, precipitants (eg. cough, micturition) Evidence of underlying cardiac disease/GI bleeding. Drug history especially diuretics. Associated symptoms, eg angina, SOB, palpitations, neurological signs/ postural hypotension. ECG. Full blood count. Consider 24 hour ambulatory ECG recording or event recorder if paroxysmal. Thyroid function tests. UEC, Mg. Management Options Isolated event and negative findings – reassure. History suggests vaso-vagal event in young and otherwise fit – reassure (vasovagal or neurocardiogenic syncope – recommend hydration, liberal with salt intake and avoid prolonged immobilistation). (refer if recurrent). Referral Guidelines Syncope – Category 1 or 2. Presyncope – Category 3 – routine. If recurrent – refer. Consider echocardiography. Diagnosis / Symptomatology Ventricular Tachyarrhythmias Evaluation History – duration of symptoms Evidence of underlying cardiac disease. Drug history. Associated symptoms, eg angina and syncope, SOB. ECG. Management Options Immediate phone referral for acute admission (via ambulance). Referral Guidelines Admission – Category 1. Draw blood for UEC, Mg, CK. (May be useful if need DCV – send with ambulance). IV cannula. Echocardiogram. Last updated February 2006 Page 9 of 9