Combined_Travel_form_and_info_leaflet
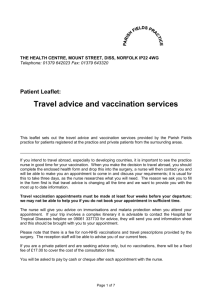
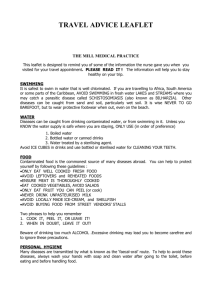
advertisement

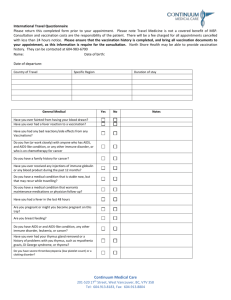
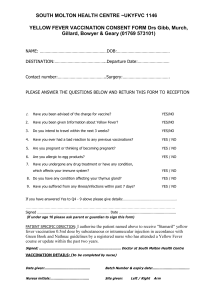
Personal details Name: Date of birth: Male [ ] Female [ ] Easiest contact telephone number: E mail: Dates of trip Date of departure Return date or overall length of trip Itinerary and purpose of visit Country to be visited Length of stay Away from medical help at destination, if so, how remote? 1. 2. Future travel plans Please tick as appropriate below to best describe your trip 1. Type of trip Business Pleasure Other 2. Holiday type Package Self organised Backpacking Camping Cruise ship Trekking 3. Accommodation Hotel Relatives/family home Other 4. Travelling Alone With family/friend In a group 5. Staying in area which is Urban Rural Altitude 6. Planned activities Safari Adventure Other Personal medical history Do you have any recent or past medical history of note? (including diabetes, heart or lung conditions) List any current or repeat medications Do you have any allergies for example to eggs, antibiotics, nuts? Have you ever had a serious reaction to a vaccine given to you before? Does having an injection make you feel faint? Do you or any close family members have epilepsy? Do you have any history or mental illness including depression or anxiety? Have you recently undergone radiotherapy, chemotherapy or steroid treatment? Women only: Are you pregnant or planning pregnancy or breastfeeding? Have you taken out travel insurance and if you have a medical condition, informed the insurance company about this? Please write below any further information which may be relevant © Jane Chiodini Vaccination history Have you ever had any of the following vaccinations / malaria tablets and if so when? Tetanus Polio Diphtheria Typhoid Hepatitis A Hepatitis B Meningitis Yellow Fever Influenza Rabies Jap B Enceph Tick Borne Other Malaria Tablets For discussion when risk assessment is performed within your appointment: I have no reason to think that I might be pregnant. I have received information on the risks and benefits of the vaccines recommended and have had the opportunity to ask questions. I consent to the vaccines being given. Signed: Date: FOR OFFICIAL USE Patient Name: Travel risk assessment performed Yes [ ] No [ ] Travel vaccines recommended for this trip Disease protection Hepatitis A Hepatitis B Typhoid Cholera Tetanus Diphtheria Polio Meningitis ACWY Yellow Fever Rabies Japanese B Encephalitis Other Yes No Further information Travel advice and leaflets given as per travel protocol Food water and personal hygiene advice Insect bite prevention Insurance Websites Travellers’ diarrhoea Hepatitis B and HIV Animal bites Air travel Travel record supplied Other Accidents Sun and heat protection Malaria prevention advice and malaria chemoprophylaxis Chloroquine and proguanil Chloroquine Doxycycline Atovaquone + proguanil (Malarone) Mefloquine Malaria advice leaflet given Further information e.g. weight of child Signed by: Position: VCG/LVP/09/28670/2 21001709 Date of preparation: February 2009 Date: Travel and Health What you need to know before you go This pack is a guide only. Advice will vary depending upon your destination, duration of travel, types of accommodation and what activities you take part in. You should discuss your requirements with the nurse at the travel clinic. If possible, please make your first appointment up to eight weeks prior to departure. Vaccinations for Typhoid, Hepatitis A, Meningitis C, Tetanus, Diphtheria and Polio are provided by the NHS. Other vaccines including Yellow Fever, Hepatitis B, Rabies, Meningitis and Malaria will attract a fee. Please see the website for current prices. For further advice please see the following websites: www.nhs.uk (this also contains a number of useful videos). www.nathnac.org www.fitfortravel.nhs.uk www.malariahotspots.co.uk Diseases Preventable by Vaccination Yellow Fever This disease is spread by infected mosquitoes normally from sunrise to sunset and is endemic in parts of Sub-Saharan Africa and South America. During outbreaks it has up to a 60% mortality rate and therefore the World Health Organisation (WHO) recommends vaccination against Yellow Fever if travelling to affected regions. In addition, some countries require a certificate proving vaccination before allowing entry. A single vaccine lasts for ten years and is available only at Registered Yellow Fever Centres. Insect bite avoidance using repellents, mosquito nets and covering up in clothing treated with Bug proof Clothing Treatment is essential. For advice re Yellow Fever areas contact www.nathnac.org Tetanus The bacteria that causes tetanus is present in soil worldwide and disease occurs when the bacteria gets into a wound or even small cuts. The disease leads to uncontrollable muscle spasms and possibly death. Travellers should ensure they have had a tetanus vaccine within the last ten years before they travel. Polio Polio is a disease of the central nervous system usually spreads through contaminated food and water. Many countries have eradicated polio through vaccination although it still exists in some African and Asian countries and cases continue to occur worldwide. Boosters are recommended at ten yearly intervals if travelling to an endemic country. Diphtheria Diptheria is a bacterial disease spread mainly by exhaled water droplets and occasionally through infected skin lesions. It can be fatal if left untreated. Travellers are at risk when mixing closely with the local population in most developing countries. Travellers should ensure they have had a diphtheria vaccine within the last ten years if they are likely to be at risk. Typhoid Typhoid is spread through faecally contaminated food and water. The disease is common in areas with poor standards in food hygiene and preparation and where suitable treatment of sewage is lacking. It is possible to contract typhoid from shellfish, raw fruit or vegetables fertilised by ‘night soil’ (human waste). A feverish illness will develop 1-3 weeks after infection and, without correct diagnosis and treatment, the disease can spread through the gut wall and cause a serious infection throughout the body. It is also possible to become a carrier of this disease when bacteria remain in the gut after symptoms have resolved but you continue to be able to infect others. This disease can be prevented by healthy eating and drinking and pre-travel vaccination. A single vaccine is valid for 3 years. Cholera Cholera epidemics typically happen in areas where there are lots of people with very poor hygiene facilities (particularly slums and refugee camps) and areas affected by floods and rainy seasons. Most travellers should experience minimal risk of exposure to cholera but the risk is far greater for emergency relief and health workers in refugee camps. There is an effective vaccine available for cholera administered orally in two doses one to six weeks apart. Tuberculosis TB is mainly spread through infected respiratory droplets but also through unpasteurised milk. The BCG vaccine provides limited protection and is advised for healthcare workers and those under age 16 years travelling for more than 3 months to high risk countries. Vaccination is provided either at the BRI Travel Clinic or Normad Travel Hepatitis A This disease affects the liver and is usually spread through contaminated food and water or close physical contact with an infected person. It is common in developing countries where sanitary conditions are poor and the safety of drinking water is not adequately controlled. The disease can incubate for 3-5 weeks before illness develops. Adults can take many months to fully recover from infection whereas children often have very mild illness but can easily pass it to others. Hepatitis A is prevented by eating ‘safe food’, drinking ‘safe water’ and pre-travel vaccination. Single vaccine valid for minimum of 1 year with one booster vaccine providing cover for 20 years+. Hepatitis B Hepatitis B is another disease which affects the liver. It is associated with chronic liver problems leading to increased risk of liver cancer or cirrhosis. It is found worldwide, although the general infection rate if far higher in Africa than elsewhere. Many Hepatitis B infections cause mild symptoms and may not be recognised; however infected individuals may develop into being lifelong carriers. Hepatitis B is generally spread through unprotected sex and blood (via blood transfusions, dirty needles, piercing and tattoos etc); however it may also be transmitted though body fluids. It is 100 times more infective than HIV. All travellers should consider a course of Hepatitis B vaccines, especially if travelling long term or those working with children and humanitarian aid workers. It is a 3 dose course, given over a 3 week to 6 month period. Rabies Rabies is endemic throughout most of the world and causes approximately 60,000 human deaths per year. The virus is carried in the saliva of infected mammals (which may appear normal) and is usually spread by a bite but licks on open wounds and scratches have been enough to transmit the virus to humans. In the event of a possible exposure the area should be washed thoroughly with soap and water, irrigated with iodine based antiseptic and medical attention sought as soon as possible, ideally within 24 hours. The virus affected the nervous system and once symptoms develop death is inevitable even with good medical care. A pre-exposure course of 3 vaccines is available and should be administered over a 3 weeks period. Meningitis Sub-Saharan Africa has frequent epidemics of meningitis, particularly in the zone stretching from Senegal to Ethiopia during the dry season. Outbreaks have also been known in India and Nepal and during religious pilgrimages to Saudi Arabia. Meningitis is an inflammation of the surface of the brain. Transmission occurs from direct person to person contact and through inhaling infected droplets. Vaccines for strains A, C, W135 and Y are available and should be considered, especially for extended trips or if mixing very closely with the local population during risk season. A certificate of vaccination may be required if visiting Saudi Arabia. (Please note only Meningitis C is given in schools). Single vaccines last 3-5 years; this is dependent on visa requirements. Japanese Encephalitis This disease is spread through the bite of an infected mosquito normally between sunset and sunrise. It is most common in rural farming areas of Asia. Most infections have few symptoms and may not be recognised but severe cases can lead to inflammation of the brain and other symptoms which can be fatal. Risks to travellers are generally very low but vaccination should be considered by people intending to spend a significant length of time in rural areas, particularly during the transmission season (monsoon). The vaccine is a course of 2 injections given 28 days apart. Vaccination is available at the BRI Travel Clinic or Nomad Travel. Tick Bourne Encephalitis Spread by the bite of an infected tick and, rarely, via unpasteurised milk from infected cows, sheep and goats. Travellers at risk include those planning to walk, camp or work in long grassy or wooded areas for long periods, especially during spring, summer and autumn months, as this is when the ticks are more active. If caught, symptoms include flu like illness sometimes followed by neurological complications. If at risk, travellers should consider vaccination which involves 2 initial injections and a booster for extended coverage. They should also avoid tick bits by covering up and treating clothing with Permethrin (|Bugproof Clothing Treatment) which is a tick killer. Always remove any ticks promptly. Vaccination is available at the BRI Travel Clinic or Nomad Travel Chikungunya Currently widespread and similar to Dengue Fever, Chikungunya is spread by the bites of infected mosquitoes that normally bite between sunrise and sunset. Bite avoidance is essential as vaccination is not available. Symptoms include fever, bone pain and rash – all similar to Dengue. Treatment is not available but symptoms will resolve themselves in time. Schistosomiasis (Bilharzia) Bilharzia is a parasitic infection caused by flukes that use freshwater snails as hosts. It is caught through swimming, wading or bathing in contaminated fresh water. It is particularly high risk in Africa in areas such as Lake Malawi but also in parts of Asia and north eastern South America. The flukes can burrow into unbroken skin causing no initial symptoms but if left untreated can lead to long term problems such as liver, bladder and kidney disease. There is no vaccine available so all travellers are advised to avoid swimming, bathing or wading in possibly contaminated water. If unavoidable, then it is possible to get tested at least 12 weeks following possible exposure and then treatment given if required. Leishmaniasis Leishmaniasis if contracted through the bites of infected sandflies (phlebotomus), which bite normally at night. The disease affects the skin causing lesions close to the bite slowly growing larger 4-6 weeks after the initial bite. Other symptoms can include fever, sweating, lymph node disturbance and inflammation of the spleen. There is no vaccine available so all travellers are advised to carry out strict bite avoidance using Permetherin impregnated mosquito nets (sandflies fly low to the ground so high hammocks and beds will give some protection) and 50% DEET frequently on the skin (hourly in humid environments). Dengue Fever Denque Fever is spread by daytime biting mosquitoes normally from sunrise to sunset and is more common in urban areas. As there is no vaccine available to provide protection against this disease, insect bite avoidance is essential. It is currently widespread in many countries and it is often known locally as Break Bone Fever since it causes a feverish illness with associated bone pain. Its severest form is more common in children and people experiencing repeat infection. Insect bite avoidance using repellents, mosquito nets and covering up in clothing treated with Bugproof Clothing Treatment is essential. Malaria Malaria is a common and life threatening disease in the tropics and affects many international travellers each year. It is caused by a parasite introduced by the bite of an infected mosquito that feeds normally from sunset to sunrise. Symptoms will develop 8 days or more after the infected bite. Severe illness or death can occur within a few hours of the first symptom. Early symptoms include high temperature with shivering, headache, muscle ache and weakness, vomiting and diarrhoea. Malaria is a far more serious disease for young children and pregnant women. Prompt medical treatment can be life saving. Antimalarial tablets are recommended for risk areas and the choice of drug will depend on your destination, medical history and budget. Avoiding insect bites using repellents, covering up with treated clothes and sleeping under a mosquito net are also essential to protect against malaria and several other common tropical diseases spread by insect bites. To determine if you are going to a malaria area please visit www.fitfortravel.nhs.uk or www.malariahotspots.co.uk Malaria Prophylaxis Possible side effects: Not suitable if you have: Nausea/vomiting Diarrhoea Skin rashes/visual disturbance/headache Convulsions Hair thinning Epilepsy Psoriasis Severe renal impairment Mild gastric intolerance Diarrhoea Occasional mouth ulcers Skin rash/hair thinning Known to increase effects of Warfarin Renal impairment Chloroquine Two tablets to be taken together once a week on the same day each week wth food. Start one week before entering the malarial region, continue whilst at risk and for 4 weeks after last possible malarial contact. Proquanil (Paludrine) Two tablets to be taken together each day with food. Usually taken in combination with chloroquine. Commence course one week prior to entering the malarial region, continue whilst at risk and for 4 weeks following last possible malarial contact. In pregnancy, high dose folic acid supplements are needed. Doxycycline One capsule to be taken daily at the same time each day with food and a large glass of water. Start 1-2 days before entering the malarial region, continue whilst at risk and for 4 weeks after last possible malarial contact. Heartburn/nausea Pregnant/breast feeding Increased sensitivity to the Children under 12 years sun Allergy to Tetracycline Photosensitive rash (1-3% antibiotics of users) Diarrhoea/headache/visual disturbance Vaginal thrush May affect absorption of the pill (Alternative contraceptive precautions should be used for the first 3weeks, after which time gut flora will have adapted and full contraceptive cover resumed.) Malarone & Malarone Paediatric One tablet to be taken every day, starting 1-2 days before entering the malarial region, continue whilst at risk and for 7 days after last possible malarial contact. Ideal for short visits. Licensed for 28 days in malarial regions but can be used for up to 1 year. (Children’s dosing may vary.) Mefloquine (Lariam) One tablet weekly on the same day each week. Try 3 tablets prior to travel (start 2½ weeks before departure), continue whilst in malarial region and for four weeks after last possible malarial contact. Nausea/vomiting Diarrhoea Abdominal pain/loss of appetite Cough Pregnant Renal failure Sleep disturbances Nausea/vomiting Diarrhoea Dizziness Rashes/abdominal pain Anxiety/panic attacks Depression Psychotic reactions/convulsions Rarely: hallucinations Pregnant/breast feeding History of seizures/epilepsy History of depression Psychiatric disorders Cardiac conduction defects Calcium channel blockers Beta blockers Severe renal or hepatic failure Insect Bite Avoidance There are many tropical diseases spread through insect bites. There are vaccines and medicines available to help protect against some, others are prevented only by avoiding insect bites. Spray insect repellents containing up to 50% DEET on skin, cover up using clothing preferably treated with bug proof clothing treatment (Permethrin) and sleep under mosquito nets treated with a similar product. If you are staying in an air conditioned room with a guarantee electrical supply you could use a “plug in” unit which will give off an odourless vapour throughout the evening to kill insects in your room or use a standard knockdown room spray. Mosquitoes can bite through tight clothing, so wear loose-fitting long trousers and long sleeves in the evening in malaria hot spots. Water and Food Safety Many infectious diseases are transmitted through contaminated food and water. You can reduce your risk of these diseases by following some basic guidelines: Don’t drink tap water or use it to brush your teeth in countries with poor sanitation. Use filtered or bottled water instead. When drinking bottled water always check that the seal is on securely and if in doubt then carbonated water will be safe. Don’t put ice in drinks. Boiled water or drinks made with boiled water should be safe. Don’t eat salads, uncooked fruit and vegetables unless you’ve washed and peeled them yourself. Don’t eat food that has been kept at room temperature in warm environments, or that has been exposed to flies. Don’t consume unpasteurised milk, cheese, ice cream or other dairy products. Avoid raw or undercooked seafood. Alcohol hand sanitizers should be used prior to eating Travellers’ Diarrhoea Travellers’ Diarrhoea is a very common illness caused by contaminated food and water or by poor hygiene. Ensure you wash your hands every time before you eat. If clean water is not available use an alcohol hand wash. If you do get travellers’ diarrhoea it generally only lasts a few days. General advice is as follows: I Drink plenty of fluids to avoid dehydration. Slightly increase the level of salt and sugar intake with meals. Alternatively use a ready prepared rehydration treatment solution. Anti-diarrhoea agents such as loperamide (Imodium®) or diphenoxylate plus atropine (Lomotil®) should be used sparingly - they can help particularly with associated colicky pains and may be considered for those in whom frequent diarrhoea is inconvenient eg those travelling on long bus/train/plane journeys or for business meetings. However it should not be used if the traveller has active inflammatory bowel disease (eg Ulcerative Colitis) a fever or bloody diarrhoea. Overuse can cause 'rebound' constipation and occasionally encourage other complications such as septicaemia. If your diarrhoea is severe (more than six episodes per day), lasts for several days and you have a high temperature or are passing blood or mucus in your stools, it is best to consult a doctor as soon as possible. Accidents More holiday makers and travellers die from accidents abroad than from any other cause. Don’t hire mopeds if you haven’t ridden before- the roads may be in a poor state and road safety may be poor. Always wear seat belts and avoid poorly lit roads at night. Always ensure that you have sufficient travel insurance to cover any visits to a doctor or hospital. Always travel with a good medical kit including a sterile needle. Travel packs can be purchased at the surgery – please ask the nurse for details. Animal Bites Rabies is present in most countries worldwide. It is responsible for approximately 60,000 human deaths a year, particularly in India. It is also prevalent in South America, Asia and Africa. Rabies is a virus transmitted through the saliva of a bite, lick or scratch from an infected animal that may not show any signs of infection. Should a bite occur, you should wash the wound thoroughly, apply a good antiseptic and get medical help as soon as possible. Sexual Health A sexually transmitted infection (STI) or unintended pregnancy can be the worst kind of souvenir to bring home, so don’t get carried away and end up having unprotected holiday sex. Please follow these simple guidelines: Buy condoms before you go on holiday. Check that these have the CE mark on them to show that they have been manufactured to the standards required in Europe. Remember that condoms can be damaged by oil-based products such as moisturiser, sun screen products, baby oil and lipstick. Heat can affect condoms so store them in a cool place. Diarrhoea, vomiting, some antibiotics and anti-malaria tablets can make the contraceptive pill or implant less effective. Use a condom to help protect against an unwanted pregnancy or STI. If you are worried about an STI or unwanted pregnancy please contact the surgery or Sexual Health Clinic as soon as you return home. If you are still abroad, check your travel insurance cover. Private doctors can be expensive and there is no guarantee of standard care. Where possible try to avoid antibiotic injections. Most antibiotics can be taken orally. Please refer to drug information sheets for details. Personal Hygiene Keep your nails short – trapped dirt can easily make its way into your mouth. Avoid biting your nails and putting objects into your mouth (sunglasses, pens etc). Use plenty of soap. Water alone will not kill bacteria. Use wet wipes or a no water hand gel when it is difficult to wash. Avoid sharing clothing and equipment. Keep your clothes clean. Frequently wash sweaty parts of your body to avoid fungal infections. Pay close attention to dental care. Sun Most holiday destinations are usually a lot sunnier than we are used to. Sunburn, heat exhaustion and sunstroke are unpleasant and can be dangerous. Protect yourself with high factor sunscreen. Cover up with shirts and hats especially during the midday sun (12.00 – 15.00) In higher altitudes there is less atmosphere to filter out the sun’s harmful rays so be particularly careful. In hotter climates you will sweat more so drink more non-alcoholic drinks to prevent dehydration. Re-apply sunscreen or insect repellents which may have sweated off. Personal Safety Try to keep expensive camera and other equipment hidden where possible. Take copies of important documents such as passports, tickets and insurance details and keep these in a separate place from the originals. Just before you leave send yourself an e-mail with important telephone numbers, passport number and flight details. Always try to carry cash in several places – some in a hidden money belt and a small amount in your pocket for easy access. Never leave valuables in a hotel room unless you can be sure of its safety. Ask to use the hotel safe. Air Travel and DVTs A growing concern for travellers is deep vein thrombosis (DVT). For the majority of healthy travellers the risk is small although this does increase with flight duration. By drinking plenty of non-alcoholic and caffeine free fluids during the flight and mobilising your legs as often as possible you will greatly reduce the risks. Compression stockings may be beneficial but seek advice from your GP or nurse. These are recommended for patients over the age of 40 and on a flight longer than 4 hours. They can be purchased from major chemists. If you have any medical conditions (heart problems or previous DVTs) please consult with your GP or nurse for specialist advice. We hope that you enjoy your holiday. Please use the sheet below to record any major queries you may have for the nurse at your travel appointment. Personal Travel Checklist Queries from reading the Travel Advice 1.0 2.0 3.0 4.0 5.0 6.0 List of items to buy before holiday Vaccination Appointment Schedule Date 1st Visit 2nd Visit 3rd Visit Time