Knowsley - service specification revised
advertisement
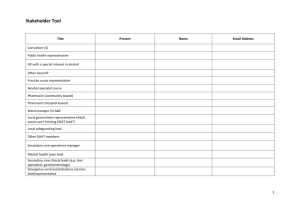
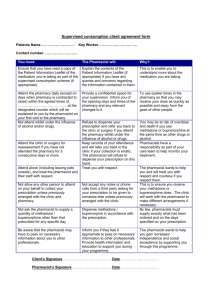
SERVICE SPECIFICATION FOR PROVISION OF ANTICOAGULANT MONITORING SERVICE BY PHARMACIST PRACTITIONERS IN A PRIMARY CARE CLINIC AT THE KIRKBY HEALTH SUITE AIMS OF SERVICE Pharmacist Practitioners to provide optimal therapeutic control for patients prescribed oral anticoagulants whilst minimising the risks associated with such therapy. Overall responsibility for the organisation, supervision and adherence to quality assurance and quality control standards within the primary care clinic, will be held by the Primary Care Pharmacist with responsibility for the Anticoagulant Service. 1. 2. SPECIFIC OBJECTIVES 1.1 To maintain anticoagulation within a prescribed range by dose adjustment, anticipating changes and frequency of review. 1.2 To monitor therapy with reference to appointments and length of treatment. 1.3 To educate and inform patients. 1.4 To maintain documentation. 1.5 To perform quality control testing and routine maintenance of anticoagulant monitoring equipment. CLINIC ORGANISATION 2.1 Referral of Patients to Primary Care Anticoagulant Clinic Patients will be referred to the Primary Care Anticoagulant Clinic by: - Their General Practitioner after being stabilised by the University Hospital Aintree NHS Trust Anticoagulant Service. - Transferred directly to the Primary Care Anticoagulant Clinic by University Hospital Aintree NHS Trust. - Referrals from other Trusts will be accepted at the discretion of the Anticoagulant Services Manager. - Direct Referrals will not be accepted for housebound patients. When patients are referred or transferred to the Clinic, relevant documentation in the form of anticoagulant clinic records will be completed. These records should contain the original prescription for therapy, which will include indication for therapy, prescribed International Normalised Ratio (INR) range, duration of treatment, drug history and concomitant disease history, and any previous anticoagulant therapy records. Where INR range is not specified, the pharmacist practitioner will apply an INR range according to British Haematological Guidelines and bring this to the attention of the Anticoagulant Services Manager. 2.2 Clinics 2.2.1 Patients will be seen by appointment in the designated room at the Kirkby Health Suite by a pharmacist practitioner who has undergone appropriate training. 2.2.2 The anticoagulant dose will be adjusted by the pharmacist practitioner with reference to the patient's INR and any other changes that may be identified during the appointment. 2.2.3 Under normal circumstances patients will be reviewed for INR measurement and dosage adjustment, if necessary, at least every 12 weeks. 2.2.4 Adequate information will be provided to ensure General Practitioners are kept informed of the progress of their patient. 2.2.5 Reception staff at the Kirkby Health Suite will document the date and time of the next appointment in both the patient's record card and the Health Suite anticoagulant appointments file. 2.2.6 If a patient fails to attend a clinic, the attached DNA policy will be applied (appendix 1). A new appointment should be scheduled within 2 weeks either by telephone or use of a standard letter to the patient. 2.2.7 For regular non-attenders, the Anticoagulant Services Manager will inform the GP in writing, and a decision made as to future management of these patients. 2.3 Domiciliary Visits 2.3.1 Patients may be referred for domiciliary visits if they are existing patients of the Kirkby Anticoagulant Service and due to unforeseen circumstances can no longer attend the clinic. 2.3.2 The Home Visiting Policy (Appendix 4) will be adhered to at all times. 2.3.3 Patients will be seen in their home by a pharmacist practitioner or technician who has undergone appropriate training. The anticoagulant dose will be adjusted by the pharmacist practitioner. If the technician has visited the patient they will contact the pharmacist over the telephone in order for the pharmacist to dose the patient. The patient will be dosed with reference to the patient's INR and any other changes that may be identified during the appointment. 2.3.4 Under normal circumstances patients will be reviewed for INR measurement and dosage adjustment, if necessary, at least every 12 weeks. 2.3.5 Adequate information will be provided to ensure General Practitioners are kept informed of the progress of their patient. 2.3.6 The technician will document the date and time of the next appointment in both the patient's record card and in the domiciliary appointments file. 2.3.7 If a patient is not at home, the attached DNA policy will be applied (appendix 1). A new appointment should be scheduled within 2 weeks either by telephone or use of a standard letter to the patient. 2.4 Referring Patients for Medical Advice 2.4.1 Occasionally patients may seek medical advice from the pharmacist practitioner. In these circumstances patients will be advised to consult their General Practitioner. 2.3.2 Patients presenting with the following medical complications of their anticoagulant treatment will be referred immediately to the local hospital A & E department. If necessary further advice will be sought from Dr Ade, Consultant Haematologist, Aintree Hospitals (NHS) Trust, or the patient’s GP. INR greater than 8.0 and / or they have signs or symptoms of bleeding or signs or symptoms of thromboembolic episodes or if thought to be at high risk of bleeding or thromboembolism. If INR > 8.0 and there is absence of both bleeding and risk factors for thromboembolism, any decision not to refer a patient to an A&E Department can only be taken with the agreement of the patient’s GP. 2.5 Confidentiality 2.5.1 In the course of your employment you may come across confidential information regarding patients, staff or the business dealings of Knowsley PCT. Unauthorised disclosure of such information will be considered gross misconduct and will lead to disciplinary action being taken against you. 2.5.2 Immediately upon termination of your employment you must return to us all documents, forms, papers or other records relating to your employment (including copies). 2.5.3 After termination of your employment a breach of confidentiality by you may render you liable for legal action. This does not affect your statutory rights under the Public Interest Disclosure Act 1998. 2.6 Fraud and Probity 2.6.1 The trust is committed to the elimination of fraud, to the vigorous investigation of any such cases and where fraud or a criminal act is proven to ensure that wrong doers are appropriately dealt with. The trust will take appropriate steps to recover any assets lost as a result of fraud. 2.6.2 Employees found in breach of the Trust Fraud and Probity Policy and procedures will be considered to have committed an act of gross misconduct and will, therefore, be subject to disciplinary action. 2.7 Health and safety 2.7.1 Anticoagulant practitioners are required to follow all applicable rules an procedures relating to Health and Safety at Work and take reasonable precautions to avoid accidents. 2.8 Documentation 2.8.1 Strict confidentiality will be maintained. The file will be kept in a lockable filing cabinet in the designated room for anticoagulant monitoring at the Kirkby Health Suite. The room will be accessible only to keyholders. Suitable arrangements will exist for access in the interests of patient safety. 2.8.2 A patient record will be maintained for each patient. This record will be updated at each clinic visit and will contain: a) The original referral form. b) The INR result at each visit. c) The dose of anticoagulant. d) The number of weeks to next appointment e) Relevant notes of each visit. f) Correspondence concerning the individual patient. g) List of current medication h) Any near miss forms 2.8.3 The patient-held anticoagulant treatment card must be updated at each visit. If this is not available, a temporary record booklet must be completed and given to the patients. 2.8.4 The pharmacist practitioner should record the number of attenders, non-attenders and home visits in the designated file and record for each clinic session the number of patients within, above and below specific ranges, the average number of weeks since the last appointment and the results of quality control tests. See Appendix 2. 2.8.5 All files will be kept for 10 years after a patient leaves the care of the anticoagulant service. 2.5 End of Treatment 2.5.1 Two weeks before the end of a specified period of treatment the pharmacist practitioner in consultation with the Anticoagulant Services Manager will notify the GP, detailing a summary of recent clinic appointments. Following a case review by the GP, anticoagulant therapy will either be extended or stopped. The Anticoagulant Services Manager will forward a summary copy of the INR results and dosage of warfarin to the GP for inclusion in patient records. 3. TRAINING 3.1 Before working in an unsupervised capacity the pharmacist practitioner must demonstrate that she/he is suitably qualified and experienced to comply with the specification and must have completed an approved course for pharmacist practitioners undertaking anticoagulant monitoring in primary care and the Knowsley PCT Anticoagulant Pharmacy Competencies. The competencies include key competencies which are to be demonstrated to the satisfaction of the Anticoagulant Services Manager are as follows: Operation of analyser Quality control proceedures Determination of quality control results Obtaining of adequate blood sample Determination of INR results Compliance with an established clinical management protocol for action on INR results Understanding of range of problems likely to be encountered in interpreting INR results. Making dosage adjustments Recognition of instances where it is necessary to seek further advice The giving of information and advice to patients 4. 3.2 As part of their training, pharmacist practitioners and student pharmacist practitioners may work in the service under the direct supervision of a qualified Anticoagulant Pharmacist. 3.3 Pharmacist practitioners will be required to demonstrate good practice through audit and participation in peer review which will be the overall responsibility of the Anticoagulant Services Manager. Pharmacist practitioners will also be required to demonstrate a commitment to continuing education organised through their professional body or other approved method. 3.4 Pharmacist practitioners will undertake fire safety and evacuation procedures on an annual basis and will receive training in cardiopulmonary resuscitation. QUALITY 4.1 General Standard The pharmacist practitioner will exercise professional skill and care in providing the anticoagulant monitoring service. 4.2 Service Quality The pharmacist practitioner must provide the services in a manner which assures safety, confidentiality, comfort, courtesy, dignity and privacy to the patient and shows responsiveness to patients’ needs. 4.3 Non-Discrimination The pharmacist practitioner must not discriminate in his/her provision of services on the basis of race, gender, religion, or disability. 4.4 Statutes The pharmacist practitioner must comply with all applicable statutes, regulations, EC directives and guidelines of the Department of Health and NHS Executive. 4.5 Complaints All complaints will be brought to the attention of the Anticoagulant Services Manager in the first instance. Unresolved complaints will be submitted by the Anticoagulant Services Manager to the Complaints Manager at Knowsley Primary Care Trust, who will investigate the complaint. A record of the number of complaints dealt with locally will be collated by the Anticoagulant Services Manager and submitted to the Complaints Manager. 4.6 Risk Management Records of near miss incidents should be brought to the attention of the Anticoagulant Services Manager within 1 working day and recorded in the notes and on the database. The incident report should be forwarded to the Primary Care Trusts nominated officer within 5 working days. 4.7 Quality Assurance and Control System The pharmacist practitioner will comply with the quality assurance and control system established by the Anticoagulant Services Manager and described in Appendix 3. 4.8 Health & Safety Pharmacist practitioners should be fully immunised against Hepatitis B. 4.9 Clearances All practitioners must consent to and undergo a CRB check and medical. References must also be provided on request. 5. INSURANCE AND INDEMNITY 5.1 Indemnities The pharmacist practitioner must indemnify and keep indemnified Knowsley Primary Care Trust against all costs, claims, damages, liabilities or losses which the Trust may suffer arising out of or in connection with the provision of the said anticoagulant monitoring services. 5.2 Insurance The pharmacist practitioner must warrant Knowsley Primary Care Trust that there is in force professional indemnity insurance covering his/her liabilities in respect of any negligent act or omission in connection with the provision of the said anticoagulant monitoring services under this contract with a limit of indemnity of not less than £500,000. The pharmacist practitioner must maintain such insurance throughout the period of this contract and will provide evidence of such insurance and the payment of all premiums if requested so to do by Knowsley Primary Care Trust. 6. ACCOUNTABILITY 6.1 Practitioners are responsible and accountable for their own actions (including advice and amending dosages) in the anticoagulation management of patients attending clinics. 7. DISCIPLINE AND GRIEVANCE PROCEDURES 7.1 8. A copy of Knowsley PCT’s Discipline and Grievance procedures are available from the HR department. TERMINATION 8.1 The Trust will be entitled to terminate this Agreement forthwith in the event that the pharmacist practitioner commits a serious irremediable breach of his/her obligations hereunder. Under statutory notice requirements: 1 month – 2 years service - 1 weeks notice 2 years – 12 years service - 1 weeks notice for each complete year More than 12 years service - 12 weeks notice 8.2 Without prejudice to paragraph 6.1 in the event that the pharmacist practitioner commits any breach of this Agreement, the Trust will be entitled to serve a notice specifying such breach and requiring it to be remedied forthwith. Should the said notice not be complied with the Trust will be entitled to treat the said breach as a serious and irremediable one for the purposes of paragraph 6.1 hereof. 8.3 If a pharmacist practitioner wishes to terminate the Agreement then they must notify the service manager in writing and serve a notice period of a minimum period of two months. 8.4 If the service manager wishes to terminate the Agreement for any other reason other than stated above they will notify the practitioner in writing providing a notice period of a minimum of two months. This employment is exempt form the provision of the Rehabilitation of Offenders Act 1974. You are therefore not entitled to withhold information requested by us about any previous conviction you may have, even if under the circumstances they would have been regarded as 'spent' under the Act Concealment of such information may result in your dismissal You are also required to tell us of any convictions or offences with which you are charged whilst you are providing a service for us. Both parties agree to the aforementioned terms and conditions of this contract. Amendments and variations of the contract may occur from time to time and any such changes will be notified in writing. Signed ……………………….. Dated Chief Executive Knowsley PCT Signed ………………………. Dated Pharmacist Practitioner APPENDIX 3 ANTICOAGULANT MONITORING SERVICE IN PRIMARY CARE CLINIC QUALITY ASSURANCE AND CONTROL SYSTEM Quality must be assured across all aspects of the service, including clinical supervision, INR testing, dosage advice, record keeping, patient held records and quality control records and testing, information giving and education. The pharmacist practitioner must complete all documentation required and record any action taken which is outside the service protocol. The Anticoagulant Services Manager will be responsible for the monitoring of: Quality Assurance of stored reagents Equipment calibration and maintenance Analytical quality control Compliance with clinical management protocols Maintenance of staff competencies The Anticoagulant Services Manager will: Be responsible for the selection, installation, maintenance and planned replacement of each analyser. Ensure that the calibration and maintenance of each analyser is in accordance with the manufacturer's recommendations. A logbook will document standard operating procedures, faults, repairs and a maintenance schedule. Document the batch numbers and shelf life of reagents used. Ensure that the analytical process is subject to both internal and external quality control in accordance with national guidelines. Analysers will be registered by the Anticoagulant Services Manager with the National Quality External Assurance Scheme or through an accredited laboratory which may provide additional external quality control exercises. There will be a written procedure for assuring a back up service in the event of analyser failure or quality control results falling outside predefined limits. The Anticoagulant Services Manager will ensure the following are evaluated through internal and external audit on a regular basis: clinical outcomes patient waiting times validity of clinical management protocol frequency of patient reviews acceptability of service for patients quality of INR control Appendix 1 POLICY ON FOLLOW-UP OF PATIENTS WHO DNA The aim of this policy is to ensure: Patients who DNA are followed-up appropriately There is prioritisation of appointments which should ensure minimum of additional pressure on clinic appointments The possibility of deceased patients and those in hospital receiving letters is decreased Action required upon a FIRST DNA At the end of each clinic, - FOR EACH PATIENT who did not attend: 1. Reception should inform the pharmacist undertaking the clinic of any patients who have failed to attend. Where a patient has failed to attend twice (i.e. in last few weeks) this should be specifically brought to the attention of the pharmacist. 2. The pharmacist undertaking the clinic should inspect the record for each patient who has not attended. 3. The pharmacist is responsible for informing reception on when the patient should receive their next appointment – usually this will need to be either inside a week, a week, or the first available appointment the week after 4. Reception staff are responsible for issuing the ‘standard’ anticoagulant clinic DNA letter. Additional Action required upon a SECOND DNA Before the end of each clinic, - FOR EACH PATIENT who has DNA twice or more as seen on the appointment sheet (No. of DNAs) The clinic pharmacist should inform SARAH as the services manager who will be responsible for further action. Sarah will then inform reception of the outcome within 48 hours. ACTION REQUIRED FOR PATIENTS WHO REGULARLY MISS THEIR APPOINTMENTS i.e. very irregular attendance without good reason Reception staff should notify SARAH of the details of any such patients. Sarah will take responsibility for discussing this with patient’s GP.