corticosteroids pose an increased risk for serious infection
advertisement
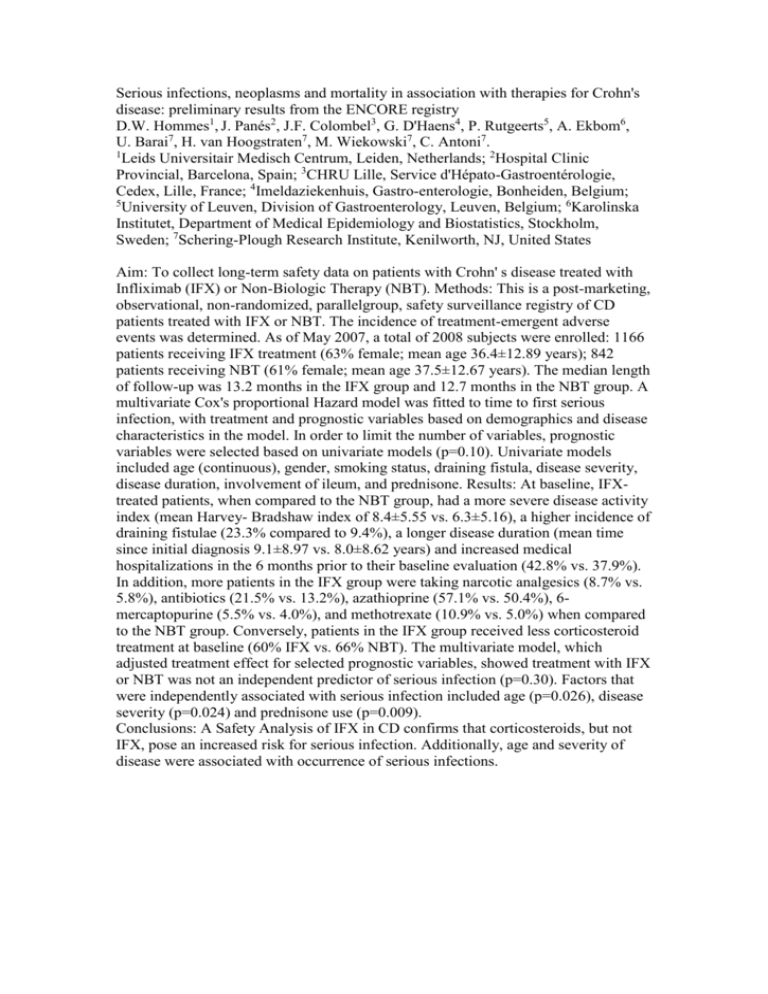
Serious infections, neoplasms and mortality in association with therapies for Crohn's disease: preliminary results from the ENCORE registry D.W. Hommes1, J. Panés2, J.F. Colombel3, G. D'Haens4, P. Rutgeerts5, A. Ekbom6, U. Barai7, H. van Hoogstraten7, M. Wiekowski7, C. Antoni7. 1 Leids Universitair Medisch Centrum, Leiden, Netherlands; 2Hospital Clinic Provincial, Barcelona, Spain; 3CHRU Lille, Service d'Hépato-Gastroentérologie, Cedex, Lille, France; 4Imeldaziekenhuis, Gastro-enterologie, Bonheiden, Belgium; 5 University of Leuven, Division of Gastroenterology, Leuven, Belgium; 6Karolinska Institutet, Department of Medical Epidemiology and Biostatistics, Stockholm, Sweden; 7Schering-Plough Research Institute, Kenilworth, NJ, United States Aim: To collect long-term safety data on patients with Crohn' s disease treated with Infliximab (IFX) or Non-Biologic Therapy (NBT). Methods: This is a post-marketing, observational, non-randomized, parallelgroup, safety surveillance registry of CD patients treated with IFX or NBT. The incidence of treatment-emergent adverse events was determined. As of May 2007, a total of 2008 subjects were enrolled: 1166 patients receiving IFX treatment (63% female; mean age 36.4±12.89 years); 842 patients receiving NBT (61% female; mean age 37.5±12.67 years). The median length of follow-up was 13.2 months in the IFX group and 12.7 months in the NBT group. A multivariate Cox's proportional Hazard model was fitted to time to first serious infection, with treatment and prognostic variables based on demographics and disease characteristics in the model. In order to limit the number of variables, prognostic variables were selected based on univariate models (p=0.10). Univariate models included age (continuous), gender, smoking status, draining fistula, disease severity, disease duration, involvement of ileum, and prednisone. Results: At baseline, IFXtreated patients, when compared to the NBT group, had a more severe disease activity index (mean Harvey- Bradshaw index of 8.4±5.55 vs. 6.3±5.16), a higher incidence of draining fistulae (23.3% compared to 9.4%), a longer disease duration (mean time since initial diagnosis 9.1±8.97 vs. 8.0±8.62 years) and increased medical hospitalizations in the 6 months prior to their baseline evaluation (42.8% vs. 37.9%). In addition, more patients in the IFX group were taking narcotic analgesics (8.7% vs. 5.8%), antibiotics (21.5% vs. 13.2%), azathioprine (57.1% vs. 50.4%), 6mercaptopurine (5.5% vs. 4.0%), and methotrexate (10.9% vs. 5.0%) when compared to the NBT group. Conversely, patients in the IFX group received less corticosteroid treatment at baseline (60% IFX vs. 66% NBT). The multivariate model, which adjusted treatment effect for selected prognostic variables, showed treatment with IFX or NBT was not an independent predictor of serious infection (p=0.30). Factors that were independently associated with serious infection included age (p=0.026), disease severity (p=0.024) and prednisone use (p=0.009). Conclusions: A Safety Analysis of IFX in CD confirms that corticosteroids, but not IFX, pose an increased risk for serious infection. Additionally, age and severity of disease were associated with occurrence of serious infections.