The Transition Model
advertisement
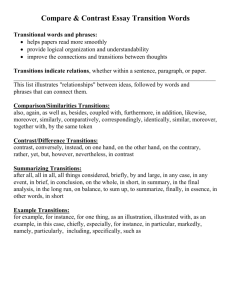
The Transition Model Candace Dreier, R.R.T. Welcome to today’s lecture. Our topic today is transition. Transition is caused by a provoking event that persists as a disruption of a situation and ends in change. Accommodating to change requires coping skills that require the participant to gain new knowledge, attitudes, and skills. Coping with change requires a realistic perception, an interpretation of new situations and experiences by everyone involved. The transition model involves a theory of learning as a conceptual change. It assumes that people strive to make sense of their experiences and situations using their existing knowledge. People develop patterns of knowledge with accompanying skills, attitudes, and beliefs which we refer to as conceptions. People construct conceptions in ways that are logical and useful based on their knowledge and experiences. Therefore, any two people exposed to the same events may perceive and interpret these events in different ways. Three types of conceptual learning issues may hinder transition. The first is any gaps in knowledge, attitudes or skills. The second involves confusions, which are knowledge, attitudes or skills that are undifferentiated or unclear. The third are errors or misconceptions. This is knowledge that is untrue, attitudes that are inappropriate, or skills that are ineffective. All these conceptions must be considered when interventions are proposed. Strategies that facilitate learning can help a person integrate new conceptions into their existing understanding, clarify confused conceptions, and change inappropriate conceptions. This instructional approach may involve a variety of techniques including lectures, written materials, demonstrations, videotapes, problem solving exercises, discussions, etc. The transition process begins and ends with the system in a stable state of equilibrium. In stage one, the individuals involved in the child’s care comprise the system based on common understanding and congruence. These individuals may include the family, hospital care team, home care nurses, teachers and others. The system is in equilibrium. When the patient enters a transition phase, the entire system may participate in the transition because of the various relationships of the individuals with the patient. An example of this type of transition would be an environmental transition. Imagine a family awaiting the birth of their first child. They live in a small one-bedroom apartment and the pregnancy at this point is going well and the child is expected to be born healthy. Upon the child’s birth, they find that she has special health care needs. She’s going to require a tracheostomy tube, a ventilator for continuous use, and a gastrostomy tube for feedings. Arrangements are being made for the child to be discharged from the hospital to home. In order to accommodate having the child at home, the parents will need to move from their small apartment to a larger place to store equipment and be able to house the child and the equipment and supplies. The parents are arranging a move into the maternal grandmother’s home. This will provide more room for the family and will also enable the grandmother to provide limited care for the child. The system has switched, or is in a state of equilibrium and is beginning the switch which we will discuss in stage two. In stage two, the transition is initiated by one or more provoking events that involve a number of changes. In our case, one of the main transitions is having the child be born with special health care needs. Another is the need to move from their current living situation. These changes require new knowledge, skills, and attitudes. These changes may cause disequilibrium in the system if individuals fail to understand the change. There may be gaps, errors, or confusion regarding an individual’s knowledge, attitudes, and skills concerning the provoking event. The resulting disequilibrium is uncomfortable and stressful. It may be perceived as potentially dangerous by the patient, family, or any other members of the care team. In stage three, coping represents the core of the transition process. A successful transition results from coping with change in knowledge, attitudes, and skills effectively by addressing the gaps, confusions, and errors. Successful transitions are facilitated by teaching interventions geared towards integration, differentiation, and exchange. Coping may be seen as the efforts made by participants in the system to re-establish a stable state. Interventions involve identifying the nature of the needs and deciding how to intervene. What strategies will be necessary? What methods to use? Who will intervene and when? A system strives for equilibrium or a stable state because stress, anxiety and discomfort are reduced and the perceived danger is eliminated or reduced. In stage four, equilibrium is established when participants once again find common understanding and congruence. In our example, the family learns the skills needed to take care of this child at home. They find and arrange their new living situation to accommodate their needs, and they have arranged for additional childcare for their child by having the grandmother participate in care. So they have again reached that state of equilibrium. The transition model provides an action plan for the care of complex illnesses involving multiple caregivers over long periods of time. Transitions begin with expected or unexpected provoking events. If transitions are anticipated, careful planning with training of all participants in the system will facilitate a successful transition. The care team can plan proactively by gauging the knowledge, attitudes, and skills of the patient, the family, and of the care providers. By teaching essential skills and providing information, they will facilitate the change process. Checklists that relate to anticipated transition points serve to document information that must be taught to families and caregivers. The care team uses checklists to help us track where we are in the process and how soon discharge can be accomplished. If the transition is unexpected, the upset in equilibrium may be noticed only when an individual (whether the parent, child, or care team member) becomes upset. This type of behavior indicates that the individual is having trouble coping with a new demanding situation. If this happens, the team must attempt to facilitate coping by all individuals with the goal of re-establishing equilibrium. One example of this would be using the same situation: the young child who is at home with a ventilator, trach tube and feeding tube. This child has been home now for two months. All has been going relatively smoothly. Parents and the home care nurses have developed a routine that seems to be comfortable for them while providing the required care to the child. Now over the past several days the child has developed a cough with increased secretions and therefore an increased demand for suctioning. This morning, following a coughing spell, the child appeared to have difficulty breathing. Her color seemed bluish, suctioning was attempted but did not solve the problem. The parents contacted the local Emergency Medical Service and the child was transferred by ambulance to the local emergency room. Obviously, this situation would cause the state of disequilibrium we discussed earlier. In spite of the fact that they were providing quality care to this child, they are not able to anticipate this type of transition or how successfully the transfer might occur. The transition model can be used retroactively to understand the success or failure of specific transitions. It is often helpful to review an unexpected transition, such as the one described, to see how things could or would go smoother in a similar situation in the future. The transition model provides a means to plan for transitions proactively ensuring that potentially provoking events are avoided through appropriate teaching at the right time. Another example of use of the transition model would be to look at a therapeutic transition. Imagine now that our child has been home and being cared for by family and home care nurses for three years. The child is now weaned off the ventilator and has been decannulated, which means the trach tube has been removed. Without the ventilator or trach tube, the parents are expected to provide all observations and all cares required by the child. Home care nursing will no longer be provided. This transition, although planned for, expected, and considered to be a positive transition, still creates stress in the family and still involves coping mechanisms in order for the family to successfully complete this transition. The transition model provides a means of understanding the dynamics of transitions that occur in the care of children with chronic illness and children dependent on technology to allow facilitation of smooth transitions.