A two-year-old Mascot boy has recorded a blood
advertisement

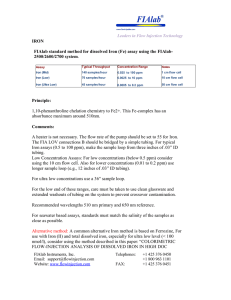
Jack, a 5 year old, is brought to the pediatrician by his mother, who is concerned that her child is hyperactive and vomiting. Subjective Data: Mother stated: Has been restless and easily distracted. At a parent teacher conference, his kindergarten teacher said that he has trouble concentrating and recommended evaluation by a physician as well as by the school psychologist. Has had a very poor appetite lately Complaining of abdominal pain Vomited last night and this morning Has been on iron supplements for “mild iron deficiency anemia” for the past three months. Has no known allergies Objective Data: Chart Review: last seen in clinical for preschool physical 1 year ago – results overall normal. A note describes a very active 4 year old who could dress himself without help but could not correctly name the primary colors. Vision was normal, hearing acuity below normal Speech and language slightly delayed. Immunizations up to date Good appetite – no pica Lab Work - Spun hematocrit was diminished at 30%. Peripheral blood smear showed hypochromia and microcytosis. There was no evidence of blood loss, and stool examination was negative for occult blood. Diagnosed at this time with "mild iron deficiency anemia," and iron therapy was prescribed. The family failed to keep several follow-up appointments, but the child did apparently complete the prescribed 3-month course of iron supplements. He receives no medications at this time and has no known allergies. Assessment: Minor muscle weakness and joint pain Attention span is very short, making him appear restless Irritable, trouble following simple directions Abdomen tender, soft In the tenth percentile for height and weight. Family History: Lives with his sister, mother, and maternal grandparents in an older suburb of your community. The child's monthly weekend visits to his father's house are working out fine. However, he seems to be fighting more with his sister who has an attention-deficit disorder and is repeating the first grade. Since the mother moved in with her parents after her divorce 4 years ago, she has worked with the grandfather in an automobile radiator repair shop, where her children often come to play after school. The mother was just laid off and expressed worry about increasing financial dependence on her parents. Lab Data: Hgb – 9.2g HCT – 30% Peripheral blood smear showed hypochromia and microcytosis. Stool examination was negative for occult blood. Lead - 50 micrograms per dl. Critical Thinking Questions: 1. What is the nurses first intervention? 2. What is the possible causes for the low hemoglobin? 3. What is the level at which lead is considered to indicate lead poisoning? What happens at 45-69 ug/dl? 4. The case study suggests several sources of lead in the boy's life. What are these sources? What questions will you ask to gauge the extent of the boy's exposure to each of these sources? 5. What questions will you ask the family to evaluate less obvious, but possible, sources of lead exposure ? 6. What would likely be revealed by an X-ray of the abdomen or long bones of a lead-exposed child? 7. Why does the blood lead level fail to drop within a few days, even with complete removal from the source of exposure ? 8. The laboratory results indicate that the blood lead level of the child in the case study is 50 mcg/dL. Chelation therapy is ordered. Explain rationale and nursing care. 9. Several weeks after chelation therapy and removal from the source of exposure, in some cases the patient's blood lead level is found to have increased again. What is the cause of this rebound phenomenon? 10. What are the major effects of lead on the human body? 11. What are pertinent nursing diagnosis related to Jack and related nursing interventions? 12. The nurse learns from the laboratory that the boy has a ZPP level of 350 mcg/dL. What are the possible causes of this elevated value ? (13) 0. What other laboratory tests will you now order to confirm or rule out your diagnosis? 13. Jack’s family ask what they can do to decrease the risk of this happening again. What patient teaching is appropriate in this case? 14. Who could the nurse you contact for additional information regarding Jack’s condition?