Do Not Resuscitate Orders (DNR)
advertisement

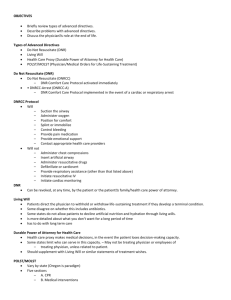
Do Not Resuscitate Orders (DNR) What is a Do Not Resuscitate Order? A Do Not Resuscitate order states that if the person goes into cardiac (heart) or respiratory (breathing) arrest measures to restart these functions should not be attempted. There are two types of Do Not Resuscitate Order: 1. Hospital Do Not Resuscitate Order- this order is entered into a patient’s chart while they are in the hospital 2. Nonhospital Do not Resuscitate Order- this type of Do not resuscitate order is for individuals who are in a nursing home or at home. The order informs emergency medical service personnel that resuscitation should not be attempted if this individual is suffering from cardiac or respiratory. NOTE: Every person is presumed to consent to resuscitation efforts in the event of cardiac or respiratory arrest, unless a Do Not Resuscitate order has been issued. Are there any limitations to Do Not Resuscitate Orders? Yes, a Do Not Resuscitate order only applies when a person is suffering from cardiac or respiratory arrest. © 2005 CDHS/ College Relations Group, Research Foundation of SUNY, BSC Will a Do Not Resuscitate Order effect the health care treatment that I receive? A Do Not Resuscitate order does not have an effect on the health care treatment that the person is receiving or will receive in the future. The person will not be deprived of pain relief or comfort care. How does a capable individual implement a Do Not Resuscitate Order? There is a presumption that every adult has the capacity to make their own decisions about CPR unless there is a medical determination or a court order that states otherwise. If a person is interested in entering a DNR order he or she should talk with his or her physician. Is there anything the attending physician needs to do before he/she can enter a Do Not Resuscitate Order for a capable person? Before an attending physician can enter a Do Not Resuscitate order the physician must: 1. Inform the patient about his/her condition, 2. Discuss the DNR order with the patient, 3. Explain the possible risks and benefits to the patient, 4. Describe the consequences of the DNR order to the patient, and 5. Obtain the consent of the patient, or in the case of an emergency, obtain the consent of the health care agent. © 2005 CDHS/ College Relations Group, Research Foundation of SUNY, BSC What happens if the attending physician does not agree with a patient’s decision to enter into a Do Not Resuscitate Order? If the attending physician does not agree enter a DNR order and the patient does not agree with the physician, then the physician can either: 1. Make arrangements for another physician to assume responsibility for the patient’s care, or 2. Refer the matter to the dispute mediation system in the health care facility. How is a Do Not Resuscitate Order revoked? A Do Not Resuscitate order is easily revoked. A patient or the patient’s health care agent can revoke their consent to a DNR order at any time by either an oral or written statement to a doctor or nurse or by any other action that demonstrates that the person intended to revoke the DNR order. How does an incapable person enter into a Do Not Resuscitate Order? If it is found that the adult lacks capacity, but this adult has a health care agent then this agent has the same power to make decisions regarding CPR that the patient would have had if they had the capacity. If it is found that a patient lacks the mental capacity needed to consent to a DNR order, and this patient does not have a health care agent, then a DNR order can still be issued under the following limited circumstances: © 2005 CDHS/ College Relations Group, Research Foundation of SUNY, BSC 1. After a personal examination by the attending doctor and another physician, both physicians agrees that to a reasonable degree of medical certainty, one of the following applies: a. the patient is terminal ill, or b. the patient is permanently unconscious, or c. Resuscitation would be medically futile, or d. “Resuscitation would impose an extraordinary burden on the patient in light of the patient’s medical condition and the expected outcome of resuscitation for the patient.” 2. If one of the above circumstances is met, a surrogate needs to be chosen to make a decision for the incapable patient. This surrogate needs to be chosen from the highest category of the following list which has been set out in the law: a. A committee for the person, Article 17-A guardian, or Article 81 guardian b. The patient’s spouse c. The patient’s son or daughter who is over the age of 18 d. The patient’s parent e. The patient’s sibling who is over the age of 18 f. A close friend of the patient. What are the limits to a surrogate’s authority? The surrogate’s authority to make decisions applies only to decisions involving CPR and not to any other health care treatment issues. © 2005 CDHS/ College Relations Group, Research Foundation of SUNY, BSC The surrogate’s decision must be based on what the surrogate believes are the patient’s wishes regarding CPR. The surrogate’s decision must take into account the patient’s religious and moral beliefs. If the patient’s wishes are not know and cannot be determined, then the surrogate must make the decision based on the patient’s best interest. In determining what is in the patient’s best interest, the surrogate needs to weigh the benefits of CPR versus the risks of CPR to the patient. Also, in order to make an informed decision, the surrogate is allowed the same access to the patient’s medical information as the patient would have. How does a surrogate’s consent to a Do Not Resuscitate Order? The surrogate can consent to a DNR order either orally or in writing. Oral consent must be given in the same way that a capable patient would give consent. Therefore, the surrogate’s oral consent must be given to two adults, one of which must be a doctor that is connected to the health care facility that the patient is being treated in. Written consent must be dated and signed in the presence of at least one witness who is over the age of 18, and this witness must sign the order. © 2005 CDHS/ College Relations Group, Research Foundation of SUNY, BSC What must the physician do when a surrogate consents to a Do Not Resuscitate Order? The physician’s responsibility towards the surrogate’s consent to a DNR order is the same as when a capable patient consents to an order. These responsibilities are as follows: When the attending physician is given or becomes aware that the surrogate has consented to a DNR order on behalf of an incapable patient, the attending physician can either: 1. Issue the DNR order, or 2. Inform the surrogate of any objections to the issuance of the DNR order. If the attending physician object to the issuance of the DNR and the surrogate does not agree with the physician’s objections, then the physician can either: 1. Make arrangements for another physician to assume responsibility for the patient’s care, or 2. The attending physician can “submit the matter to the dispute mediation system in the facility.” How does a surrogate revoke a Do Not Resuscitate Order? The surrogate can revoke his/her consent to a DNR order by: 1. Giving a written statement to a doctor or nurse at the health care facility, or 2. By giving an oral statement, in the presence of one adult witness. NOTE: An Article 81 Guardian cannot revoke a DNR order. © 2005 CDHS/ College Relations Group, Research Foundation of SUNY, BSC What if a surrogate is not available? An attending doctor can issue a DNR order if there is no surrogate that is “reasonable available, willing to make a decision regarding the issuance of an order not to resuscitate, and competent to make a decision,” and the adult patient does not have the capacity to make the decision and has not previously expressed a decision. In these circumstances, before issuing the order, the attending doctor needs to determine and place in writing that “resuscitation would be ‘medically futile’ to a reasonable degree of medical certainty.” This determination must then be reviewed and approved by another physician who is authorized by the health care facility. What should be done after a Do Not Resuscitate Order is in place? Once a patient has a DNR order in place, the order must be reviewed from time to time in order determine if it is still appropriate. How often the review takes place is determined by where the patient is 1. If the patient is in the hospital, then the DNR order must be reviewed by the attending doctor at least once every 7 days. 2. If the person is a resident of a nursing home then the order needs to be reviewed by the physician at every visit, but at least every 60 days. 3. For patients with a nonhospital DNR order, this order must be reviewed by the physician every time the patient is examined, but at least every ninety days, “providing that the review need not occur more than once every seven days.” However, a failure to review does not cancel the DNR order. © 2005 CDHS/ College Relations Group, Research Foundation of SUNY, BSC What if there is a dispute over a Do Not Resuscitate Order? Every health care facility is required to have a mediation system for disputes involving DNR orders in place. If a dispute arises regarding a hospital DNR order, then the parties are required to take their disagreement to the hospital’s dispute mediation system. The order cannot be issued or revoked until the dispute is resolved The provisions governing dispute mediation do NOT apply to nonhospital DNR orders. Are the decisions made in mediation final? Any dispute concerning a DNR order is subject to judicial review, except that there is no judicial review of a patient’s refusal to consent to a DNR order. The party challenging the decision to issue a DNR order must be able to show “by clear and convincing evidence that the decision is contrary to the patient’s wishes or alternatively that it is not in the patient’s best interest.” © 2005 CDHS/ College Relations Group, Research Foundation of SUNY, BSC Here is a sample New York Department of Health Nonhospital DNR order form: Person's Name ...................................... Date of Birth ... / ... / ... Do not resuscitate the person named above. Physician's Signature ........................ Print Name ................................ License Number ............................ Date ... / ... / ... It is the responsibility of the physician to determine, at least every 90 days, whether this order continues to be appropriate, and to indicate this by a note in the person's medical chart. The issuance of a new form is NOT required, and under the law this order should be considered valid unless it is known that it has been revoked. This order remains valid and must befollowed, even if it has not been reviewed within the 90-day period. Source: New York Public Health Law, Art. 29-B (§§ 2960-2979) © 2005 CDHS/ College Relations Group, Research Foundation of SUNY, BSC