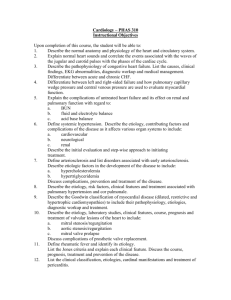
Learning Guide for Myocardial Infarction
advertisement
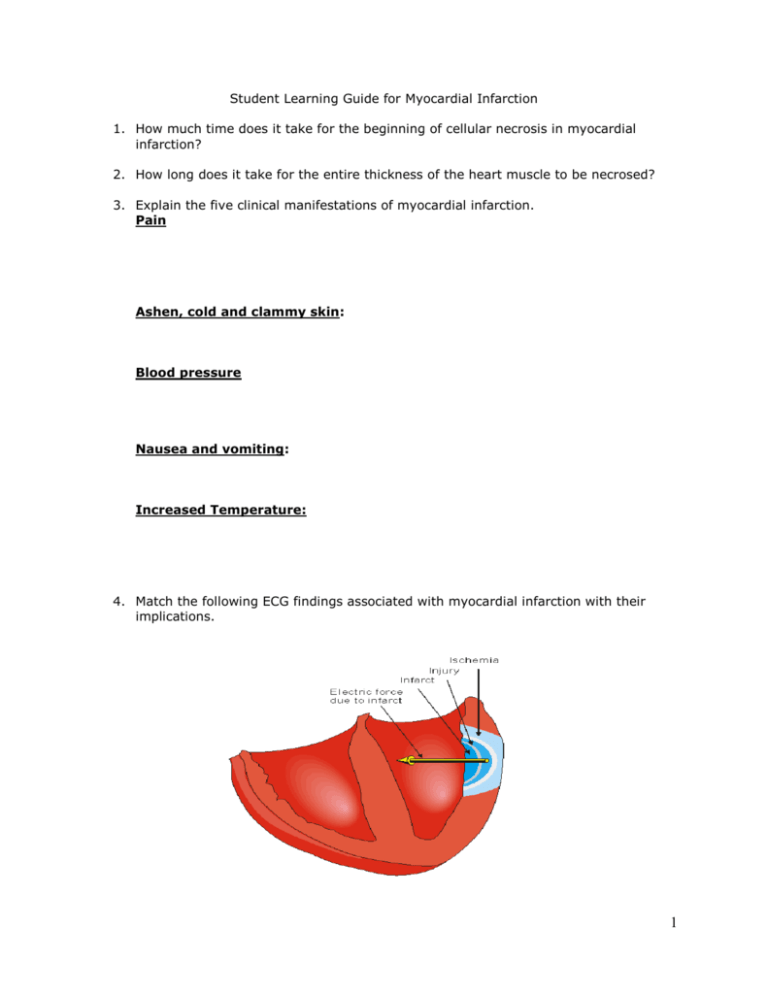
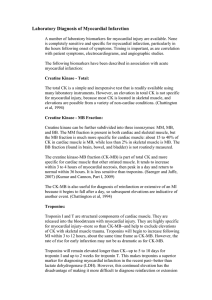
Student Learning Guide for Myocardial Infarction 1. How much time does it take for the beginning of cellular necrosis in myocardial infarction? 2. How long does it take for the entire thickness of the heart muscle to be necrosed? 3. Explain the five clinical manifestations of myocardial infarction. Pain Ashen, cold and clammy skin: Blood pressure Nausea and vomiting: Increased Temperature: 4. Match the following ECG findings associated with myocardial infarction with their implications. 1 _____ ST segment elevation A. Necrosis _____ T wave inversion B. Ischemia _____ Pathologic Q wave C. Injury 5. How does the heart heal from an MI? 6. Explain the seven complications of MI. Dysrhythmias Heart failure: Cardiogenic shock Papillary muscle dysfunction: Ventricular aneurysm: 2 Pericarditis: Dressler syndrome 7. Which tends to be more extensive, a STEMI or an NSTEMI? How does this manifest on the ECG tracing? 8. Fill out the following table on cardiac markers: (p. 781) Marker Time to peak Time to return to normal Myoglobin CK-MB Troponin 9. What is the goal of percutaneous coronary intervention (PCI). 10. List four advantages to percutaneous coronary intervention (PCI). 11. What are the most serious complications of PCI? 12. What are the initial interventions in someone with severe chest pain? 3 13. Describe the major nursing interventions post PCI. (Under cardiac catheterization on Table 32-6) 14. What are the absolute and relative contraindications for fibrinolytic therapy in the client with MI? Absolute: Active internal bleeding (except menstruation) History of cerebral aneurysm, cerebral hemorrhage or AV malformation Intracranial neoplasm Recent ischemic stroke within 3 months Significant closed-head or facial trauma within 3 months Suspected aortic dissection Relative: Active peptic ulcer disease Current use of anticoagulants Pregnancy Prior ischemic stroke greater than 3 months ago, dementia, or known intracranial pathology not covered in absolute contraindications Surgery within 3 weeks or puncture of non-compressable vessel Internal bleeding within 2-4 wks Serious systemic disease Severe uncontrolled HTN (>180/110) on presentation, or chronic severe poorly controlled HTN Traumatic or prolonged CPR (>10 min) 15. What is the goal of fibrinolytic therapy and within what time frame is it used? 16. What are the major post firbinolytic therapy complications? 17. What are the major indicators of reperfusion? 18. List three indications for coronary revascularization with CABG surgery. 4 19. Complete the following table. Drug Nitroglycerin Morphine Use/Action in MI/ACS Given for chest pain unrelieved by nitroglycerin. Vasodilates decreases cardiac workload and myocardial O2 consumption, reducing contractility, & decreasing BP and HR. Reduce anxiety & fear. Can depress respirations (rare); monitor for signs of bradypnea or hypoxia. Beta blockers (Negative Inotropic Drugs) Atenolol (Tenormin) Carvedilol (Coreg) Propranolol (Inderal) Stool softeners Constipation due to bed rest & opioids; stool softeners promote comfort & prevent straining/valsalva manuver ( Vagal stimulation bradycardia/dysrhythmias) Ace Inhibitors: Catopril (Capoten) Enalapril (Vasotech) Cholesterol-lowering drugs Statins lower LDL and reduce possibility of another MI 20. List manifestations of decreased cardiac output the nurse would assess following a myocardial infarction. 5 21. Identify priority nursing diagnoses, other than decreased cardiac output, for a client with a myocardial infarction? Explain the rationale for your choices. 22. List interventions used to facilitate the following treatment goals for a client with a myocardial infarction. Pain control Assess pain (intensity, location, radiation, duration, precipitating & relieving factors) Administer meds (nitro and/or morphine) 12 lead ECG if pain increases suddenly to r/o extension of MI or pericarditis Decrease cardiac workload Decrease anxiety Assess for verbal & nonverbal signs of anxiety Identify when level of anxiety changes (anxiety increases oxygen demand) Use calm, reassuring approach Instruct in relaxation techniques Encourage verbalization of feelings, perceptions, fears Provide factual info concerning diagnosis, treatment, & prognosis 23. List six common emotional and behavioral responses to MI. 24. Identify nursing responsibilities when administering: See table 33-8 on pages 748749. Medication category Platelet inhibitors Nursing Responsibilities ASA should be administered as soon as ACS suspected; watch for signs of bleeding; see contrainds for fibrinolytic therapy Narcotic analgesics Beta blockers Monitor pulse & BP regularly; use with caution in clients with diabetes; nonselective agents may cause bronchospasm, especially in clients with asthma ACE inhibitors 6 Thrombolytics Anticoagulants Assess for bleeding. Monitor PT, PTT, & INR. Review Precautions with students. Vasopressors 25. How will teaching needs change for a client with a myocardial infarction from the acute to the convalescent stages of the illness? 26. How many METS should the client be able to expend at the time of discharge? 27. What types of exercise should be limited post-MI? 28. What should the client be taught regarding pulse rate and exercise? (p. 791) 29. What should the client be taught about sexual activity post-MI? (p. 792) Plan resumption that corresponds to activity before hospitalization Physical training seems to improve physiologic response to sex; encourage daily physical activity Reduce eating/drinking ETOH before sex (wait 3-4 hrs after large meal) Familiar surroundings & familiar partner reduce anxiety Masturbation may reassure pt that sexual activity is still possible Avoid hot or cold showers just before & just after sex Foreplay allows gradual increase in heart rate before orgasm Oral-genital sex places no undue strain on heart Relaxed atmosphere free of fatigue & stress is best Prophylactic nitrates effective in reducing angina during sex Use of erectile agents contraindicated if taking nitrates 7 Anal stimulation can cause undue cardiac stress because of possibility of vasovagal response 30. What causes the majority of cases of Sudden Cardiac Death (SCD)? 31. List seven risk factors for SCD. 32. What is the most common approach to preventing a recurrence of SCD? 8