EMS-PEDIATRIC_SHOCK
advertisement

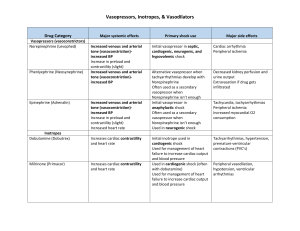
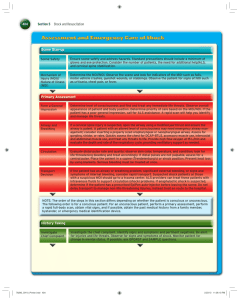
PEDIATRIC SHOCK Hemorrhagic, hypovolemic, septic, anaphylactic, spinal, OD/toxic, cardiogenic Pediatric Shock is well established before the appearance of classic signs and symptoms. The earliest sign is delayed capillary refill. This may also be accompanied by altered level of consciousness, rising pulse and increasing respiratory rate. By the time pulse, blood pressure and heart rate drop, death is near. FIRST RESPONDER 1. Open airway. Consider airway adjunct if airway not maintainable by head positioning or a towel under the shoulders 2. High flow O2, assist ventilation with BVM and suction as necessary 3. Hemorrhage control 4. Keep child warm and dry 5. Trendelenberg if tolerated 6. Request ALS EMT-BASIC 7. Pulse oximeter PARAMEDIC 8. Advanced airway as needed 9. Cardiac monitor / IV/IO 10. NG/OG tube: consider if abdominal distention a. Hypovolemic: 20 ml/kg bolus warm NS repeat to a total of 3 boluses if no improvement b. Distributive (sepsis, anaphylaxis, overdose/toxic exposure, spinal injury): i. Anaphylaxis with shock: 1. Epinephrine SQ 0.01 mg/kg 1:1,000 (max 0.3mg) 2. Epinephrine IV/IO 0.01 mg/kg 1:10,000 (max 0.1mg) must be added to 9cc NS to produce a concentration of 1:100,000 if patient in decompensated shock (hypotensive) or cardiopulmonary failure 3. Diphenhydramine 1mg/kg IV/IM 4. If wheezing, Albuterol 5mg and 0.5mg Atrovent nebulized, may repeat Albuterol as needed. ii. Sepsis, overdose/toxic exposure, spinal injury: 1. 20 ml/kg bolus warm NS 2. Dopamine 5-20mcg/kg/minute titrated to effect c. Cardiogenic: if history of congenital heart disease, consider cardiogenic shock i. Certain conditions have a normally very low SaO2. Ask caregivers what child’s normal saturation is and limit O2 to maintain. In hypoplastic left ventricle, BLUE IS BETTER ii. 10ml/kg warm NS with caution iii. Consider Dopamine 5-20mcg/kg/minute titrated to effect IF RESUSCITATION NEEDED USE BROSELOW TAPE! PINK 6