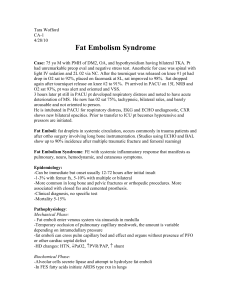
Fat embolism syndrome
advertisement

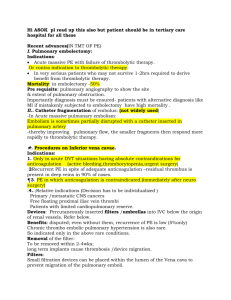
FAT EMBOLISM SYNDROME Incidence in Plastic Surgery Abdominoplasty – 1% Liposuction – case reports o 3 post mortems (J Forensic Sci 2002) showed 2 were due to FES, the other from fluid overload. 2 theories 1) mechanical - large fat droplets are released into the venous system. These droplets are deposited in the pulmonary capillary beds and travel through arteriovenous shunts to the brain. Microvascular lodging of droplets produces local ischemia and inflammation, with concomitant release of inflammatory mediators, platelet aggregation, and vasoactive amines. 2) biochemical theory - circulating or hydrolyzed free fatty acids in the pulmonary system activate acute-phase reactants, such as C-reactive proteins, and causes damage to the endothelial cells and pneumocytes. above. The biochemical theory helps explain delayed onset of fat embolism syndrome. Pathogenesis After being trapped in the pulmonary capillaries and hydrolyzed by a pulmonary lipase, free fatty acids cause direct toxic damage of the microvascular and alveolocapillary units and subsequently cause release of vasoactive amines and prostaglandins. The histopathology of FES is characterized by interstitial edema, transudate, and later exudate in the alveoli, the death of type II pneumocytes, and hyaline membrane formation. Clinical Fat embolism is a clinical diagnosis. Characterised by fever, acute respiratory failure, global neurologic dysfunction, and petechial rash occurring within 12-72 hours after surgery without evidence of cardiogenic pulmonary edema or sepsis 10-20% mortality rate CVS - Early persistent tachycardia CNS – acute delirium, stupor, seizures, or coma Resp - tachypneic, dyspneic, and hypoxic often febrile Skin (20-50%) – reddish-brown nonpalpable petechiae developing over the upper body, particularly in the axillae, within 24-36 hours of injury. Eyes - Subconjunctival and oral hemorrhages and petechiae also appear. Retinal hemorrhages with intra-arterial fat globules are visible upon funduscopic examination Investigations ABG – increased AA gradient FBC - Thrombocytopenia, anemia, and hypofibrinogenemia CXR - diffuse bilateral pulmonary infiltrates within 24-48 hours of onset VQ scan - often normal Pulmonary angiogram – rarely diagnostic Bronchoscopy lavage – most diagnostic - fat laden macrophages Treatment supportive maintenance of adequate oxygenation and ventilation and stable hemodynamics In most case reports - aggressive haemodynamic and respiratory support over 1-2 weeks required blood products as clinically indicated hydration prophylaxis of deep venous thrombosis and stress-related gastrointestinal bleeding, nutrition. Consider use of steroids – may be used as prophylaxis