Downloadable draft © - Guildford and Waverley CCG
advertisement

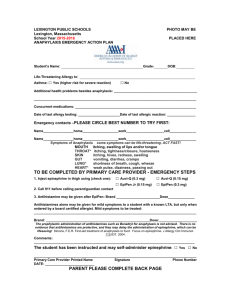
Lime Tree Surgery TREATMENT OF ANAPHYLAXIS INTRODUCTION Anaphylaxis (also called Anaphylactic Shock) is a sudden, severe, and potentially life-threatening allergic reaction caused by medications, food allergy, insect stings or substance allergy. The purpose of this protocol is to provide a summary of the immediate treatment required. EQUIPMENT AVAILABLE The Anaphylaxis Treatment kit is located in each treatment room and on crash trolley and is restocked by the practice nurse manager. Suggested content of an anaphylaxis pack 2 x ampoules adrenaline (epinephrine) 1:1,000 4 x 23g needles (green) 4 x graduated 1ml syringes Laerdal masks or equivalent suitable for children and adults KEY TO MANAGEMENT OF ANAPHYLAXIS Awareness Recognise it (consider in differential diagnosis) Treat quickly POSSIBLE SYMPTOMS (which may occur alone or in combination) Erythema Pruritus (generalised) Urticaria Angio-oedema Laryngeal oedema Asthma Rhinitis Conjunctivitis Itching of palate or external auditory meatus Nausea, vomiting, abdominal pain Palpitations Sense of impending doom Fainting, light headedness Collapse Loss of consciousness CAUSES Anaphylaxis can occur in response to almost any foreign substance even if it has been given, touched or eaten before. Anaphylaxis occurs as the result of a previously sensitised person coming into contact with or receiving the sensitising antigen (i.e., a substance capable of stimulating the formation of an antibody). Antigens known to be responsible for anaphylaxis include: Antibiotics and Other Drugs o o o o o o o o Foods o o o o o o o Fish and Seafood (particularly shellfish) Milk Eggs Nuts (particularly peanuts) Pulses Wheat Soy and Sesame Seeds Pollens and other inhaled allergens o o o o Penicillins Cephalosporins Nitrofurantoin Anti-seizure Medications NSAIDs Lignocaine Iron Dextran Plant Moulds Grasses Weeds Trees Animal/Insect Venoms o o o Bees/Wasps/Hornets Snake Spiders & Scorpions Other o o Rubber products Latex DIAGNOSIS Reactions usually begin within minutes of exposure, but may be delayed. Sometimes symptoms resolve, only to recur or progress a few hours later. The most dangerous symptoms are low blood pressure, breathing difficulties, shock and loss of consciousness, all of which can be fatal. Physiological Effect Capillary leakage Mucosal oedema Smooth muscle contraction Clinical Symptoms Urticaria Angio-oedema Laryngeal oedema Hypotension Laryngeal oedema Rhinitis Asthma Asthma Abdominal Pain/Cramp Vomiting/Diarrhoea Danger Asphyxia Shock Asphyxia Respiratory arrest Respiratory arrest TREATMENT The treatment depends on the severity of the attack. It may be possible to remove the cause of the attack (but don’t waste time – for example, in trying to remove insect ‘stingers’ as this will not stop the reaction). Assess the patient’s condition (ABC of Resuscitation - Airways, Breathing and Circulation) Mild Reaction: Make the patient comfortable. Put them in a sitting position to help breathing with legs slightly raised Give oxygen available from TR2, crash trolley, TR3 Call for help, i.e. dial 999, and seek another member of staff to assist, as well as requesting a doctor Observe blood pressure, pulse rate and respiratory rate (breathing) Sa)2 Moderate/Severe Reaction: AGE DOSAGE OF ADRENALINE (epinephrine) Under 6 months 150 mcg IM (0.15mls) Over 6 months but under 6 years 150 mcgs IM (0.15 mls) 6-12 years 300 mcgs IM ( 0.30mls) Over 12 years 500 mcgs IM (0.5mls) 300 mcgs IM if patient is small or prepubertal A suitable syringe for small volumes should be used. Record all batch numbers of medications used in the patient’s notes. The reaction should be reported to the Medicines Control Agency using the yellow card scheme at the back of the BNF. FURTHER MANAGEMENT Anti-histamines and/or Hydrocortisone are not recommended in the emergency anaphylaxis in Primary Care. They should be considered however, in the further management of anaphylaxis by appropriately trained staff. All health professionals responsible for immunisation must be familiar with techniques for resuscitation of a patient with anaphylaxis to prevent disability and loss of life. An anaphylaxis pack must always be available and a system in place to ensure the checking of expiry dates. Administer oxygen in as high a concentration as appropriate for the individual IV fluids if the patient is shocked and does not respond to drug treatment Salbutamol intravenously or by nebuliser (used to stop broncho-constriction which causes wheezing) FOLLOW-UP CARE Advise to avoid allergen if known (this may need investigation). Appropriate advice regarding the risk of recurrence Patients with a known propensity for anaphylaxis should be taught how to deal with an attack. If there is a chance that an attack might develop away from medical assistance, the patient and/or carer should be trained and equipped to inject adrenaline. Many patients prefer pre-assembled adrenaline-containing syringes, such as EpiPen or EpiPen Junior Advise to wear SOS Talisman, Medic Alert or similar device. It is important to ensure an allergic reaction warning is highlighted both on the Patients computer Notes as well as the Lloyd George notes For further leaflets and advice contact the: - www.resus.org.uk (Resuscitation Council UK) Review Date August 2013 Comment Staff Member MJ