Dr. Moore`s New Patient Questionnaire
advertisement

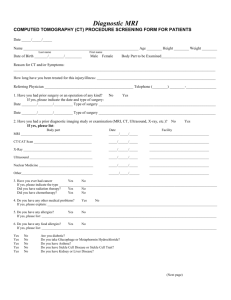
Dr. Moore’s New Patient Questionnaire Name: Age: Date: What problem would like evaluated today (e.g. left knee pain)? ______________________ ____________________________________________________________________________ On the body diagrams use the appropriate symbols to mark where you feel the following sensations: Numbness === Pins and Needles ooo Burning xxx Stabbing /// Aching ••• On the line below please indicate (with an X) how severe your pain is now. No Pain-----------------------------------------------------------------------------Worst possible pain 0 - 1 - 2 - 3 - 4 - 5 - 6 - 7 - 8 - 9 – 10 When did the problem start (approximately what date)? Did the problem result from trauma (e.g. an accident)? yes no If yes, please describe: ___________________________________________________ Have you been evaluated by a physician or received any treatment for this problem? yes no If yes, what treatments (check all applicable boxes)? Pain medicine Brace Physical Therapy Surgery Injections Alternative Medicine Other___________ If you have pain, what is it like (check all applicable boxes)? Sharp Dull Ache Episodic Constant Numb Burning Radiating Stiffness Swelling Joint feels unstable Other_________________________________________ Patient: Page 1 of 3 What makes your symptoms worsen? Motion Activity Bending Lifting Running Touch Standing Lying Sports Random Overhead activities What makes your symptoms improve? Physical Therapy Ice Alternative Meds Injections Exercise Massage Heat Sitting Nothing Early morning End of day Other _________________ Medicine Lying down Other_______________________ What is your height (in feet and inches)? __________ What is your weight (in pounds)? __________ Past Medical History: Please check (X) the box next to any problems that apply to you (or the patient if completing for a child). Heart disease Lung disease Kidney disease Eye disease Auto-immune disease High blood pressure Liver Disease/Hepatitis Diabetes Thyroid Disease Other endocrine disease Ulcers/Reflux Neurological disease Stroke Epilepsy Skin lesions or rash Bleeding/Easy bruising Sickle cell disease Other anemia Cancer Arthritis Gout or pseudogout Depression Other psychiatric disease None Other__________________________ Past Surgical History: Please list all surgeries you have had, their dates, and the hospital where the procedure was done. None Type of Surgery Date of Surgery Name of Hospital Have you had any of the following diagnostic studies performed? X-rays / radiographs CT (computed tomography) MRI (magnetic resonance imaging) EMG/NCV (electromyogram / nerve conduction velocity) Bone scan / nuclear medicine study Who is your primary care doctor or provider?________________________________ Medications: What medications do you take? ______________________________________________ ________________________________________________________________________ ________________________________________________________________________ ________________________________________________________________________ Patient: Page 2 of 3 Allergies: Please check (X) the box next to any allergies that apply to you. No Known Allergies Penicillin Sulfa Iodine Shellfish Cephalosporins Other antibiotics, medications, foods, or dyes:_________________________________ Do you have any difficulty taking anti-inflammatory medicines (e.g. Motrin)? Yes No Unknown Review of Symptoms: Please check (X) the box next to any problems that apply to you (or the patient if completing for a child). Fever or Chills Difficulty sleeping unintended weight loss Heat or Cold Intolerance Change in Gait Weakness Loss of control of bowel Loss of control of bladder Numb arm or leg Dizzy or light-headed Chest Pain Shortness of breath Night pain Endocrine/hormonal Psychiatric/emotional Other difficulties:________________________________________________________ Family History: Cancer Bleeding Problems Other Diabetes Sickle cell anemia Heart Disease Sudden death Stroke Arthritis Social History: Tobacco use: no yes if yes, packs per day_____, years of use _____ Alcohol use: no yes if yes, amount per week_________. Work status: employed unemployed disabled retired What is your occupation?_________________________________________ Marital status: single married divorced separated widow/widower Handedness: right left ambidextrous Developmental History: (complete if patient is an infant or child) Did pregnancy go to full term? yes no unknown Normal birth / normal first exam? yes no unknown Normal motor developmental milestones? yes no unknown Normal verbal developmental milestones? yes no unknown Are immunizations up to date? yes no unknown Is the child generally healthy? yes no unknown If you answered “no” to any of the above questions, please elaborate below: ________________________________________________________________ ________________________________________________________________ Doctor’s Notes: Patient: Page 3 of 3