NHS Dorset - Dorset CCG
advertisement

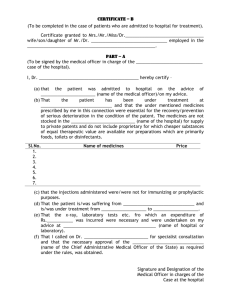
Keep Taking the Tablets Newsletter Issue 19 – December 2014 Quick bites… Medicines Health Regulatory Agency (MHRA) Drug Safety Update Medicines safety – Agomelatine Agomelatine has a “not recommended” status on the pan-Dorset prescribing formulary. Risk of hepatitis and hepatic failure with agomelatine treatment is an existing safety consideration, however, the MHRA advice in the November 2014 edition of Drug Safety Update reminds prescribers of the importance of monitoring liver function, after a recent European review revealed poor clinical compliance with recommended liver function monitoring. Baseline liver function tests (LFTs) should be carried out in every patient before starting treatment and repeat LFTs should be carried out at 3, 6, 12, and 24 weeks after starting treatment and regularly thereafter when clinically indicated, particularly if the dose is increased. Treatment should be stopped immediately if serum transaminases exceed three times the upper limit of normal, or if patients have symptoms or signs of suspected liver injury. Changes to paediatric amoxicillin doses A study recently published in the British Journal of General Practice concluded that a significant proportion of community penicillin prescriptions for children are at potentially sub-therapeutic doses. In line with guidance from the Health Protection Agency, the dose of amoxicillin recommended in the BNF and BNFC has recently been doubled to ensure that all children receive an adequate dose. The doses are now: Child 1 month to 1 year: 125mg TDS, increased if necessary up to 30mg/kg TDS. Child 1-5 years: 250mg TDS, increased if necessary up to 30mg/kg TDS. Child 5-12 years: 500mg TDS, increased if necessary up to 30mg/kg (max 1g) TDS. Child 12-18 years: 500mg TDS; in severe infection 1g TDS. Outpatient consultations and issue of prescriptions for recommended treatments The Medicines Management Team has recently received several enquiries about whether patients should be issued with a hospital prescription for medicines recommended following an out patients appointment. For clarification: There are circumstances in which a patient may be told to obtain a recommended medication from their GP. These circumstances will usually involve medications that do not require urgent initiation or titration by the specialist, and medications with a ‘green’ traffic light status, which are routinely used in primary care. In these cases the hospital may ask the GP to initiate treatment and therefore the hospital would not provide a supply. The rules for traffic light status would stand: for ‘amber’ drugs it is expected that the hospital would provide an initial supply as the consultant would initiate, and hand over once the patent is stable or as per the shared care agreement. For ‘red’ drugs prescribing must stay with the consultant permanently. For medications that require urgent initiation, even if they have a ‘green’ traffic light status, the hospital should supply. If there are examples of where clearly urgent medicines are not supplied the practice should raise through the GP niggles system so it can be followed up with the Trust concerned. Note that following an outpatient appointment, should a treatment should be required on a one-off basis, it would be pragmatic for the hospital to supply, to avoid the patient needing excessive appointments. This newsletter is for healthcare professionals and must not be discussed with persons outside the NHS. It represents what is known at the time of writing so information may be subsequently superseded. Sending medicines to foreign countries via companies such as Intercare Patient returned medicines should not be re-used in any way, including sending them abroad. This is based on historical guidance from the Royal Pharmaceutical Society, before it split into the Royal Pharmaceutical Society and the General Pharmaceutical Council. This guidance states that “no medicine supplied to or returned by an individual patient is included” for drug donations to developing countries. The World Health Organisation guidance on drug donations also says that there should be no “double standards” when donating medicines, specifically: “Donating returned medicines (unused medicines returned to a pharmacy for safe disposal) is an example of a double standard because in most countries their use would not be permitted owing to regulations on quality control.” Additionally, supplying any schedule of controlled drug as part of such schemes is likely to be a criminal offence. Following the Tsunami 10 years ago, Indonesian authorities ended up with warehouses full of unwanted medicines to safely destroy at excessive cost to the country. It is the advice of the CCG Medicines Team that if you or your patients want to help these countries, donate money to appropriate charities rather than donating medicines. Use of lactose free infant formula vs extensively hydrolysed formula In the last 12 months, there have been 809 items of lactose free infant formula prescribed in primary care. In line with the CCG policy for cow’s milk protein allergy (CMPA), prescribers are reminded that the incidence of cow’s milk protein allergy is on average 3%, whilst primary lactose intolerance is extremely rare. Lactose intolerance is the only scenario where lactose free milk formula should be used in primary care and, if used, the infant should be tried back on normal formula after 6-8 weeks. At this stage, if the infant is not able to tolerate a change to normal formula, a referral to secondary care should be made. If non IgE-mediated CMPA is suspected then in line with the policy for prescribing infant formula and associated pathway and formulary, an Extensively Hydrolysed Formula (EHF) should be recommended. The first line formula for this purpose on formulary is Nutramigen Lipil (either 1 or 2, depending on the age of the infant). Parents should be discouraged from changing brand of standard infant formula, as this will not improve symptoms and may delay diagnosis of CMPA. Risk of serotonin syndrome All practices are reminded of the risk of serotonin syndrome when prescribing, particularly fentanyl patches, tramadol, and antidepressant drugs (particularly SSRIs and SNRIs), even when these drugs are used at licensed doses. The risk is increased when these drugs are used concomitantly. A recent review has resulted in a warning that potentially life-threatening serotonin syndrome may occur with the concomitant use of fentanyl patches and other serotonergic drugs. UK Medicines Information has also published a Medicines Q&A about the risk of serotonin syndrome when tramadol and SSRIs are used concomitantly. Advice: Healthcare professionals should be aware of the potential for serotonin syndrome when prescribing any serotonergic medication. Where possible, avoid prescribing serotonergic medication concomitantly, but where it is considered essential, ensure that the patient is monitored appropriately, at initiation of treatment, after dose changes, and on discontinuation of the drug(s). Ensure patients are appropriately counselled to stop taking the medicine(s) concerned and seek medical advice if they experience signs or symptoms of serotonin syndrome, such as: confusion, agitation, muscle twitching, sweating, shivering, diarrhoea, and in severe cases, a very high temperature, seizures and irregular heartbeat. This newsletter is for healthcare professionals and must not be discussed with persons outside the NHS. It represents what is known at the time of writing so information may be subsequently superseded. Roll out of electronic prescribing in Dorset County Hospital Dorset County Hospital has been rolling out electronic prescribing (known as EPMA) throughout the Trust for in-patients. GPs will already be familiar with the electronic discharge summaries and this has not changed. However, they are due to roll-out electronic prescribing to on-site outpatient clinics from the middle of January (satellite clinics will continue using handwritten FP10s). It is hoped that the electronic prescriptions will increase safety and be more legible than existing hand written prescriptions. If there are any clinical queries, then these should be directed via the hospital switchboard to the prescriber (number will be printed on the prescription). If there are any technical issues with the electronic prescriptions (e.g. the printing/formatting) then these should be directed to the DCH electronic prescribing team, contactable on 01305 254191. The document below is a sample of the electronic prescriptions that community pharmacies and GP practices will start to see from mid-January (double click to open). Sample DCH FP10.pdf Update on shortage of steroid creams manufactured by GSK GSK have issued an update on current shortages and intermittent supplies of dermatology products. They have created a dedicated supply section on their website which will be updated on a weekly basis. A list of products and their stock status is available to download. This list may assist prescribers in assessing what stock pharmacies are likely to have available and which items can go on repeat. Important changes to the packaging of GSK’s Relvar® Ellipta® GSK are making a number of changes to the packaging of Relvar Ellipta®. The colour change is in response to the practical insights and feedback that GSK has received from a number of professional and patient organisations. Given the common practice in the UK of referring to short acting beta agonists (SABAs) as “blue inhalers”, the change will further support the clear distinction between Relvar and SABAs in clinical practice. Old packaging: New packgaging: Existing stocks of old packaging will be used up first and patients can be reassured that there is no change to the medicine or functionality of the inhaler, and to carry on with their treatment as advised by their prescriber, whether the medicine is in the blue or yellow packaging. Leaflets to assist communication of these changes to patients can be printed directly from the Relvar website. Specialist medicines advice can be obtained from the Medicines Information Centre at Southampton General Hospital: 023 8120 6908 or 023 8120 6909 or e-mail medicinesinformation@uhs.nhs.uk This newsletter is for healthcare professionals and must not be discussed with persons outside the NHS. It represents what is known at the time of writing so information may be subsequently superseded.