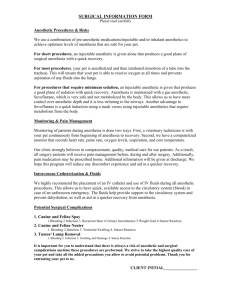
Anesthesia and Anesthetics Anesthetics: a substance that produces
advertisement

Anesthesia and Anesthetics Anesthetics: a substance that produces anesthesia, as halothane, procaine, or ether. Anesthesia: - (from Greek an- "without"; and, aisthēsis, "sensation"), Meaning insensibility or not feeling produced by agents which depress the activity of nervous tissues either locally or centrally. OR: Anesthesia is defined as total loss of sensation in a body part or the whole body, induced by a drug or drug combination that depresses activity of nervous tissue peripherally (local and regional anesthesia) or centrally (general anesthesia). OR: Anesthesia is a state of unconsciousness produced by a process of controlled, reversible drug – induced intoxication of the CNS in which the patient neither perceives nor recalls noxious stimuli. Types of Anesthesia* Anesthesia is often classified according to type of drug and method or rout of drug administration: 1- Inhalation 6-Transcutaneous Electric Nerve Stimulation (TENS, TNS, TES) 2- Injectable 3- Oral or Rectal 7- Hypnosis 4- Local and Conduction 8- Acupuncture 5- Electronarcosis 9- Hypothermia Indication for anesthesia: 1. Cast application. 2. To capture wild and vicious animals. 3. For diagnosis procedures. 4. To control convulsion (Epilepsy – tetanus). 5. For application of surgical and obstetrical procedures. 6. Euthanasia. Page 1 of 29 Factors affecting general anesthesia: 1. Age: - very young and old animals are more sensitive to anesthesia in comparison to an adult animal. 2. Size and body weight: - The small size animals with higher metabolic rate need large doses of anesthesia per kg body weight. 3. Sex: - Males need more anesthesia than females. However pregnant females are more susceptible due to high metabolic rate. 4. Species of animals: - There are species spesifity and variation. 5. Physical condition of the patient. 6. Pre anesthetic medication and previous drug administration. 7. Type of surgical procedure. Summary of Anesthetics (for reading only) Local Anesthetics General Anesthetics Inhaled injectable Bupivacaine -Enflurane Barbiturates Lidocaine -Halothane Benzodiazepines Procaine -Isoflurane Opioids Tetracaine -Methoxyfurane Neuroleptic -Nitrous oxide Dissociative -Sevoflurane inhalation anesthetic agent Liquid Gas 1- Ether 1- Cyclopropane 2- Haothane 2- Nitrous oxide 3- Chloroform 3- Ethylene 4- Methoxy flurane 5- Fluroxene 6- Ethyl chloride 7- Trichlor ethylene Page 2 of 29 Local anaesthesia (analgesia) Mean temporary loss of sensation in a defined body area without loss of consciousness. Advantages of local anesthesia: 1- In large animals necessity of casting is avoided. 2- It is easy to perform. 3- Toxicity less than general anesthesia. 4- Useful in patient condition not allowed performing general anesthesia. 5- Post anesthesia risk is reduced. Contraindications: 1- When there is hypersensitivity to local anesthesia drugs. 2- There is a danger of necrosis in site due to effect of local anesthesia drug on the blood circulation. Qualities of idea local anesthetic drug: 1- It should be water soluble, stable in solution and easily sterilized. 2- It should have lower systemic toxicity. 3- It should have good penetrating power. 4- It should have rapid onset and long duration of action. 5- It should be not irritant, not painful, and not cause tissue damage. 6- It should have high potency in low concentration. 7- It should be compatible with adrenaline. Note: - Local anesthetic agents are divided into two classes: (1) Esters (e.g. Procaine) Metabolized by pseudocholinesterases (2) Amides (e.g. Lidocaine, Bupivacaine) Metabolized by liver enzymes - Agents are bases and are charged in acidic media (inflamed tissue). Toxicity: Local anesthetic can produce toxicity two types of symptom, of toxicity: Local symptoms: - include ischemia and necrosis at site of injection. Systemic symptoms: - observed when local anesthetic drug reaches the toxic level in circulation, which leads to: 1- Decreased cardiac output. 2- Excitement. 3- Nausea and vomiting. 4- Convulsion. 5- Salivation. 6- Coma and death. Page 3 of 29 Precautionary measures against toxicity: 1- Decrease necessary dose should be used. 2- Decrease concentration of drugs but should be effective. 3- Aspiration prior to any injection to avoid injection directly to mean blood vessel. 4- Addition of adrenaline to slowing the absorption. 5- Use of premedication prior to the use of local anesthetic drug. Substances commonly used: 1- Cocaine. It is no longer in common use as of synthetic compound have replaced it. Moreover, it is a strong protoplasmic possession and produces toxicity on absorption. It is being mentioned here as a historical fact. 2- Procaine hydrochloride. Drug: Procaine (Novocaine) Class: Local anesthetic (ester linked) MOA: Blocks sodium influx and thus prevents nerve depolarization and conduction DOA: 60–90 min; ROA: (local infiltration) Effect: Blocks pain, motor, and sympathetic fibers Adverse: May cause allergic reaction Approved: None Note: Is white transparent crystalline powder which is freely soluble in water and easily sterilized. It is less toxic than cocaine. Procaine hydrolyzed by liver and blood stream. It is used for infiltration and spinal analgesia. It is used in 1% with or without adrenaline. Its effect begins within 3-5 minutes after injection and persists for one hour. Page 4 of 29 3- Lidocaine hydrochloride (xylocaine) Drug: Lidocaine (Xylocaine): 2.0% Class: Local anesthetic agent (amide) MOA: Blocks sodium influx and thus prevents nerve depolarization and conduction DOA: 90–200 min; ROA: (epidural, local infiltration) Effect: Blocks pain, motor, and sympathetic fibers; also used IV to treat ventricular arrhythmias Adverse: Hypotension due to vasodilation; respiratory arrest is possible when given epidurally; seizures at high doses Approved: None Note: Commonly used, it is a white powder is readily soluble in water. It is more effective local anesthetic particularly for per neural and spinal injection. It is 3 times more potent than procaine. The addition of adrenaline increases the duration of anesthesia. It is tends to diffuse more widely and easily in tissues. It is used in 1-2% and in 4% for surface anesthesia. The onsets of action begin 1-2 minutes after injection and persist for 1-2 hours. 4- Tutocaine: It is readily soluble in water and stable. It is more potent infiltration anesthetic than procaine. It is used in 2_4 % and the onset of action within 3-5 minutes after injection and persist for 2 hours. Page 5 of 29 5- Bupivacaine:. Drug: Bupivacaine (Marcaine**): 0.5% Class: Local anesthetic agent (amide) MOA: Blocks nerve transmission by blocking Na channel and preventing excitation conduction process DOA: 4–6 hr; ROA :( epidural, local infiltration) Effect: Reversible prevention of nerve transmission; thus motor, sensory, and autonomic function is temporarily inhibited Adverse: CNS excitation, seizures, respiratory paralysis, hypotension, hypothermia, ventricular arrhythmias Approved: None Note: It is four times as potent as lignocaine with longer duration of action for that it is indicate where prolonged analgesia is required Drug Lidocaine Mepivcaine Bupivacine Onset Fast Fast Medium Duration(hr) 2–4 1–3 4 - 10 Page 6 of 29 Local Anesthetics in clinical use Esters Amides - Benzocaine - Articaine - Chloroprocaine - Bupivacaine - Cocaine - Cinchocaine/Dibucaine - Cyclomethycaine - Etidocaine - Dimethocaine/Larocaine - Levobupivacaine - Piperocaine - Lidocaine/Lignocaine - Propoxycaine - Mepivacaine - Procaine/Novocaine - Prilocaine - Proparacaine - Ropivacaine - Tetracaine/Amethocaine - Trimecaine Combinations Naturally derived local anesthetics * Local anesthetics mixed with other - Saxitoxin local anesthetics include - Neosaxitoxin - Lidocaine/prilocaine (EMLA) - Tetrodotoxin - Lidocaine/tetracaine (Rapydan) - Menthol * Local anesthetics and - Eugenol vasoconstrictors Examples include: - Prilocaine hydrochloride and epinephrine (trade name Citanest Forte) - Lidocaine, bupivacaine, and epinephrine (recommended final concentrations of 0.5%, 0.25% and 1:200, respectively) Page 7 of 29 Notes:1- Clinically useful local analgesic drugs are: 1- Cocaine 2- Procaine (trade name Novocain) 3- Amethocaine (1% instillation into the eye; 2% used for the pharynx and nasal m.m) 4- Cinchocaine (Nupercaine) 5- Lignocaine 6- Prilocaine 7- Bupivacaine 2- Factors which influence the systemic absorption and potential toxicity of local analgesics (local anesthetics) are:1- The site of injection 2- The dosage. 3- The addition of vasoconstrictor agents 4- The pharmacological profile of the agent itself. Properties of Selected Local Anesthetic Agents Used in Veterinary Medicine (For reading only) Agent(Trade Name) Procaine (Novocaine) Chloroprocaine (Nesacaine) Lidocaine(Xylocaine) Mepivacaine(Carbocaine) Bupivacaine(Marcaine) Tetracaine (Pontocaine) Class Potency* Lipid Solubility pKa Protein Binding Onset of Effect Duration (min) Ester Ester Amide Amide Amide Ester — 1 2 2 8 8 1 1 3.6 2 30 80 8.9 9.1 7.7 7.6 8.1 8.6 6% 7% 65% 75% 95% 80% Slow Fast Fast Fast Intermediate Slow 60–90 30–60 90–200 120–240 180–600 180–600 *Potency is relative to procaine (1). Page 8 of 29 Summary on some local anesthetics used in veterinary clinic (For reading only) Drug Bupivacaine (Marcaine**): 0.5% class Local anesthetic agent (amide) MOA Blocks nerve transmission by blocking Na channel and preventing excitationconduction process DOA 4–6 hr; (epidural, local infiltration) Lidocaine (Xylocaine**): 2.0% Local anesthetic agent (amide) Blocks sodium influx and thus prevents nerve depolarization and conduction 90–200 min; (epidural, local infiltration) Mepivicaine (Carbocaine-V): 1–2% Local anesthetic agent (amide) Blocks sodium influx and thus prevents nerve depolarization and conduction 120–240 min; (epidural, local infiltration) Procaine (Novocaine) Local anesthetic (ester linked) Blocks sodium influx and thus prevents nerve depolarization and conduction 60–90 min; (local infiltration) Effect Reversible prevention of nerve transmission; thus motor, sensory, and autonomic function is temporarily inhibited Blocks pain, motor, and sympathetic fibers; also used IV to treat ventricular arrhythmias Blocks pain, motor and sympathetic fibers Blocks pain, motor, and sympathetic fibers Adverse CNS excitation, seizures, respiratory paralysis, hypotension, hypothermia, ventricular arrhythmias Approved Non Hypotension due to vasodilation; respiratory arrest is possible when given epidurally; seizures at high doses Hypotension due to vasodilation and respiratory arrest are possible when given epidurally; seizures and cardio toxicity with overdose May cause allergic reaction None None None MOA: is mechanism of action; DOA: is duration of action, these numbers are only guidelines as DOA is influenced significantly by concurrently administered drugs and individual patient status). Route of administration for every agent is listed in parentheses after DOA and includes intravenous (IV), intramuscular (IM), subcutaneous (SC), and per os (PO). In general, the onset of effect occurs within 5 minutes for drugs administered intravenously. When drugs are administered intramuscularly, onset of effect is in 15 minutes; subcutaneous administration requires a slightly longer time to take effect (20–30 minutes). Common trade names (USA; UK* or USA and UK**) for some of the agents have been listed in parentheses after the chemical name. Page 9 of 29 Local anesthetic theories: Several theories regarding the mechanism by which local anesthetics cause a decrease in cellular excitability have been postulated 1- Membrane stabilization theory 2- Control of ionic "gates" theory 3- Receptor inhibition theory Local Anesthetics - Drugs which block impulse conduction in nerves. Act to block voltage-sensitive sodium (Na+) channels in nerve membranes Disrupt the action potential Most effective on small unmyelineated fibers applied topically or injected around nerves. Mechanism of action: At rest high concentration of sodium ions occur outside the cell and reverse for potassium ions How do local anesthetic drugs work by block cell permeability Page 10 of 29 Mechanism of action: Depolarization occurs when sodium channels open and flow inward How do local anesthetic drugs work by block cell permeability Mechanism of action: Local anesthetics block the sodium channel to open by prevention the binding between calcium and the phospholipids in the cell membrane Page 11 of 29 General anesthetics General anesthesia: - It is complete unconsciousness produced by a process of controlled, reversible intoxication of C.N.S. in which there is muscle relaxation and diminished to external stimuli. General anesthetics A general anesthetic is a drug that has the ability to bring about a reversible loss of consciousness. Anesthetists administer these drugs to induce or maintain general anesthesia to facilitate surgery. Some of these drugs are also used in lower dosages for pain management. Types of general aesthetics Injectable mainly IV Sometimes IP or IM Gas inhalation Liquid Or anesthetic agents Divided into 1. Nonvolatile or injectable agents of drugs. 2. Volatile or Inhalation anesthetic agents or drugs. Injection anesthesia (mainly i.v.) differ from inhalation anesthesia by:1- Mainly administered i.v. but some time i.m., i.p. 2- Lack of control, which mean once the drug is administrated nothing could be done for it removal. 3- They are used for short operation procedure, but recently they used for long operations by repeated dose of by continuous infusion. 4- Anesthesia induced easily and recovery is fast. 5- The stages of anesthesia which is seen in inhalation anesthesia are not seen in injection anesthesia, because the onset is very rapid. Inject able or non-volatile general anesthetic drugs Advantages of use: 1. It dose not required costly equipment and attained staff and constant supervision. 2. It can be used in field condition. 3. It is good for short duration surgery or diagnostic procedure. 4. It is good for indication of anesthesia, which is to be maintained by an inhalation technique. 5. It is not-explosive and non-inflammable. Page 12 of 29 Disadvantages: 1. After administration of inject able anesthetic drug one has no control to reverse the depth of anesthesia. 2. Intravenous anesthetic drugs depends on body system for its metabolism, detoxification and excretion for that it is dangerous in animals with damaged liver and kidneys. 3. The recovery period may be long and stomy. 4. Oxygen and respiratory support equipment may be not available. Characteristics of an ideal injectable anesthetic I- Physiochemical and Pharmacokinetic 1- Water soluble 2-Long Shelf life. 3- Stable when exposed to light. 4- Small volume required for induction of anesthesia. II- Pharmacodynamics 1- Minimal individual variation. 2- Safe therapeutic ratio. 3- Onset, one vein to brain circulation time. 4- Short duration of action. 5- Inactivated to nontoxic metabolites. 6- Smooth emergence. 7- Absence of anaphylaxis. 8- Absence of histamine release. III- Side Effects 1- Absence of local toxicity. 2- No effect on vital organ function except anesthetically desirable CNS effect. Page 13 of 29 Injectable anesthetic agents can be divided into:Anesthetic agents (injectable) Rapidly Acting Less Rapidly Acting i.v. anesthetic agents 1-Thiopental Sodium 1- Chloral hydrate (Barbiturate) 2Methohexital Sodium 2- Chloralose (Barbiturate) 3- Saffan (Steroids) 3- Urethane 4- Minaxolone (Steroids) 4- Pentobarbital Sodium (Barbiturate) 5- Metomidate (Steroids) 5- Dissociative agents: 6- Etomidate (Steroids). 1. Phencyclidine 7- Eugenols 2. Tiletamine. 8- Propofol 3. Tiletamine – Zolazepam. 4. Ketamine Or another classification for injectable anesthetics Injectable anesthetics Barbiturate Non Barbiturate Althesin (Saffan) - Oxybarbiturates Phenobarbital Sodium Chloralhydrate, U.S.P. (Phenobarbital), U.S.P. Pentobarbital Sodium, U.S.P. Chloraose (Nembutal) Methohexital Sodium (Brevital) Urethane, N.F. Magnesium Sulfate - Thiobarbiturates Thiopental Sodium, U.S.P. Metomidate (Hypnodil) (Pentothal) Thiamylal Sodium (Surital) Etomidate (Amidate) Propofol (Rapinovet, Diprivan) Propanidid (Epontol) Tricaine Methanesulfonate (MS-222; Finquel) Page 14 of 29 Dosage calculation If the concentration was % then you can multiply with 10 e.g. 10% = 5*10= 100 mg/ml Anesthetic agents (Injectable) (1) Rapidly Acting 1- Thiopental Sodium (Barbiturates) (Pentothal) Drug: Thiopental (Pentothal; Intraval): Class: Ultrashort-acting thiobarbiturate MOA: Sedative/hypnotic; CNS depression by action on barbiturate receptors DOA: <15 min; ROA:(IV) Effect: Sedation to unconsciousness (dose dependent), stage II delerium can occur with inadequate or perivascular dosages Adverse: Respiratory depression (apnea), myocardial depression, cardiac arrhythmias Approved: Dogs Note: Used in Vet Med. since 1937 and from then is the widely used agent especially in dogs and cats, after i.v. injection it reach CNS and its effect become apparent within 15 – 30 seconds of injection. The animal reach surgical anesthesia within 1- 2 minutes. o It need to pre-anesthesia analgesic because it lack of analgesic properties. o It cause respiratory depress, laryngeal and bronchial spasm, hypotension in rapid injection, myocardial depression, cardiac arrhythmia. It used also in horses. Page 15 of 29 2- Methohexital Sodium (Barbiturates) (Brevital) Drug: Methohexital (Brevital; Brevane; Brietal): Class: Ultrashort-acting oxybarbiturate MOA: Sedative-hypnotic; CNS depression by action on barbiturate receptors DOA: <15 min ROA: (IV) Effect: Sedation to unconsciousness (dose dependent) Adverse: Respiratory depression (apnea), myocardial depression, excitement, muscle tremors, seizures during recovery Approved: None Notes: Its potency is 2-3 times greater than thiopental and it duration of action is shorter. The recovery is rapid than thiopental even in prolonged anesthesia. It given in dogs, cats, and horses. It recovery is fast but muscle tremor occur and sometime convulsion. 3- Saffan Steroidal preparation containing two pregnanediones (alfaxalone and alfadolone acetate) and used for the induction of anesthesia. Induces short-term anesthesia immediately when administered intravenously. Called also CT 1341. Saffan is a member of steroids (as mentioned above), it used in all domesticated animals but not for dogs because it cause histamine release. It causes hypotension dependence on dose. It causes good muscle relaxation. It is mainly excreted with bile. It not available since 1984. Note (for reading only): - Alfaxalone (trade name and other names = Alfaxan. Previous name was Alfaxalone). Is chemically alfaxalone -2- hydroxypropyl – beta – cyclodextrin (HPCD). It is synthetic neuroactive steroid that interact with GABA receptors in the CNS to produce anesthesia and muscle relaxation. 4- Minaxolone (Steroid) It cause smooth anesthesia, but prolonged recovery times. It is withdrawn from market. Page 16 of 29 5- Metomidate (Steroid) It is imidazole derivatives, it use mainly in pigs, it has a strong CNS muscle relaxant, but little ability to suppress response to painful stimulation. Note (for reading only): Metomidate Hcl, was discovered in 1965 and under the names (Hypnodil, Nokemyl) is sold as a sedative-hypnotic drug. General anesthesia can be produced by combining it with neuroleptics or analgesics. 6- Etomidate (Steroid) It used in dog. It duration of action is 10 – 20 minutes in dogs. I.V. injection may cause muscle tremor, involuntary movement of muscle, but this could be avoided by using Diazepam, Fentanyl or Pethidin as premedication. Note (for reading only): Etomidate (marketed as Amidate) is an imidazole derivatives synthesized in 1965. It is a short acting intravenous anaesthetic agent used for the induction of general anesthesia and for sedation for short procedures such as reduction of dislocated joints, tracheal intubation and cardioversion. Cardioversion (is medical procedure by which an abnormally fast heart rate or cardiac arrhythmia is converted to a normal rhythm, using electricity or drugs). 7- Eugenols They are three members: Estil, Propinal, and Propanidid (Epontol). The 1st and 2nd one was abandoned. The 3rd one was use to small ponies in castration. The duration of action is about 10 minutes. It is not used in large horses due to short duration of action. Note (for reading only):- The name is derived from the scientific name for clove, Eugenia aromaticum or Eugenia caryophyllata. Eugenol is responsible for the aroma of cloves. Page 17 of 29 8-Propofol Drug: Propofol (Rapinovet) Class: Alkyl phenol structure MOA: Sedative/hypnotic: CNS depression by enhancing GABA activity in the brain and decreasing cerebral metabolic rate DOA: <15 min ROA: (IV) Effect: Sedation to unconsciousness depending on dosage; muscle relaxation Adverse: Respiratory depression (apnea) especially if administered rapidly, myocardial depression, hypotension, Heinz body formation (oxidative injury) in cats when given repeatedly due to phenolic structure Approved: Dogs. Notes: It is used in all domestic animals; it is compatibles with wide range of drugs which used as pre-medication, inhalation anesthesia and neuromuscular blockers. Its cause rapid recovery more than Thiopental. In Dogs recovery occur after 20 minutes. In cats recovery occur after 30 minutes. Trade name and other names of Propofol: Rapinovet, Propoflo (veterinary preparations), and Diprivan (Human preparation). Propofol produces a short – acting (10 minutes) anesthesia, followed by a rapid and smooth recovery. Propofol may be used as an induction agent followed by inhalation with Halothane or Isoflurane. Page 18 of 29 Anesthetic agents (Injectable) (2) Less Rapidly Acting i.v. anesthetic Agents 1- Chloral hydrate Drug: Chloral hydrate: Class: Sedative-hypnotic MOA: CNS depression is due to active metabolites DOA: Dose dependent: <2 hr for sedative dosages ROA: (IV, PO) Effect: Sedation at low doses; general anesthetic at high doses; poor analgesic effects Adverse: Minimal at sedative dosages; anesthetic doses have high incidence of cardiopulmonary arrest Approved: None; once available in combination with pentobarbital and magnesium sulfate for use in large animals. Notes: It is good hypnotic a poor analgesia produce deep sleep lost for several hours. For that it is need high dose to produce anesthesia. It produces hypotension and respiratory depression because it depress vasomotor and respiratory center. Meanly used in equine. It can cross the placental barrier but it has low effect on fetus. It cause hypotension and Brady cardiac due to depression to vasomotor and myocardium and increase vagal tone. It is very irritant and its high concentration injected extravesscular cause tissue necrosis and sever irritation and phlebitis. It has prolonged recovery time. 3-Chloral hydrate + Magnesium sulfate: The combination of chloral hydrate magnesium sulfate in ration 1:1 Advantages: 1. Rapid and smooth induction. 2. Increase the depth of anesthesia. 3. Good muscle relaxation. 4. It reduces the toxicity of chloral hydrate and fewer irritants. 5. Less salivation. 2:1 3:1 Page 19 of 29 4-Chloral hydrate + Magnesium sulfate + Pentarbital: This combination called ( Equithesin ) It is prepared in the following ratio Chloral hydrate 28 gm Magnism sulfate 14 gm Pentobarbital 6.5 gm Dissolved in 1000 c.c of sterile distil water. Advantage: 1. Rapid and smooth induction without excitement. 2. Complete anesthesia (good analgesic) muscle relaxation. 3. Wide margin of safety. 4- Pentobarbital Sodium (Barbiturates) Drug: Pentobarbital (Nembutal; Beuthanasia-D): Class: Short-acting oxybarbiturate MOA: Sedative-hypnotic; CNS depression by action on barbiturate receptors DOA: Species and dose dependent; <1.5 hr ROA:(IV, PO) Effect: Sedation to unconsciousness Adverse: CNS/respiratory depression (apnea), myocardial depression, leukopenia, splenic engorgement, excitement (stage II) due to inadequate quantity or rate of dosing Approved: Dogs. Notes: The injection should be slow because it is rapidly depress the CNS (Cerebral cortex, hypothalamus, motor area). It depress respiratory center also. The recovery is slow and convulsion may occur. It is used in horses, cat, dogs, mice, rats, rabbits and guinea pig. In horses it is used to prolong the duration of chloral hydrate hypnosis. In dogs and cats it could be used alone as hypnotic or anesthetic but analgesics are needed. The action of pentobarbital is via nonselective depression of CNS. Rapid intravenous doses can be lethal. Pentobarbital has a narrow therapeutic index. When administrating i.v, inject first half of dose initially, then the remainder of calculated dose gradually until anesthetic effect is achieved. Page 20 of 29 5- Dissociative Agents Dissociative anesthesia defined as (Complete analgesia combined with only superficial sleep). In this state the animal may remain with their eye open with active laryngeal and pharyngeal reflexes. These agents are Cyclohexylamine derivatives, which are (Phenylcyclidine, Tiletamine and Ketamine). The term Dissociative anesthesia is used to describe an anesthetic state induced by drugs that interrupt ascending transmission from the unconscious to conscious part of the brain, rather than by generalized depression of all brain centers.. 1- Phencyclidine It is the first one used in veterinary medicine but it is no longer used. 2- Tiletamine Drug: Tiletamine; Zolazepam (Telazol) Class: Dissociative agent combined with benzodiazepine MOA: Tiletamine: depresses thalamoneocortical system; activates limbic system; analgesic effects are associated with opioid (agonist) and N-methyl-D-aspartate receptor (antagonist) interaction; zolazepam acts on benzodiazepine receptors DOA: Dose and species dependent; 20–80 min; ROA:(IM, IV) Effect: Catalepsy, superficial analgesia, amnesia, immobility, muscle relaxation Adverse: Increased secretions, muscle rigidity in some species, negative inotrope but central catecholamine release promotes increased BP and HR, increased ocular and intracranial pressure Approved: Cats, dogs Note: It is similar to Phenylcycldine but its potent twice, no long used due to lack of muscle relaxation and long recovery period with pain. 3- Tiletamine – Zolazepam combination I t is a combination of 1:1 of Tiletamine and Zolazepam respectively, it is available in all world but not in UK. It used in wild animal by dart gun in concentrated solution. In cat it causes Tachycardia. In dogs the tranquillizing effect of Zolazepam end before the effect of Tiletamine so recovery is difficult. Page 21 of 29 Notes: Trade and other names: Telazol and Zoletil. It is a combination of Tiletamine (Dissociative anesthetic agent similar in action to Ketamine) and Zolazepam (Benzodiazepam similar in action as diazepam). Tiletamine + Zolazepam produces a short duration (30 minutes) of anesthesia. In Cats, the effect of the Zolazepam will have a longer duration than Tiletamine. In Dogs, the Tiletamine will have a longer duration than Zolazepam. Therefore, anesthesia appears to be smoother in Cats than in Dogs. 4- Ketamine Hcl Drug: Ketamine (Ketaset; Ketalar; Vetalar) Class: Dissociative agent MOA: Depresses thalamoneocortical system; activates limbic system; analgesic effects are associated with opioid (agonist) and N-methyl-D-aspartate receptor (antagonist) interaction DOA: Dose and species dependent; 15–60 min; ROA:(IV, IM) Effect: Catalepsy, superficial analgesia, poor visual analgesia, amnesia, immobility Adverse: Muscle rigidity, seizures, increased secretions, negative inotropic agent but central catecholamine release causes increased ABP and HR, increased ocular and intracranial pressure Approved: Cats, primates Notes: The most important one of this group, It has shorter duration of action than other member of this group. it's effect on CNS appear after about 1 minute. With Ketamine many signs appear like muscle contraction, salivation leading to obstruction of the airways. But this side effect could be eliminated by using other compounds with Ketamine like Atropine, Diazepam, Midazolam, Xylazine, Detomidine, Medetomidine, Thiopental and even inhalation agents. It causes also mild respiratory depression, hypertension. Page 22 of 29 Other classification of injectable general anesthetics Barbiturates Nonbarbiturates Barbiturates Inject able general anesthetic drugs Are lipid soluble to varying degrees Lipid solubility increases from the long acting to the ultra short acting: The more lipids soluble the easier it is for the drug to cross the blood brain barrier Also recover from the effects of the barbiturate quicker. Recovery depends on a combination of redistribution and hepatic metabolism. As blood levels decline because of metabolism, small quantities of the drug will re-enter the bloodstream from muscle and fat occurs at such a low level and rate that this pathway does not significantly alter levels of consciousness Eliminated from the body by liver metabolism and excretion of the metabolites in the urine Classification of Barbiturate according to duration of action 1. Long-acting: Phenobarbital, Barbital. 2. Intermediate-acting: Amobarbital, Probarbilal. 3. Short- acting: Pentobarital, Cyclobarbital. 4. Ultra -short acting: Yhiopental, Thiamylal. Classification according to chemical structure: 1. Oxybarbiturates: a-methohexital b-pentobarbital 2. Methyllated oxybarbiturate: a-methohexital 3. Thiobarbiturates: Thiopental sodium hexobarbital Also classified by speed of onset of action 1. Long acting Phenobarbital 8-12 hours 2. Short-acting Pentobarbital 45- 90 minutes. 3. Ultra short acting 10-20 minutes. Drug: Methohexital (Brevital; Brevane; Brietal): Class: Ultrashort-acting oxybarbiturate MOA: Sedative-hypnotic; CNS depression by action on barbiturate receptors DOA: <15 min ROA: (IV) Effect: Sedation to unconsciousness (dose dependent) Page 23 of 29 Adverse: Respiratory depression (apnea), myocardial depression, excitement, muscle tremors, seizures during recovery Approved: None Drug: Phenobarbital: Class: Long-acting oxybarbiturate; routes include IV and PO MOA: Sedative/hypnotic; CNS depression by action on barbiturate receptors DOA: Dose dependent; 12–24 hr ROA: (IV, PO) Effect: Sedation to unconsciousness (dose dependent); used to control seizures: (16 mg/kg IV, 2–4 mg/kg PO BID (small animal); 2–10 mg/kg IV/PO every 8–12 hr (equine) Adverse: CNS/respiratory depression (apnea), myocardial depression, polyuria/polydipsia/ polyphagia Approved: None Drug: Thiopental (Pentothal; Intraval): Class: Ultrashort-acting thiobarbiturate MOA: Sedative/hypnotic; CNS depression by action on barbiturate receptors DOA: <15 min ROA: (IV) Effect: Sedation to unconsciousness (dose dependent), stage II delerium can occur with inadequate or perivascular dosages Adverse: Respiratory depression (apnea), myocardial depression, cardiac arrhythmias Approved: Dogs Nonbarbiturate Drug: Etomidate (Amidate; Hypnomidate*) Class: Imidazole MOA: Nonbarbiturate sedative-hypnotic DOA: <10 min; ROA:(IV) Effect: Rapid loss of consciousness of short duration, minimal cardiopulmonary depression Adverse: Pain on injection, myoclonus, vomiting (minimized with premedication); depression of adrenal function Approved: None Page 24 of 29 Or other classification of injectable anesthetic group Injectable anesthetic drugs 1. Barbiturate. 2. Chloral hydrate. 3. Choral hydrate + Magnesium sulfate. 4. Equithesine ( chloral hydrate + Magnesium sulfate + pentobarbitone) 5. Cataleptic or dissociative ex: ketamine. 6. Steroid anesthetic drugs ex: saffan Inhalation anesthetics Inhalation anesthetics are used in the form of volatile liquids or gases. These drugs are taken to the site of action through diffusion from pulmonary alveoli into the blood and thereafter to site of action i.e. central nervous system. Then the drugs are taken back by blood and thereafter they are exhaled. Primarily eliminated unchanged by the lungs Biotransformation to metabolites does occur to some degree, by microsomal enzymes . Factors that affect the brain concentrations of volatile anesthetic include Delivery of suitable concentrations of anesthetic agent. Vapor pressure Boiling point Anesthetic system Factors responsible for delivering the anesthetic from the lungs Alveolar partial pressure of the agent The inspired concentration of the agent Factors that affect the lung, brain and tissue uptake Solubility Tissue and arterial blood flow Anesthetic concentration Type of tissue and it’s blood Increased solubility leads to slow induction and recovery. Solubility is measured by the blood-gas partition coefficient, the solubility of an agent in the blood. Higher the number the greater the solubility Page 25 of 29 Larger amount of agent must be taken in before anesthesia result Potency of inhalation anesthetic agents often expressed as MAC (minimum alveolar concentration): The minimum concentration of an anesthetic that produces no response in 50% of the patients exposed to painful stimuli. The lower the MAC the more potent the anesthetic. A lower concentration is required to maintain a similar anesthetic depth Values vary among species and are affected by age, temperature, disease, other CNS depressant drugs and pregnancy 1- Ether ( Diethyl ether ) Colorless, highly volatile, inflammable and explosive and irritant liquid. Due to its irritant propriety it result in increase secretion of salivary and bronchial screacation. Ether can be administered by all methods. It has wide margin of safety. Good muscle relaxation. Induction period is long accompanied with excitement and slow recovery. It causes tachycardia and hypotension. It causes metabolic acidosis due to increase of lactic acid. 2-Chloroform: It was firstly used as anesthetic drug in animals by flourens in 1847. Clear sweat non inflammable non explosive and non irritating anesthetic liquid. It can be given by closed system. It is powerful anesthetic and a concentration of 0.035 percent of blood cause anesthesia and a concentration of 0.06 percent of blood is fatal. Induction is smooth with minimal salivation and marked relaxation of bronchial muscle. It has direct effect on myocardium which leads to cardiac dilation which reduces cardiac out put. It cause stimulation of vagal reflex in early stage which lead to slowing of heart and thus, cardiac failure. Palus is often increased due to struggling. Then the pulse becomes slow then normal. It causes depression of liver and kidney function. Death occurs due to cardiac failure and myocadium depression. Narrow margin of safety. Page 26 of 29 3-Halothane: Drug: Halothane (Fluothane) Class: Fluorinated hydrocarbon inhalation anesthetic MOA: Reversible depression of central nervous system DOA: Not applicable Effect: Unconsciousness, muscle relaxation Adverse: Dose-dependent cardiopulmonary depression, ventricular arrhythmias Approved: Dogs, cats, nonfood animals Notes: In dogs and cats, 2 to 4 per cent concentration in air or oxygen provokes full surgical anesthesia in 2 to 5 minutes with little excitement and no increase in salivation. Abdominal relaxation appears to be satisfactory. It has little analgesia. It is non nephrotoxic but it has hepatotoxoxic. It is noninflammable non explosive non irritating liquid anesthetic agent. It has characterstic pleasant odour. Halothane 2 more potent than chloroform and 4 times than ether it can be given by closed system. It have fast induction and fast and smooth recovery in about 10 to 20 minutes. It may cause respiratory depression. Inhalation of high concentration produces easily reversible apnea and progressive respiratory acidosis. IT also cause dose related cardiac depression resulting in hypotension. Bradycardia follows administration of halothane, due to vagal stimulation which is easily counteracted by atropine. It has very little effect on liver and kidney but repeated administration may cause liver necrosis. 4-Nitrous oxide: It is colorless non-irritating; non-inflammable and non-explosive gaseous anesthetic agent. Good margin of safety. Quick induction and recovery. Mild respiratory and cardiac depression Mixed with oxygen. Provides additional analgesia (varies by species) When used during anesthesia maintenance, it reduces the amount of other anesthetic agent require. Page 27 of 29 Disadvantages Cannot be used alone (MAC >100%) Danger of hypoxia if not used properly Reduces inspired oxygen levels to 33% Danger of hypoxia if used in patients with respiratory problems: Pneumonia, lung tumors, pulmonary edema, diaphragmatic hernia, or other conditions which compromise the patient’s ability to oxygenate Cannot be used with animals with gas occupying cavities (i.e. gastric dilation, intestinal obstruction, pneumothorax) Has an increased partial pressure and low solubility in blood. 5- Cyclopropane: Color less highly inflammable and explosive gas. The volatile anesthetics are liquid at room temperature and are relatively more soluble in blood and fat. The gaseous agent like cyclopropane and nitrous oxide are relatively less soluble in blood. 6- Desflurane Drug: Desflurane (Suprane) Class: Methyl ether inhalation agent MOA: Reversible depression of central nervous system DOA: Not applicable Effect: Unconsciousness, analgesia, muscle relaxation Adverse: Dose-dependent cardiopulmonary depression (slightly less than other inhalation agents at equivalent MAC concentrations) Approved: None 7- Enflurane Drug: Enflurane (Ethrane): an isomer of isoflurane Class: Methyl ether: inhalation agent MOA: Reversible depression of central nervous system DOA: Not applicable Effect: Unconsciousness, muscle relaxation Adverse: Dose-dependent cardiac and respiratory depression Approved: None Page 28 of 29 8- Isoflurane Drug: Isoflurane (Aerrane, Isoflo; Forane) Class: Methyl ether inhalation anesthetic MOA: Reversible depression of central nervous system DOA: Not applicable Effect: Unconsciousness, muscle relaxation Adverse: Dose-dependent cardiopulmonary depression (relatively less than halothane) Approved: Horses, dogs 9- Methoxyflurane Drug: Methoxyflurane (Metofane; Penthrane) Class: Methyl ether inhalation anesthetic MOA: Reversible depression of central nervous system DOA: Not applicable Effect: Unconsciousness, analgesia, muscle relaxation Adverse: Dose-dependent cardiopulmonary depression; prolonged recovery; renal toxicity due to metabolites Approved: Small and large animals, birds 10- Sevoflurane Drug: Sevoflurane (Ultrane) Class: Methyl ether inhalation agent MOA: Reversible depression of central nervous system DOA: Not applicable Effect: Unconsciousness, muscle relaxation Adverse: Dose-dependent cardiopulmonary depression (similar to isoflurane) Approved: None Page 29 of 29