Assignments Why do we add KCl when performing urine
Assignments
1.
Why do we add KCl when performing urine alkalinization using
NaHCO3?
1.
Indication: Drug Overdose with weak acid
1.
Phenobarbital or barbiturate overdose
2.
All Class I antidysrhythmic overdose
1.
Other sodium channel blockers
3.
Tricyclic Antidepressant Overdose
4.
Antihistamine Overdose
5.
Cocaine Overdose
6.
Salicylate s
7.
Chlorpropamide
8.
Sulfonamide s (some)
9.
Methotrexate
10.
Fluoride
11.
Diflunisal
2.
Mechanism
1.
Enhances urinary excretion of weak acids
2.
Traps weak acids in ionized state (ion trapping)
3.
Prevents reabsorption by renal tubules
3.
Preparation
1.
Sodium Bicarbonate 100 to 150 meq (2-3 ampules)
2.
Dissolve in 1 liter D5W with 20-40 meq KCl
1.
Works out to 0.1 to 0.15 meq/ml
2.
Do not exceed 0.5 meq/ml concentration
4.
Dosing
1.
Use 0.1 to 0.15 meq/l NaHCO3 in D5W with KCl as above
2.
Administer at 2 to 4 times maintenance IV rate
1.
Adult rate will be 200 to 400 ml/hour
2.
Adults would receive 20-30 to 40-60 meq/hour
3.
Do not exceed 1 meq/kg/hour
4.
Typically given over 2-3 hours
3.
Titrate to alkalizization
1.
Keep Urine pH at 7.5 to 8.0
2.
Keep serum pH normal (>7.40)
3.
Keep urine output at 2-5 ml/kg/hour
4.
Monitoring
1.
Follow Serum Potassium closely
2.
Correct Hypokalemia if it occurs
Potassium replacement becomes of utmost importance in this setting because potassium is usually also lost in urine and hypokalemia promotes bicarbonate ion retention and prevents bicarbonate excretion, thus interfering with alkalinization of the urine.
1
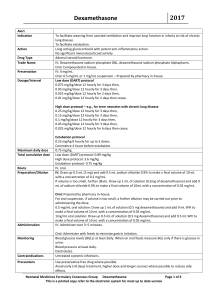
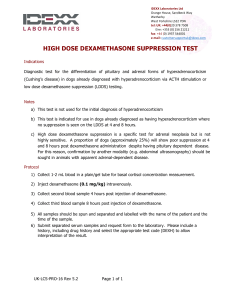
2. Convert methylprednisolone dose to dexamethasone in hyper CVAD regimen.
We can either use one of the following tables or use an internet website such as http://www.globalrph.com/corticocalc.htm
Glucocorticoid Approximate
Equivalent dose (mg)
Half-life (Biologic) hours
Cortisone
Hydrocortisone
Methylprednisolone
Prednisolone
Prednisone
Triamcinolone
Short-Acting
25
20
Intermediate-Acting
4
5
5
4
Long-Acting
0.6 - 0.75
0.75
8-12
8-12
18-36
18-36
18-36
18-36
Betamethasone
Dexamethasone
36-54
36-54
Glucocorticoid Comparison*
*Approximate Equivalent may vary with disease state
Agent
Betamethasome 0.6-0.75 IM,IV,PO 20-30
Dexamethasone 0.75 IM,IV,PO 5-30
Hydrocortisone 20
Methylprednisolo ne
4
Prednisolone 5
Prednisone
Equivale nt Dose
(approx. mg)
5
Route of
Administrati on
IM,IV,PO
PO
PO
Relative
Antiinflammato ry
Potency
Relative
Mineralocortico id
Potency
Biologi c
Half-
Life
(hours)
IM,IV,PO 1
5
4
4
0
0
2
0
1
1
36-54
36-54
8-12
18-36
18-36
18-36
2
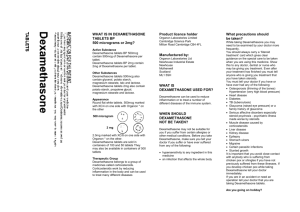
Dexamethasone to Methylprednisolone Conversion
Dr Bleck's Neurosurgery Service
Dexamethasone Methylprednisolone
Dose in mg Dose in mg
0.5
2
1 4
6
7
8
9
2
3
4
5
9
13
18
22
27
31
36
40
10
11
12
13
14
15
16
17
18
44
49
53
58
62
67
71
76
80
19
20
84
89
So the 50 mg methylprednisolone dose is equivalent to 9.38 mg.
3. Role of methotrexate in hyper CVAD
Methotrexate’s therapeutic and toxic effects are a result of its ability to limit
DNA and RNA synthesis by inhibiting dihydrofolate reductase and thymidylate synthetase. It enters cells through an active transport system used by folate and binds to and inhibits the enzyme. This enzyme maintains reduced folate by recycling dihydrofolic acid which has been produced during thymidylate synthesis (see diagram). Dihydrofolate reductase reduces folic acid to tetrahydrofolate, an essential co-factor in the synthesis of purine nucleotides.
Reduced folates are also required by thymidylate synthetase to provide methyl donors for the formation of thymidylate, essential for DNA synthesis.
3
Thus the effects of methotrexate poisoning are most apparent in more rapidly dividing cells such as gastrointestinal tract and bone marrow. Effects are also often observed on the liver as higher concentrations of methotrexate are provided to the liver through the portal circulation as the drug is absorbed.
Acute renal failure can result from drug precipitation in the renal tubule, particularly in patients who are inadequately hydrated or not alkalinised.
4. Role of Ca-leucoverin in hyper CVAD
The antidote folinic acid supplies tetrahydrofolate and needs to be given for as long as the methotrexate is present in the cell (48-72 hours).
Administration of reduced folate in the form of folinic acid (leucovorin) allows for continued purine synthesis in the methotrexate-toxic patient and is used in high-dose MTX therapy to limit the toxic effects.
5. Role of dexamethasone in hyper CVAD
Systemic Dexamethasone:
Dexamethasone is an immunosuppressant.
It induces apopotosis in ALL.
In combination with intrathecal cytrabine, dexamethasone decreases the severity of arachnoiditis (cytarabine side effect).
Dexamethasone eye drops:
Prophylactic use of Dexamethasone 0.1% or Pred Forte
Ophthalmic solution 1-2 drops q4h while awake for 7 days
(during high dose Cytarabine) to prevent conjunctivitis.
Prepared By: Rania Abdelghaffar Elwatidy
4
Pharm.D. student.
5
![[Drug Name] Generic Name: Compound Anisodine Hydrobromide](http://s3.studylib.net/store/data/007043112_1-d16b4f2e5f96c851498d41cb4852b648-300x300.png)