The sleeve gastrectomy: A alternative restrictive operation
advertisement
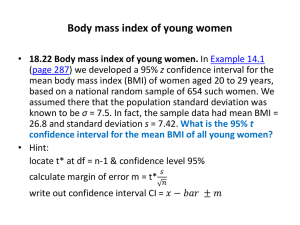
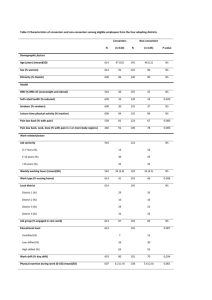
Laparoscopic Sleeve Gastrectomy. A multi-purpose bariatric operation Aniceto Baltasar MD 1, Carlos Serra MD 2, Nieves Pérez MD 2, Rafael Bou MD 2, Marcelo Bengochea MD 2, Lirios Ferri 2 (*) Chief of the Surgical Service (**) Surgical Staff Clínica San Jorge & Alcoy Hospital. Alcoy. Spain A. Baltasar, MD c/ Cid 61 03803 Alcoy Alicante. Spain abaltasar@seco.org baltasar_ani@gva.es Short-title: “LapSG” Phone (+34) 96-553.74.39 FAX (+34) 96-533.04.00 2 Abstract: Background: We present our experience with the use of the LSG (laparoscopic sleeve gastrectomy), a restrictive procedure, in different settings. Methods: Thirty–one patients had the LSG for: I) Seven patient with very high BMI as a first stage of the DS (Duodenal Switch); II) Seven morbidly obese patients with severe medical conditions; III) Sixteen obese patients with low BMI (35 to 43); and IV) One patient converted from a lap-band. Results: One patient with BMI-74 died, 3.2% mortality. The %EBMIL (percentage BMI loss) of I patients is 63.1% from 4 to 27 months. The %EBMIL of the cirrhotic II patients is 76.0% (69 to 100). The %EBMIL of III patients is 68.5% (from 58.3 to 123%) at 3 to 27 months. The %EBMIL of the IV patient is 13% since she has lost previously almost all her EBMI. Conclusion: LSG may become the ideal operation for staging high > 55% BMI patients, treat morbidly obese patients with severe medical conditions, an excellent alternative to adjustable bands in low BMI patients or conversion of the lap-band patients. Key words: Sleeve gastrectomy. Laparoscopy. Obesity surgery. 3 Introduction: SG (sleeve gastrectomy) is the restrictive part of the more extensive mixed restrictive and mal-absorptive operation, the BPD/DS (Bilio-pancreatic diversion-Duodenal Switch). Hess 1, 2 performed the first DS (Duodenal Switch) operation in March 1988 (in a lady with a BMI of 60 and 17 years later remains with a BMI of 29) and Marceau Rabkin 4 3 published the first paper. in September 1999 did the first hand-assisted LDS (Laparoscopic DS) and Gagner et al 5,6 the first totally laparoscopic LDS in October of the same year. Gagner et al 7 published the first report of the LSG (Laparoscopic SG) as the first stage of the LDS in the super-obese patients. Matherial & Methods: Thirty-one obese patients have been treated with the LSG (selected from a total of 791 patients who had the DS) from Jan 2003 until June 2005, for different conditions: I) Super-obese (SO). Seven patients had, BMI ranging from 61 to 74 (mean 65), the LSG as a first stage of the full LapDS. One patient had a previous Lap fundoplication and has the Nissen dismounted at the time of the LSG. II) Severe medical illness and BMI > 40. Seven patients had a severe medical condition that made not advisable the full DS. Four had unexpected cirrhosis of the liver (discovered at surgery and later confirmed by biopsy), one BMI-51 patient had Crohn´s disease and a 4 previous right hemicolectomy, one BMI-60 patient had a severe pulmonary poisoning condition (Ardystil syndrome) and one BMI-61 patient is a HIV+ without AIDS III) Low BMI. Sixteen patients had BMI from 35 to 43 with at least one co-morbidity, and IV) Conversion from a Lap-band. A patient with normal BMI had severe unbearable symptoms that required conversion. Technique: General anesthesia is given. The drawing of the operation is shown in Fig 1. An Endopath gasless technique is used to enter the abdomen by a #12 mm. trocar on the supraumbilical lateral border of the right rectus. Four more #5 mm trocars were placed 1) subxifoid, 2) right costal margin, 3) left costal margin, 4) lateral border of the left rectus and a #10 mm. trocar for the camera in the midline (Fig.2). Bupivacaine is used as local anesthetic at all the trocar entrances. Division of the greater curvature of the stomach is done with the HS (Harmonic scalpel) from the left crus of the diaphragm to distal to the pylorus. At the level of the spleen’s lower pole, the peritoneal sheets are farther apart and the tissue in between is thicker and harbours tortuous vessels (the short gastric) which must be coagulated separately by using small bites of the HS. Two sequential USSC (Tyco Healthcare) 45 mm. blue linear staplers are used starting 2 cm from the pylorus, and close to a 32 F naso-gastric tube, up to the incisura angularis. Then the Tyco staplers 6 cm long are used (3 to 4) up to reach the angle of His. A gastric tube (sleeve), less than 60 cc in volume, remains and the rest of the 80% of the stomach is excised. The staple line is 5 inverted by placing a sero-serosa continuous suture of PDS from the angle of His to mid-suture line and a second one to the end. Diluted half-strength Methidine blue dye, 50 cc, is used to test for leaks. The duodenum is clamped and by irrigating the sleeve the dye usually overflows back to the patient’s mouth. The stomach is removed by enlarging the peritoneal and fascial opening of the #12 mm. trocar and pulling from the antrum without the need for a protecting bag. The enlarged fascial opening is closed with a single figure-of-eight Maxon #1 suture and a drain is left, through one #5 mm. port, for 2 days along the pouch suture-line. Mean average operating time is 49 minutes (40 to 60) for the <BMI-60 patients. On POD1 the patient is given a test of oral Methidine blue dye and a gastrografin x-ray study to rule out leaks and discharged on the POD2. Small sipping, strictly liquids, oral feedings are used for 2 weeks and then they resume normal intake. Post-Op Dietary: It is imperative that SG patients adhere to a strict postoperative diet. After 4-6 weeks, patients graduate to a 600-800 calorie/ day solid diet. Once goal weight is achieved, usually 1-2 years after surgery, most patients can consume about 1000-1200 calories per day. Results: For WL (Weight Loss) measures we have used the formula %EWL (percentage of Excess Weight Loss) = [(Operative Weight – Follow-up Weight) / Operative Excess Weight] x 100 and the %EBMIL (percentage of Excess BMI Loss) = %EBMIL = 100 – [(Follow-up BMI – 25 / Beginning BMI -25) x 100] 6 I. SO Patients. One male patient, BMI-74, with several co- morbidities died due to complications related to the working port hemorrhage. The rest of patients had a mean 56.1 %EWL (46-66%) and a 63.1 %EBMIL (57 to 72) from 4 to 27 months. Only one BMI-62 patient had, one year later, a second stage of the DS at BMI-49 and, now six months later her BMI is 33. II. Severe medical illness and BMI > 40. The patient with Crohn’s disease has at 16 months a %EWL 0f 59.5 and %EIMCL = 66.0. The patient with the pulmonary condition has at 14 months %EWL = 72.5 and her %EIMCP = 76.0. The HVI+ patient at 4 months has %EWL=33.6 and %EIMCL=36.8. The cirrhotic patients have 71 %EWL (64-90) and 76 %EBMIL (69-100) without worsening their liver function. III. Low BMI patients. One patient ruptured (while coughing) the sutured working trocar access and developed an intra-abdominal bleeding that required re-laparoscopic aspiration of 400 cc. hemoperitoneum and suture of the abdominal opening again. The patients have a %EWL at 3-27 months of 62.3 %EWL (42-100) and 68.5 %EBMIL (58-123%). IV. Conversion from a Lap-band. The only patient had a BMI of 28 and her BMI is 27 one year later, %EBMI 13%, and her QOL was improve significantly. Two patients suffered serious complication of trocar related intrabdominal bleeding, one of then died (3.2% mortality) and the second required laparoscopic exploration. No episodes of deep venous thrombosis, pulmonary emboli, pneumonia, acute respiratory distress syndrome, splenectomy, gastric leak and fistula or small bowel obstruction occurred. 7 All these patients have done clinically extremely well at the intermediate period. None of them had any pernicious side-effect. Early satiety has been their only symptom. B12 and folic acid have been normal. None of them have anemia. Two patients with hypertension and diabetes are off medications. Discussion: Hess 1, 2 after 10 years follow up with a %EWL of 75% in 94% of his patients considers that the DS is the most effective operation and should become the gold standard in bariatric surgery and we, as Rabkin 8, fully agree with him. The idea of the SG appeared after the LDS became a reality. The LSG has been proposed as a first step in the staging of the LapDS 9,10,11,12 by different authors with encouraging results for high >55 BMI patients. Staging helps decrease mortality mostly in the association of Super-SuperObesity and male gender were the mortality is elevated in patients undergoing the DS procedure 13, but even LSG resulted in mortality in our male super- super-obese with a minor trocar site hemorrhage. To protect the stomach suture line from bleeding and leaks other materials have been added (buttressed absorbable polymer membranes, Goretex, bovine pericardial strips, etc.) with mixed results 14, 15, 16. We use a continue absorvable suture sero-serosa, inverted over the staples, which controls bleeding in almost all cases, decrease leaks 1, does no increase the cost of the procedure and takes about 10 minutes of suturing. LSG generates weight loss by restricting the amount of food that can be eaten without any malabsorption. The stomach pouch in the LSG is usually made smaller than the pouch that DS patients because without an intestinal bypass 8 weight regain may happens as in the gastroplasty procedures done in the 1970's and 80's. Basically, the SG is an improvement over prior gastroplasty procedures, which today are rarely done due to problems related to the placement of staples, silastic rings and mesh around the stomach pouch and reservoir-gastric fistulas. No foreign body is used as it is on the vertical banded gastroplasty and adjustable bands. We do not think the M&M (Magenstrasse and Mill) operation described by Johnston 17 is the same as a SG type of operation. On the M&M, The Magenstrasse or “street of the stomach” is a long tube fashioned from the lesser curvature, which conveys food from the esophagus to the antral Mill. Normal antral grinding of solid foods and antro-pyloro-duodenal regulation of gastric emptying and secretion are preserved. There is no resection of the stomach and the antrum (Mill) is intact and the rest of the stomach is in the food pathway, so the Ghrelin production is not reduced and food can enter the rest of the stomach before it empties into the duodenum. It is also simple gastroplasty with leads to a 60% EWL but more difficult to carry out by laparoscopy than the LSG. What Johnston reports is the importance of the size of the NG tube stent while doing the division of the stomach since the 32 F proved to be the ideal size for better weight loss. Consensus about the gastric sleeve volume is still to be made. Gagner et al 6 uses a 60F gastric bougie and the gastric volume is 150-200 cc. and this could be a reason why some patients may require further surgery due to dilation of the gastric pouch 18. LSG patients at the Mt Sinai Hospital (NYC) have approximately 60 percent of the stomach removed and patients get a %EWL of 30 to 50% of their excess 9 body weight over a 6 - 12 month period. Lee 10 removes about 85% of the stomach in 68 patients. Schauer 11 uses a 48F bougie in his 77 patients. The distance from the pylorus where the division of the stomach starts is not standard. Gagner 7 recommends 10 cm, Lee 10 only 6 cm. We start the division of the antrum 2 cm from the pylorus in the LSG and 3 to 4 cm on the LDS, because the “restrictive only” SG should be more restrictive still than the full DS, since it is the only mechanism used to loose weight. Our stomach remnant is reduced in volume to less than 50 cc but functions normally and most foods can be consumed, albeit in small amounts, and gastric emptying is normal 19, 20. SG eliminates the portion of the stomach that produces the hormones that stimulates hunger (Ghrelin). No dumping syndrome exists in the SG because the pylorus is preserved and it minimizes the incidence of peptic ulcers. By avoiding the intestinal bypass, the risk of intestinal obstruction (blockage), anemia, osteoporosis, protein malnutrition and vitamin deficiencies are eliminated. Very large, > 65 BMI patients can still be operated on. LSG is also an appealing option for people with other medical conditions such as existing anemia, those who need to take anti-inflammatory medications, Crohn's disease and numerous other conditions that make them the DS too high risky for intestinal bypass procedures. For patients with low BMI (BMI 35-43 kg/m2), early and limited results appear promising as a single stage procedure in our cases but follow up is still too short. If the long-term results are maintained, this procedure may become the ideal operation for those patients instead of the lap-band since no foreign body is used, no adjustments are needed, and excess stomach volume is removed, not left in place. This possibly eliminates most Ghrelin hormone production and helps to reduce the sensation of hunger that obese patients 10 have. The patient also has a second opportunity to have the second stage part of the DS if the WL results are not significant without the need to go back to the upper abdomen to remove a problematic band. It seems to us at this time that LSG is the best alternative to the lap-band for low BMI patients; those were the lap-band has the best indications. The LSG is also a good indication for the patients were the lap-band has given complications such us poor weight lost, perforation and removal or poor QOL, such as in our only patient who after removal of the band and LSG has improved her QOL. LSG disadvantages are: This procedure does involve stomach division and stapling and therefore leaks and other complications related to stapling may occur. Potential for inadequate weight loss or weight regain. While this is true for all weight loss procedures, it is theoretically more likely with procedures that do not have an intestinal bypass. Higher BMI patients will need to have a second stage procedure later to help loose the rest of the excess weight if their BMI remains above 45. Two stages may ultimately be safer and more effective than one operation for high BMI patients. This is an active point of discussion for bariatric surgeons. Soft calories such as ice cream, milk shakes, etc. can be absorbed and may slow weight loss. Because the stomach is removed, it is not reversible, but it can be converted to almost any other weight loss procedure, mainly laparoscopic gastric bypass or DS. Long-term WL results are at this time unknown but on the low BMI patients if 70% of them will have <50 %EWL this will eventually be for them the ideal operation. 11 References: 1. Hess DS, Hess DW. Biliopancreatic diversion with duodenal switch. Obes Surg 1998; 8:267-82 2. Hess DS,Hess DW,OakleyRS. The biliopancreatic diversion with the duodenal switch: results beyond 10 years. Obes Surg 2005;15:408416(9). 3. Marceau P, Biron S, Bourque RA et al. Bilio-pancreatic diversion with a new type of gastrectomy. Obes Surg 1993:3:29-35. 4. Rabkin RA, Rabkin JM, Metcalf B, Lazo M, Rossi M, Lee BL: Laparoscopic technique for performing duodenal switch with gastric reduction. Obes Surg 2003, 13: 263-268. 5. Ren CJ, Patterson E, Gagner M. Early results of laparoscopic biliopancreatic diversion with duodenal switch: a case series of 40 consecutive patients. Obes Surg 2000; 10:514-23. 6. Gagner M.: Laparoscopic Malabsorptive procedures. Laparoscopic biliopancreatic diversion with duodenal switch. Technique and preliminary results. Presentation at SAGES 2001. Laparoscopic bariatric surgery. 7. Regan JP, Inabnet WB, Gagner M: Early experience with two-stage laparoscopic Roux-en-Y gastric bypass as an alternative in the supersuper obese patient. Obes Surg 2003; 13: 861-4. 8. Rabkin R.: Concept. The duodenal switch as an increasing and highly effective operation for morbid obesity. Obes Surg 2004; 14: 861-865. 9. Almogy G, Crookes PF, Anthone G.: Longitudinal gastrectomy as a treatment for the high-risk super-obese patient. Obes Surg 2004; 14; 492-497. 10. Lee C, Feng J, Cirangle P, Jossart G.: Laparoscopic vertical sleeve gastrectomy. A novel bariatric procedure - Superior to stablished operations? Presentation at the American College of Surgeons, New Orleans, October 2004: www.facs.org/education/gs2004/gs33lee.pdf 11. Schauer P: Two-stage weight loss surgery for high-risk, morbidly obese patients reduces surgical risk. Presentation at SAGES. Denver, 2004. 12. Milone L, Strong V, Gagner M: Laparoscopic sleeve gastrectomy is superior to endoscopic intragastric balloon as a first stage procedure for the super-obese patients (BMI >50). Obes Surg 2005; 15:612-617. 13. Fazylov R, Savel R, Horovitz J, Pagala M, Coppa G, Nocastro J, Lazzaro R, Macura J: Association of super-super-obesity and male gender with elevated mortality in patients undergoing the duodenal switch procedure. Obes Surg 2005; 15:618-623. 14. Consten E C.J.; Gagner M; Pomp A;. Inabnet WB: Decreased bleeding after laparoscopic sleeve gastrectomy with or without duodenal switch for morbid obesity using a stapled buttressed absorbable polymer membrane. Obes Surg 2004 14:1360-1366. 15. Consten E.C.J, Dakin G.F, Gagner M. Intraluminal migration of bovine pericardial strips used to reinforce the gastric staple-line in laparoscopic bariatric surgery. Obes Surg, 2004;14: 549-554. 12 16. Shikora SA, Kim JJ, Tarnoff ME: Reinforcing gastric staple-lines with bovine pericardial strips may decrease the likelihood of gastric leak after laparoscopic roux-en-y gastric bypass. Obes Surg, 2003, 13, 37-44(8). 17. Johnston DJ, Dachtler J, Sue-Ling H, King R, Martin I.: The Magenstrasse and Mill operation for morbid obesity. Obes Surg2003, 13:10-16. 18. Gagner M.; Rogula T.: Laparoscopic reoperative sleeve gastrectomy for poor weight loss after biliopancreatic diversion with duodenal switch. Obes Surg 2003, 13: 649-654. 19. Baltasar A. Gastric emptying of solids after the duodenal switch. IFSO. Prague. Abstracts. Obes Surg 1996; 16:302. 20. Martinez Castro R., Baltasar A., Vidal V, Sánchez Cuenca J, Lledó JL: Gastric emptying study in patients with morbid obesity who undergo duodenal switch. Rev Esp Enf Digest 1997; 89:413-4.