Module 05 FL Baker Act Involuntary Treatment
advertisement
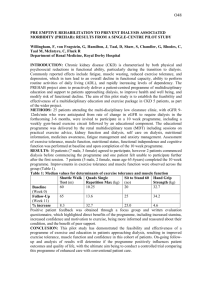
Module 05 The patient was a 35-year old Caucasian female admitted to this facility due to noncompliance with her dialysis medication and depression with suicidal gesture, having taken an overdose of Keppra and Zonegran. Upon medical stabilization the patient was admitted to behavioral medicine unit. The patient suffered from chronic renal failure and was routinely on dialysis for which she had been repeatedly non-compliant – described as nth stage. She also reported frequent seizures. Competence was a central issue as the patient states: “I’ve had enough and don’t want to live anymore”. The patient consistently expressed her wish to be discharged home – an apartment where she was living with her spouse. The medical physician notes the following on her history and physical: “The patient was alert, oriented to person, place, time and circumstance. She denied the use of alcohol or any illicit drugs. Her mood was depressed, her thought process hopeless, helpless, negativistic. She is of average intelligence and has general fund of knowledge. No acute cognitive deficits were noted. Memory recall for recent and remote events remained intact. She admitted to recent suicidal ideation following a gesture of overdose and continued to verbalize ongoing suicidal ideations. Her insight and judgment skills were fair, impulse control poor.” The patient was admitted under the Florida Mental Health Act’s BA-52 involuntary placement criteria. This allows a psychiatric facility to hold an individual up to seventy-two hours based on the opinion of a qualified professional and treating psychiatrist. After the 72 hours is up, the facility must file a BA-32 involuntary placement petition in order to keep the patient longer. BA-32 requires a 2nd opinion by a psychiatrist and a court hearing within a reasonable period of time – usually no more than two weeks. The admitting psychiatrist determined that the patient lacked capacity to make medical decisions and was therefore incompetent to refuse dialysis. She wrote an order upon admission to forcibly administer dialysis. As director of the program, I asked that a second opinion be done, in order to fulfill the BA-32 requirement and to concur with the capacity assessment. I asked that once the 2nd opinion was completed that an emergency hearing be called to have a judge determine competence and appoint a health care surrogate. I asked that all of this occur prior to forcing dialysis. The medical physicians had assured me that dialysis could wait at least 7 days. Two psychiatrists examined the patient and determined she was competent to make medical decisions and expressed concern that her wish to refuse medical care was being ignored. Two other psychiatrists refused to examine the patient including the acting medical director. The 72-hour involuntary placement period ran without the required 2nd opinion being completed. As the program director it was my decision, some would say my responsibility to discharge the patient immediately. Instead I met with the patient and explained the dilemma. She asked to be discharged immediately and reiterated her intent to end her life because of her physical illness. I chose instead to discharge and readmit the patient under another BA-52 signed by the treating psychiatrist. While technically allowable under the law, this practice rarely occurs and always draws scrutiny from the court. Prior to taking the action, I solicited an opinion from our risk management department and an informal opinion from the hearing master who would eventually hear the case. We then asked for an emergency hearing which occurred within 24-hours. The court determined that the patient was incompetent to make medical decisions and appointed a guardian, a friend of the patient, to make all further medical decisions. The patient, faced with no option but to accept treatment, agreed to dialysis and was eventually discharged to a nursing home after a 2-week stay.