Chapter 21: Answers to Case Study 1
advertisement

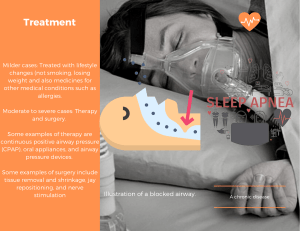
Answers to Case Study, Chapter 21, Assessment of Respiratory Function Objective: 4 Which assessment parameters are appropriate to determine the characteristics and severity of the symptoms that the patient is exhibiting? The nurse needs to assess the patient’s lungs anteriorly and posteriorly to assess for adequacy of ventilation. Pulse oximetry is also needed to assess for oxygenation. The nurse needs to assess the patient’s vital signs to determine hemodynamic stability. The nurse needs to further investigate the patient’s breathing pattern, which is suggestive of sleep apnea. The patient’s symptoms of lethargy and somnolence are suggestive of retaining carbon dioxide (CO2). Which nursing interventions should the nurse institute? Which intervention must be provided immediately? The nurse needs to place the head of the bed up immediately to a level where the patient’s lungs may fully expand to help the patient to breathe. The nurse will need to perform an assessment to determine the underlying causes for the patient’s sudden change in maintaining airway and breathing. The nurse will need to contact the surgeon with the assessment findings. The nurse should call for the rapid response team to help assess the patient’s situation and to provide emergent standing orders to maintain airway and breathing. The nurse anticipates that the patient will need oxygen, and naloxone (Narcan) to reverse the respiratory depression caused by the narcotic, and further investigation and follow-up treatment of sleep apnea. Explain the possible reasons for the patient’s sudden decline in the respiratory status. A patient who is obese has limited chest expansion because of the large abdomen interfering with proper expansion, leading to hypoventilation and atelectasis, and the retention of CO2. The retention of CO2 leads to the body’s compensatory mechanism of breathing faster, which is reflected in the baseline vital signs when the patient’s respiratory rate was 26 breaths per minute. The patient is lying supine and chest expansion is limited by obesity leading to shallow breaths and the development of atelectasis. The narcotic provides sedation, which further decreases the patient’s tidal volume. The narcotic also depresses the patient’s respiratory center, which leads to a decreased respiratory rate. The patient’s sedation leads to sleep, and the patient may have sleep apnea as reflected by the observation of having a period of apnea followed by a snorting gasp. As the patient’s CO2 level increases, the body starts to increase the respiratory rate and the airway in sleep apnea may be blocked by excessive soft tissue so the patient snorts to open the airway and then gasps for air and begins breathing. The patient’s neck circumference is 21 inches, which supports excessive soft tissue related to obesity that may occlude the airway during sleep. The patient’s body mass index (BMI) of 36.2 also supports the risk for sleep apnea.