CEREBROVASCULAR DISEASE
advertisement
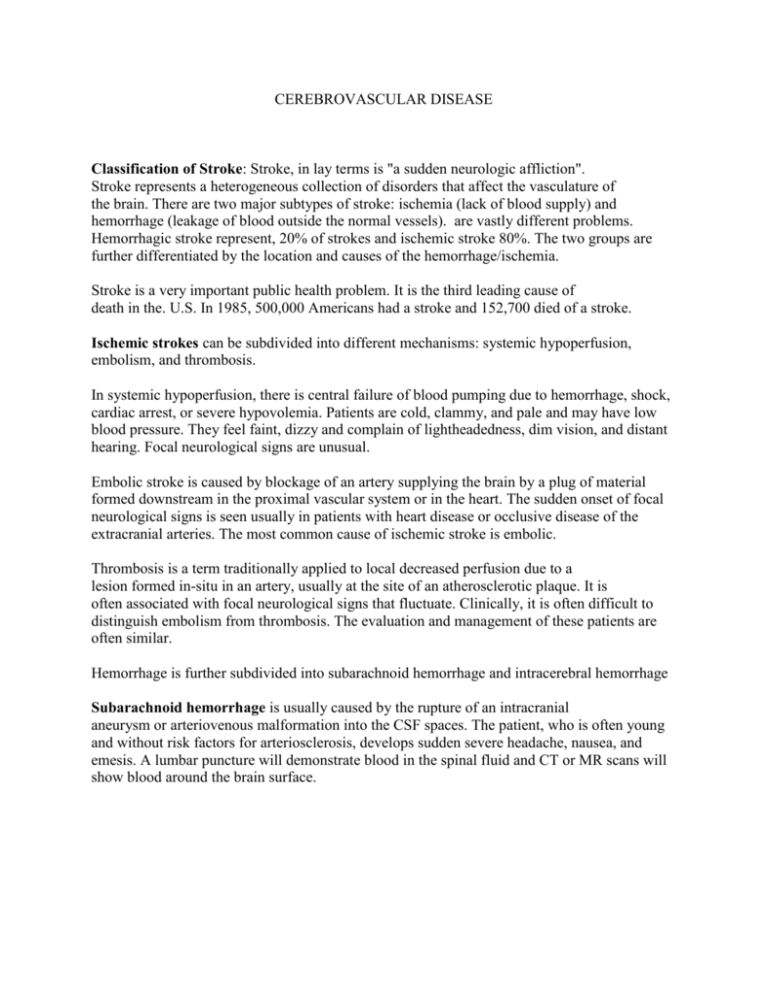
CEREBROVASCULAR DISEASE Classification of Stroke: Stroke, in lay terms is "a sudden neurologic affliction". Stroke represents a heterogeneous collection of disorders that affect the vasculature of the brain. There are two major subtypes of stroke: ischemia (lack of blood supply) and hemorrhage (leakage of blood outside the normal vessels). are vastly different problems. Hemorrhagic stroke represent, 20% of strokes and ischemic stroke 80%. The two groups are further differentiated by the location and causes of the hemorrhage/ischemia. Stroke is a very important public health problem. It is the third leading cause of death in the. U.S. In 1985, 500,000 Americans had a stroke and 152,700 died of a stroke. Ischemic strokes can be subdivided into different mechanisms: systemic hypoperfusion, embolism, and thrombosis. In systemic hypoperfusion, there is central failure of blood pumping due to hemorrhage, shock, cardiac arrest, or severe hypovolemia. Patients are cold, clammy, and pale and may have low blood pressure. They feel faint, dizzy and complain of lightheadedness, dim vision, and distant hearing. Focal neurological signs are unusual. Embolic stroke is caused by blockage of an artery supplying the brain by a plug of material formed downstream in the proximal vascular system or in the heart. The sudden onset of focal neurological signs is seen usually in patients with heart disease or occlusive disease of the extracranial arteries. The most common cause of ischemic stroke is embolic. Thrombosis is a term traditionally applied to local decreased perfusion due to a lesion formed in-situ in an artery, usually at the site of an atherosclerotic plaque. It is often associated with focal neurological signs that fluctuate. Clinically, it is often difficult to distinguish embolism from thrombosis. The evaluation and management of these patients are often similar. Hemorrhage is further subdivided into subarachnoid hemorrhage and intracerebral hemorrhage Subarachnoid hemorrhage is usually caused by the rupture of an intracranial aneurysm or arteriovenous malformation into the CSF spaces. The patient, who is often young and without risk factors for arteriosclerosis, develops sudden severe headache, nausea, and emesis. A lumbar puncture will demonstrate blood in the spinal fluid and CT or MR scans will show blood around the brain surface. Intracerebral hemorrhage occurs most often from rupture of small arteries damaged by hypertension. It can be caused by rupture of an aneurysm or AVM. The patient develops focal neurological signs, such as hemiparesis or aphasia, depending on the location of the clot, that progressively worsen in minutes or hours. Headache, vomiting, and reduced level of consciousness occur. Imaging studies show hematoma within the brain. ISCHEMIC STROKE Atherosclerosis, the primary cause of vascular occlusion, is most prevalent at the bifurcations of blood vessels. The origin of the internal carotid artery, just distal to the bifurcation of the common carotid artery, is a common place for atherosclerosis to occur. Transient Ischemic Attacks (TIA): An episode of focal brain ischemia of loss than 24 hours is called a transient ischemic attack or TIA. Diagnosis of TIA: Clinical concept based on the sudden development and clearing of neurological symptoms presumably resulting from a vascular occlusive process. Non-focal symptoms occurring in isolation are not TIAs. These include isolated vertigo, wooziness, lightheadedness, and syncope. Focal ischemia is not the only cause of sudden focal neurological deficits. Simple partial (focal) seizures, migraine syndromes, tumors and chronic subdural hematoma may mimic TIAs. Focal seizures may not be associated with a change in level of consciousness. Focal migraine may not have associated headache. The key to the diagnosis of focal seizures and migraines, rather than TIA, is the marching evolution of the neurological symptoms. With seizures, the march is rapid, lasting seconds. With migraines, the march lasts several minutes. Other clues to migraine include visual scintillations and normal results of vascular imaging studies. On the other hand, focal ischemia occasionally produces marching, clonic, or positive symptoms suggestive of seizures or migraines. Focal clonic limb shaking has been associated with severe carotid stenosis or occlusion (hemodynamic insufficiency), and patients with vertebro-basilar system atherosclerosis may have visual symptoms due to occipital lobe ischemia. Vascular distribution of TIAs Carotid vs. vertebro-basilar: Unilateral symptoms suggest carotid ischemia, while bilateral symptoms suggest vertebro-basilar ischemia, especially when combined with symptoms like vertigo, dysarthria, or dysphagia. Recurrent, stereotyped hemi-motor or hermi-sensory symptoms suggest carotid occlusive disease. Alternating neurological symptoms suggest vertebro basilar disease, cardiac embolism, or diffuse vascular disease. Carotid artery ischemia Amaurosis fugax: Transient monocular blindness. The patients classically describe descending or ascending "shade" in vision. Less than half of patients have 75% or greater stenosis of the internal carotid artery. Cortical deficits: Contralateral hemiparesis and hemisensory loss, dysphasia with dominant cerebral hemisphere involvement, dysarthria with non-dominant cerebral hemisphere involvement, and contralateral homonymous hemianopsia may be seen in varying combinations in carotid artery territory ischemia. Vertebro-basilar ischemia: Homonymous field defect, diplopia, vertigo, dysarthria, gait ataxia, brief loss of consciousness, unilateral or bilateral hemiparesis or hemisensory loss. Bilateral visual loss is posterior circulation ischemia. Description of visual loss moving medially or laterally is suspicious for hemianopsia arid therefore posterior circulation ischemia. Mechanism of TIAs: Embolus: atherosclerotic plaque, lipohyaliosis of arterioles. Hemodynamic basis: postural, exercise induced, after introduction of antihypertensive medications. Epidemiology and natural history of TIAs: A prevalence of 116 per 100,000 was seen in the Framingham, MA study and a prevalence of 139 per 100,000 was found in the 1970 age-adjusted Rochester, MN study. Less than halt of brain infarctions are preceded by warning TIAs. The period of highest risk for stroke is in the first several months to the first year after TIA occurrence. There is an 8% risk of stroke in the first month, 5% per year risk for the next three years and a 3% risk per year thereafter. The overall 5 year risk of stroke following the onset of TIAs is 33%, but the numbers may be diluted by including younger patients, non-focal symptoms, etc., in these series. The long-term stroke rate for carotid or vertero-basliar TIAs, is not significantly different. The frequency, duration, and number of TIAs are not consistently related to stroke risk, but this is not proven. "Crescendo" TIAs are thought to have greater stroke risk, but this is not proven. A single TIA also carries significant risk. The annual risk of MI is 5% in TIA patients, which is equivalent to that of patients with angina pectoris or triple vessel coronary disease. There is a high prevalence of asymptomatic coronary artery disease in TIA patients. Carotid bruit is a better marker for coronary artery disease than for stroke. It is important to incorporate an evaluation of the coronary circulation the workup of patients with cerebrovascular symptoms. Cerebral Infarction: There is risk of further infarction after the initial occurrence of infarction. A 7.9% risk of recurrent infarction within 30 days was seen in patients with an atherosclerotic cerebral infarct entered into the Stroke Data Bank Study. Transient monocular blindness, TIA, minor stroke and major stroke form a hierarchy of increasingly severe symptoms that mirror an increasing risk for stroke. The available evidence indicates that stroke risk correlates with the degree of carotid stenosis. Lacunar Infarction: Lacunes are small infarcts resulting from the thrombosis of small perforating blood vessels. These infarcts are associated with hypertensive vascular disease and may produce certain well-defined neurological syndromes. Pure motor hemiparesis. Pure motor weakness without other associated neurological deficits are often associated with small lacunes in the pons or internal capsule. Pure sensory stroke. Sensory loss without other associated neurological deficits is often due to a small lesion within the thalamus. Leg paresis and ataxia. This unusual combination of weakness and difficulty with coordination can be seen with lesions in the pons or internal capsule. Clumsy hand dysarthria syndrome. This combination of neurological findings is seen with lesions in the upper third of the pons. Prevention of Stroke: Risk factors for cerebral atherosclerotic TIA and stroke include: age, hypertension, diabetes, family history, cigarette smoking, lipid disorders. Cardiac pathologies, such as dilated cardiomyopathies, certain valvular disease, and atrial fibrillation may lead to intracardiac thrombus formation and cerebral embolism. Risk factor modification, smoking cessation, anti-hypertensive agents, and lipid lowering agents all decrease the risk for stroke as well as for myocardial infarction. The widespread treatment of hypertension is the most important reason for the decline in the stroke rate in the U.S. over the past 40 years. No studies have shown a benefit of anti-platelet therapy in the general population and for asymptomatic cerebrovascular lesions. Evaluation of patients Medical history and examination: The history should focus on atherosclerotic risk factors, cardiac disease, and vascular disease in patients under age of 45, non-atherosclerotic causes of cerebral ischemia are more prevalent. Question patients re: use of oral contraceptives and the use of cocaine. A history of spontaneous abortions and deep vein thrombosis may suggest a hypercoagulable state, such as the anticardiolipin syndrome. Neurovascular exam: Blood pressure in both arms, lying and standing. This is particularly important in patients suspected of having vertebro-basilar ischemia to detect a subclavian steal syndrome. Cardiac auscultation and rhythm check Auscultation of head and neck for bruits: Absence of bruit does not rule out severe carotid stenosis. Conversely, only 50% of cervical bruits are associated with significant underlying carotid stenosis. Palpation of neck, facial, and radial pulses: Unless the carotid pulse is absent, palpation of the carotid pulse is not much help in establishing a diagnosis. Funduscopic exam for platelet or fibrin, cholesterol or calcific emboli. Laboratory evaluation is often normal in stroke patients. Diabetes mellitus and lipid disorders need to be ruled out. In younger patients, tests for vasculitis and hypercoagulable states need to be performed. Cardiac studies give the best results in patients under age 45. In patients with unexplained events, or in patients with cardiac symptoms and signs, transesophageal echocardiography is superior to transthoracic echocardiography in potential sources of cerebral emboli. Transthoracic echocardiography is less expensive and more convenient and is usually used for initial screening. Holter monitoring may detect occult cardiac rhythm disturbances associated with cerebral ischemia. Imaging studies Brain imaging studies: A CTor MR scan should be obtained to rule out tumor, vascular malformations, and other nonocclusive causes of neurological symptoms, intracranial hemorrhage, and to demonstrate infarction. An MR scan is more likely to show acute changes in patients with cerebral infarction, compared to a CT scan. A CT scan may begin to demonstrate low-density areas as early as 12 hours after the occurrence of an infarct. The lowdensity of infarction seen on CT scan may take several days to become maximal. The lowdensity of cerebral infarction does not stop at the border between gray and white matter, as is seen with cerebral edema. Contrast enhancement of the infarct may be seen after several days and may persist for weeks. In one study of patients with TIA or amaurosis fugax, 42% of CT scans had focal changes, half of which correlated with the patient's symptoms. MR scans showed abnormalities in 84% of patients, with 80% of abnormalities ipsilateral to the presenting symptoms. An MR scan is more expensive and loss readily available. A CT scan is adequate to rule out intracranial hemorrhage, which is the major concern in initial management. Ultrasound studies: Duplex carotid ultrasonography has supplanted a large battery of noninvasive tests for the detection of extracranial carotid artery occlusive disease. In experienced hands duplex scanning for lesions of the carotid artery have shown an overall 91% to 99% sensitivity and 84% to 90% specificity. Ultrasound studies may not be able to distinguish severe stenosis from complete occlusion of the internal carotid artery. It is most accurate for detecting stenosis exceeding 70%, Duplex scanning is also useful for studying carotid plaque morphology. The extra-cranial vertebral artery can be studied with ultrasound technique. If the patient is a reasonable surgical risk for carotid endarterectomy, there is little indication for ultrasound studies. The patient should have cerebral angiography carried out. Conventional cerebral angiography is still the "gold standard". It permits assessment of the intracranial circulation and collateral pathways. It defines the extent of extra cranial occlusive disease. The indications for angiography in vertebra-basilar disease are more controversial. MR angiography continues to be refined. It has proven to be a good screening procedure for extra cranial carotid occlusive disease with accuracy comparable to duplex carotid ultrasonography. Some studies are not technically adequate and its accuracy in determining the degree of stenosis is not as good as conventional angiography. It sometimes has difficulty distinguishing severe stenosis from complete occlusion of the carotid artery. Medical treatment of ischemic stroke Cardiac disorders: Anticoagulation with warfarin decreases the incidence of stroke in patients with recent MI, prosthetic valves, and non-rheumatic atrial fibrillation. Four randomized, controlled clinical trials have compared warfarin or aspirin with placebo for primary prevention of stroke in patients with atrial fibrillation. Control patients had stroke event rates 4.5% per year (3%-7%) compared to 1.7% per year (0.2%-3.4%) in patients treated with warfarin. The annual rates of bleeding in patients; on warfarin was less than 2%. The proper dose of warfarin is unclear, but significant risk reduction is achieved with the prothrombin time at 1.3-1.5 times control. Large artery atherosclerotic occlusive disease Warfarin anticoagulation: There is no indication for warfarin in carotid artery disease. There is some evidence for warfarin anticoagulation in vertebra-basilar artery disease; but- this is not entirely clear. Antiplatelet therapy: Aspirin (ASA) therapy is standard for virtually all patients since publication of the American and Canadian aspirin trials in the late 1970s. A metaanalysis of 25 completed studies involving 29,000 patients with angina, MI, TIA, or stroke indicates that ASA reduces the risk of nonfatal stroke, MI or vascular death by 25%. The risk of nonfatal stroke in TIA patients is reduced by about 22%. Aspirin is thought to work by inhibiting the cyclooxygenase pathway of the arachidonic acid cascade. The ineffectiveness of ASA in women may be due to the small number of women included in published studies. The European Stroke Prevention Study showed that the combination of ASA and dipyridamole was effective in men as well as women. The optimal dose of ASA is problematic. Low and high doses of A SA were equivalent in the UK-TIA ASA trial. Dipyridamole and sulfinpyrazone are no better than ASA alone. Ticlopidine is a newer antiplatelet agent. The mechanism of action of this agent is unclear. It does not inhibit cyclooxygenase. It may irreversibly affect platelet membrane function. It is moderately superior to ASA in stroke prevention. In the Ticlopidine Aspirin Stroke Study (TASS), the overall risk reduction for nonfatal or fatal stroke by ticlopidine was 21% and was observed in both men and women. Compared with placebo, ticlopidine reduces the rate of recurrence in patients who have had a major stroke by 33% in one year. Side effects of ticlopidine are severe neutropenia (0.8%}. This usually occurs in the first 90 days of therapy and is reversible. The CBC must be monitored every two weeks for three months. It also causes diarrhea and GI upset. Ticlopidine is currently recommended for stroke prevention in patients with symptomatic atherothrombotic cerebrovascular disease who cannot tolerate ASA or who have events while on ASA. It is a very expensive drug. Clopidogrel (Plavix) is a new antiplatelet drug. It has not been shown to be any more effective than ASA in the secondary prevention of stroke. No studies have shown a benefit for antiplatelet therapy as a primary prevention for stroke in the general population or in asymptomatic patients with vascular risk factors or carotid artery stenosis. Surgical Treatment of Ischemic Stroke Carotid endarterectomy involves opening the carotid artery at the carotid bifurcation and dissecting out and removing the atheromatous plaque. Three major randomized studies of symptomatic patients comparing medical vs. surgical therapy were recently completed. All patients were on ASA and hypertension was treated. Some medical patients were on warfarin. The patients had amaurosis, hemispheric TIAs, or mild strokes. North American Symptomatic Carotid Endarterectomy Trial (N.Eng.J.Med. 325:445453,1991, N Eng J Med 339:1415-1425, 1998). MRC European Carotid Surgery Trial (Lancet 337:1235-1243. 1991). VA Cooperative Study (JAMA 266:3289-3294, 1991) Surgery significantly benefits patients under 80 years of age with appropriate angiographically defined carotid stenosis of 70%-99%. There is a small but significant benefit of surgery in symptomatic patients with 50% to 69% stenosis of the carotid artery. The benefit is greatest in males, with only a marginal benefit of surgery in females. The benefit of carotid endarterectomy in this group of patients is much less than that seen in patients with carotid stenosis of 70% or more. No benefit for carotid stenosis of 50% or less. Extracranial-intracranial arterial bypass for atherosclerotic lesions not accessible by conventional extra cranial surgical techniques. No benefit of surgery vs. medical therapy was found in a large randomized study. Interventional neuroradiology treatment: Balloon angioplasty and stenting are being performed for carotid artery stenosis. Distal emboli following angioplasty is a major risk, but has not been a significant problem. Good initial results for carotid artery stenosis have been reported. Good results have been reported for balloon angioplasty of vertebral artery origin stenosis. Some good results have been reported for balloon angioplasty of intracranial stenosis, but a significant number of severe arterial complications have occurred with this procedure when performed in intracranial vessels. Intra-arterial thrombolytic agents have been used in some centers to treat acutely thrombosed cerebral arteries. Asymptomatic carotid artery stenosis: Prevalence of neck bruits and carotid artery stenosis. Neck bruits in Framingham study: 3.5% incidence <54 years of age, 7.0% incidence 65-79 years of age. Ultrasound screening for carotid stenosis (45-84 years of aye): 2.4% incidence in men, 30% incidence in men 75-84 years of age. The risk of perioperative stroke are future stroke are two separate problems in patients with asymptomatic carotid artery stenosis. The risk of perioperative stroke is known and is very low. The risk of future stroke is less clear. In a large long-term followup study using carotid ultrasound to investigate patients with asymptomatic cerebral artery disease, patients with less than 75% stenosis of the internal carotid artery had an annual ipsilateral ischemic stroke rate of 1.3%. With greater than 75% stenosis of the internal carotid artery, the annual ipsilateral stroke rate was 2.5%. Carotid endarterectomy: A large randomized trial of surgical vs medical treatment of asymptomatic carotid stenosis of 60% or greater showed a significant benefit of carotid endarterectomy, with a reduction of an annual ipsilateral stroke risk of 2.2% to 1.0%. The benefit occurred mostly in men with only a marginal benefit for surgery in women. HEMORRHAGIC CEREBROVASCULAR DISEASE The two most frequent types of hemorrhagic strokes are subarachnoid hemorrhage (SAH) and spontaneous intracerebral hemorrhage. Each of those occurs with an incidence of approximately 10-14 per 100,000 population per year and represents an important cause of neurological morbidity and mortality. Hemorrhagic strokes may either result in devastating neurological deficits and death, or relatively minor symptoms. Subarachnoid hemorrhage Epidemiology: Depending on the population studied, trauma is probably the most common cause of subarachnoid hemorrhage. In general, and for the purposes of this syllabus, subarachnoid hemorrhage of non-traumatic (spontaneous) etiology will be considered. Ruptured intracranial aneurysms account for approximately 80% of subarachnoid hemorrhages. Arteriovenous malformations lying adjacent to the subarachnoid space account for approximately 15 %. A variety of other less frequent causes, including tumor and vasculitis, cause the remaining cases of subarachnoid hemorrhage. As many as 20% of patients who sustain a subarachnoid hemorrhage, after a complete neuroradiological evaluation, will not have a definable cause for their hemorrhage, Intracranial aneurysms are present in approximately 2% of the population. The risk of rupture has been quantified by the ISUIA study. The 5 year rupture rate for aneurysms in the anterior circulation aneurysms by size are: 0% for <7mm, 2.6% for 7-12 mm, 14.5% for 13-24 mm, and 40% for >2.5 cm. For posterior circulation aneurysm, the risks are higher: 2.6% for <7mm, 14.5% for 7-12 mm, 18% for 13-24 mm, and 50% for .2.5 cm. Certain families appear to have a higher prevalence of intracranial aneurysm. There are welldocumented cases where multiple family members have had subarachnoid hemorrhages. Most data suggest that families with more than one close relative with an intracranial aneurysm or subarachnoid hemorrhage have a prevalence of intracranial aneurysms of about 7% to 8%, or approximately three times the risk for the general population. About one-third of patients will have a subarachnoid hemorrhage that occurs during sleep. A significant number of other patients will be participating in strenuous activity, such as exercise or sexual intercourse, at the time of their hemorrhage. An important entity in the differential diagnosis is benign orgasmic cephalalgia which is a condition of uncertain cause characterized by recurrent headaches that occur during orgasm. Subarachnoid hemorrhage is not infrequently associated with extension of the hemorrhage into the cerebral hemisphere or into the ventricles. It rarely involves the subdural space. A number of risk factors have been identified for subarachnoid hemorrhage. These include hypertension, cigarette smoking in women, alcohol consumption and possibly oral contraceptives. Subarachnoid hemorrhage can occur during pregnancy and parturition, but there is controversy about whether the risk of intracranial hemorrhage is increased in either of these conditions. The relationship between the occurrence of systemic arterial hypertension and intracranial hemorrhage is also uncertain. Hypertension does appear to be related to the development of intracranial aneurysms, but is not clearly related to their rupture once they have developed. Some patients with defects of Type 3 collagen and certain connective tissue diseases also appear to be at an increased risk for the development of cerebral aneurysms. Patients with polycystic kidney disease and coarctation of the aorta are also at increased risk, although the precise cause of this, whether it relates to hypertension, is not entirely clear. About 28,000 patients will sustain a subarachnoid hemorrhage each year. A significant number of patients (between 10%- 20/%), will die either with the initial hemorrhage or during the first few days. The overall early mortality is approximately 5O% and about half of the survivors of subarachnoid hemorrhage have a significant neurological disability. Clinical Aspects: Subarachnoid hemorrhage is characterized by the abrupt onset of a severe headache. Patients frequently describe this headache as being the worst headache of their life. Other patients will describe a feeling like "being hit in the back of the neck with a 2 by 4". Patients will frequently describe neck pain, especially in the suboccipital region, as the initial manifestation of their hemorrhage. A generalized headache may later develop. Neck stiffness and symptoms of focal crania nerve deficits may also occur. About 30%-50% of patients with subarachnoid hemorrhage will sustain a loss of consciousness. Warning hemorrhage may occur in up to 50% of patients with subarachnoid hemorrhage. This is usually a headache of less severe character or occasionally a mild neurological deficit such as diplopia. It is important that these warning symptoms be recognized and evaluated, although they are often very subtle and may be difficult to distinguish from other transient neurological symptoms. Physical Examination: Patients may have an altered level of consciousness and they are described by the variety of classification schemes for subarachnoid hemorrhage. The commonly used scheme is that described by Hunt and Hess as indicated in the following table. Cerebrovascular Disease Grade 1 2 3 Clinical Description Asymptomatic or very mild headache or meningismus Cranial nerve palsy, moderate to severe headache or severe nuchal rigidity Mild to moderate focal neurological deficit, lethargy or confusion 4 Stupor (Localize) 5 Coma (Posture) One grade is added for serious medical illnesses such as coronary artery disease, diabetes mellitus or chronic obstructive pulmonary disease. Nuchal rigidity usually develops after the patient’s initial symptoms. When the thigh is flexed and the knee is extended, Kernig's sign may be elicited with pain in the posterior aspect of the upper legs. Brudzinski's sign is elicited when the patient's neck is flexed and they involuntarily flex their hips. A third nerve palsy may be present especially with aneurysms arising at the posterior communicating artery, superior cerebellar, or basilar artery. Subhyaloid hemorrhages may occur on fundus examination and are characterized as a bright red accumulation of blood near the optic disc. Diagnosis of Subarachnoid Hemorrhage: The history and physical exam findings should suggest the diagnosis of SAH. Laboratory and imaging studies are used to confirm the diagnosis. The first confirmatory diagnostic study that should be applied in a patient with a suspected subarachnoid hemorrhage is a non-contrast CT scan. Greater than 95% of patients with a subarachnoid hemorrhage, scanned within 48 hours of the onset of their symptoms, will have detectable blood in the subarachnoid cisterns or cerebral ventricles. The CT scan may also show the presence of a significant increase in ventricular size, the presence of a hematoma and may the useful in predicting the location or the aneurysms If the CT scan is positive, it is usually not necessary to further confirm the diagnosis by doing a lumbar puncture, In patients who are suspected of having a subarachnoid hemorrhage and in whom the CT scan is negative, a CSF examination should be performed. Bloody fluid will indicate that a subarachnoid hemorrhage has occurred. If the fluid is bloody because o a traumatic tap, the cell count in sequential tubes will decrease. Xanthochromia of the fluid will often be present and should be looked for in a specimen of the fluid after centrifugation. MR scans are generally not useful in making the diagnosis of a subarachnoid hemorrhage from an intracranial aneurysm. It may be helpful if other entities cause the hemorrhage, such as an arteriovenous malformation. Usually, however, MR scanning is not necessary. Once the diagnosis of subarachnoid hemorrhage has been confirmed by a CT scan or lumbar puncture, a cerebral angiogram should be performed. In 80% to 85% of patients, an aneurysm or other cause for the hemorrhage will be identified. The most common sites for the occurrence of an aneurysm in a patient with a subarachnoid hemorrhage are the internal carotid artery at its junction with the posterior communicating artery, the anterior communicating artery, the bifurcation of the middle cerebral artery in the Sylvian fissure, and the basilar artery apex. Less frequent sites include the ophthalmic artery, the termination of the carotid artery, and arteries distributed along the vertebral and lower trunk of the basilar artery. Twenty per cent of patients will have multiple intracranial aneurysms and it is important that complete cerebral angiography be accomplished so that all potential sites of aneurysms have been identified. Management of Subarachnoid Hemorrhage: The main objectives in the management of aneurysmal subarachnoid hemorrhage are to prevent rebleeding, treat vasospasm and hydrocephalus, and avoid the medical complications of subarachnoid hemorrhage. Re-hemorrhage is avoided by securing the aneurysm or resecting the arteriovenous malformation which has caused the hemorrhage. Surgical and Endovascular Management: To prevent rebleeding, cerebral aneurysms should be either clipped or coiled. Clipping the aneurysm is a time-tested standard therapy which requires a craniotomy and microsurgical.dissection of the arteries and the application of a small aneurysm clip. Recently, techniques have been developed to treat cerebral aneurysms by endovascular techniques. The most commonly applied technique is the use of a detachable platinum coil. In this technique, a cerebral angiograrn is performed and a small platinum wire is placed into the aneurysm to form a coil in the shape of a basket, which leads to the eventual thrombosis and obliteration of the aneurysm in successful cases. The coil is then detached from the delivery mechanism. Aneurysms with small necks relative to the overall dimensions of the fundus of the aneurysm, are the lesion most optimally treated by endovascular means. In most large medical centers, a decision regarding the appropriate type of treatment is made by a combined team neurosurgeons and endovascular therapists. The surgical management of subarachnoid hemorrhage is usually initiated within the first two days after the hemorrhage. If the diagnosis has been delayed for some reason and the patient is within the 10-14 day post subarachnoid hemorrhage period, surgery is usually delayed so that the patient will not be at increased risk for the development of postoperative vasospasm. Early surgery in the treatment of subarachnoid hemorrhage is usually a superior approach because it markedly reduces the risk of rebleeding which occurs frequently in the first few days following subarachnoid hemorrhage. It also may allow vasospasm to be more effectively treated by having the aneurysm secured prior to manipulations which may elevate the transmural pressure of the aneurysm. The frequent sites for the occurrence of cerebral aneurysms can he reached via a pterional craniotomy. In this approach, an incision is made behind the hairline and a flap of bone is removed, centered on the pterion in the anterior temporal and inferior frontal region. This allows access to the basal subarachnoid cisterns by a path that parallels the greater sphenoid wing. The anterior communicating artery, posterior communicating artery, middle cerebral artery and basilar apex may all be accessed through this approach. A more posterior subtemporal approach is sometimes used for aneurysms of the basilar apex. Surgery on intracranial aneurysms is greatly facilitated by the use of the operating microscope. These sophisticated devices allow magnification and..brilliant illumination of the subarachnoid space. Precisely manufactured spring-loaded clips can then be manipulated across the neck of an aneurysm, separating the aneurysm from the circulation while maintaining normal blood flow through the parent vessel and important perforators in the region of the fundus of the aneurysm. The surgical morbidity and mortality for the management of vertebrobasilar aneurysms, and large and giant aneurysms (aneurysms having a maximum dimension exceeding 25mn) is generally higher than that for smaller anterior circulation aneurysms. Peri-operative Management: Patients who have sustained a subarachnoid hemorrhage are vulnerable to a number of complications. The most frequent and serious complications are: rebleeding of the aneurysm, cerebral vasospasm with the development of delayed cerebral ischemia, hydrocephalus, fluid and electrolyte problems. Cerebral Vasospasm Incidence and pathophysiology: Cerebral vasospasrn is an incompletely understood complication of subarachnoid hemorrhage in which progressive arterial narrowing occurs-usually 4-10 days after the initial hemorrhage. If this progressive arterial narrowing is severe enough, cerebral ischemia will develop in the distribution of the affected arteries. The pathogenesis and etiology of cerebral vasospasm are not completely understood. Most evidence points to oxy-hemoglobin accumulating in the subarachnoid space on the adventitial surface of the vessel as the main causative agent. A loss of endothelial dependent relaxation, inflammation and free oxygen radicals all appeal to play a role in the ultimate pathological consequences of cerebral vasospasm which is a critical narrowing of cerebral arteries with resultant cerebral ischemia. Clinical characteristics of cerebral vasospasm: About one-third of patients with aneurysmal subarachrroid hemorrhage will develop some evidence of symptomatic cerebral vasospasm. Many patients will have radiographic evidence of some vasospasm without developing clinical symptoms. The onset of spasm is usually 6-8 days after subarachnoid hemorrhage, but may occur somewhat earlier and later than this. Cerebral vasospasm appears to be much more likely in patients with thick subarachnoid clot. A grading system proposed by Fisher describes patients at increased risk. There also appears to be a relationship between the initial Hunt and Hess grade and the incidence of clinical vasospasm. Patients with poor neurological function are at higher risk for the development of vasospasm. The initial symptoms and signs of cerebral vasospasm after a subarachnoid hemorrhage include increasing lethargy, fever and the development of focal neurological deficits such as hemiparesis or dysphasia. The recognition of subtle neurological deficits in this setting is important for the early escalation of treatment for cerebral vasospasm. Treatment of cerebral vasospasm Calcium channel blockers: Cerebral arteries are extremely dependent upon the mobilization of calcium from extracellular stores to induce vasoconstriction. For this reason, calcium channel blockers have proven to be effective in the management and prophylaxis of cerebral vasospasm. Nimodipine has been shown in a randomized perspective double blind clinical trial to improve outcome after aneurysmal subarachnoid hemorrhage by lessening the severity of delayed cerebral ischemia. It must be given PO or by an NG tube at a dose of 60mg every four hours. It can be associated with hypotension or cardiac dysrhythmias and therefore must be administered in lesser doses in patients who develop one of these complications. Hypervolemic therapy for cerebral vasospasm: Patients with symptomatic cerebral vasospasm are extremely sensitive to reduced blood volume. This observation led to the development of hypervolomic therapy for cerebral vasospasm. Patients with symptomatic cerebral vasospasm are monitored with an arterial line, a Foley catheter and usually a Swan-Ganz catheter. Cardiac output and pulmonary capillary wedge pressure are monitored and continuously recorded. The CVP is elevated to approximately 10-12mm of mercury and tine pulmonary capillary wedge between 14 -20mm of mercury. The systolic blood pressure may be allowed to rise to levels up to 240mm of mercury in patients with clipped aneurysms and mean blood pressure levels less than 150mm of mercury. Patients with unclipped aneurysms should have their systolic blood pressure maintained below 150mm of mercury. Volume expansion to induce hypervolemia is usually accomplished by the administration of colloids including plasma, albumin or hetastarch. Packed red cells or whole blood is given, depending upon the hematocrit which should be maintained between 30-33%. Pressors, such as Dopamine or phenylephrine, may be administered. Patients will often develop a brisk diuresis in this situation and high volumes of crystalloid may need to be given. Occasionally, vasopressin can be administered to diminish the volume of such a diuresis as long as the serum sodium is carefully monitored. Additional treatments for cerebral vasospasm: Recently it has become possible to treat cerebral vasospasm by an endovascular route. Balloon catheters are placed within the artery and are used to gently dilate the constricted vessels. Papavorine many be administered interarterially and has been reported to be effective in the treatment of cerebral vasospasm. These treatments are used for patients who do not respond to hypervolemic therapy and calcium antagonists. Hydrocephalus: Hydrocephalus develops after subarachnoid hemorrhage in about 15% of patients. Patients with intraventricular hemorrhage and severe subarachnoid hemorrhage are more likely to develop hydrocephalus. Hydrocephalus is an important differential consideration in evaluating the new onset of lethargy in a patient after subarachnoid hemorrhage and therefore a CT scan may often have to be performed to detect this condition. Hydrocephalus, in the setting of. subarachnoid hemorrhage, is usually managed initially with a placement of an intraventricular catheter via a frontal twist drill craniotomy if the hydrocephalus does not resolve after a week to 10 days of external ventricular drainage, then a ventriculo-peritoneal shunt may need to be placed. Hyponatremia and other fluid and electrolyte problems: Hyponatremia occurs frequently in patients with subarachnoid hemorrhage. The etiology of the hyponatremia in these patients is complex, but is not the simple development of inappropriate secretion of ADH (SIADH). There appears to be a significant component of hypovolemia and total body sodium depletion which occurs in these patients. A variety of naturetic factors have been implicated in the pathogenesis of this syndrome, but it is incompletely understood. It is crucial that patients with hyponatremia not be treated with fluid restriction. This will only worsen the vasospasm that will likely develop in this circumstance. Patients should either be managed with isotonic or occasionally hypertonic saline with careful attention to central filling pressures. The management of hyponatremia in the setting of subarachnoid hemorrhage can be extremely difficult. Vascular malformations which cause intracranial hemorrhage: There are three important types of vascular malformations: arteriovenous malformations (AVMs), cavernous angiomas or cavernous malformations, and venous angiomas. Arteriovenous malformations: Arteriovenous malformations are congenital lesions lesions characterized by direct shunting of arterial blood into the cerebral venous system. These lesions may vary in size from a few millimeters up to 10-20 centimeters and may occupy an entire hemisphere. They have a tendency to enlarge after their formation in the fetus and the progressive enlargement of the arterial and venous components may constitute a mass lesion, cause seizures or alter cerebral hemodynamics in a way that may precipitate cerebral ischemia. Clinical characteristics of arteriovenous malformations: Most often become apparent during the 2nd, 3rd or 4th decade of life. Arteriovenous malformations may present as an intracerebral or subarachnoid hemorrhage, seizures, headaches or other neurological deficits. Hemorrhage occurs in 30-50% arteriorvenous malformations and seizures occur with a similar frequency. Natural history of arteriovenous malformations: Arteriovenous malformations, which present with an initial hemorrhage, rehemorrhage at a rate of approximately 4% per year. AVMs that present with other manifestations such as a seizure or headaches appear to bleed at a rate of 1% to 2% per year. Younger patients are more likely to develop epilepsy as a complication of an existing arteriovenous malformation. Evaluation of arteriovenous malformations: CT scans will often demonstrate an enhancing mass of abnormal vessels. MR scans are extremely useful in the evaluation of cerebral arteriovenous malformations since it allows assessment of the contiguity of functional brain structures around the arteriovenous malformation. Assessment of the feeding vessels and venous components of an arteriovenous malformation can only be done by cerebral angiography. Arteriovenous malformations are graded based on their size, the eloquence of adjacent brain and the pattern of venous drainage. The outcome of treatment on the Spetzler grading system is directly related to the grade of AVM. Treatment of arteriovenous malformations: The decision to treat an arteriovenous malformation must be based on an assessment of the location and vascular characteristics of the lesion as well as the proximity of the lesion to eloquent cortex. In general, arteriovenous malformations of moderate size which are not in eloquent areas of brain should be removed in younger patients since they are likely to cause a hemorrhage at some point in the patient’s life. The decision to treat other lesions must be individualized. There are several methods of treating arteriovenous malformations: microsurgical removal, endovascular treatment with embolization therapy and stereotactic radiosurgery. Microsurgical removal involves the performance of a craniotomy usually after embolization therapy has been performed. The arterial feeders of the malformation are isolated and the lesion is progressively separated from the surrounding brain. Eventually the lesion is isolated on its venous pedicle and it is removed. Intraoperative angiography can often be helpful in the management of these lesions. Stereotactic radiosurgery is another useful treatment for arteriovenous malformations. Lesions with diameters of less than 3-4cm are suitable for stereotactic radiosurgery. The radiation administered in this form of treatment causes a progressive obliteration of the arterial and venous components of the lesion, making it not visible on angiography, in approximately 85% of patients at two years after treatment. A disadvantage of stereotactic radiosurgery is that there is a latency period between the administration of the treatment and the effect of obliteration of the lesion, which may be up to two years. About 15-20% of lesions so treated will not be completely obliterated. Cavernous malformations are lesions composed primarily of large venous channels without a clear-cut arterial component. These lesions are difficult to visualize on angiography and are not characterized by the very high blood flows seen in arteriovenous malformations. These lesions are readily identified by their typical appearance on the MR scan consisting of a heterogeneous lesion with bright and dark signal areas on the T1 and T2 weighted images consistent with blood products in various degrees of resolution. They constitute about 5-10% of vascular malformations and may occur at any site in the brain. They usually present with seizures, but may sometimes cause an intracerebral hemorrhage. Accessible cavernous malformations which cause symptoms should be surgically excised. Asymptomatic lesions or lesions at inaccessible sites are often not treated surgically unless they cause recurrent and repeated hemorrhages. Venous malformations seldom need any type of treatment. They are often identified incidentally. Intracerebral Hemorrhage Epidemiology: Intracerebral hemorrhage occurs with a frequency of about 8-14 cases per 100,000 per year. The incidence of intracerebral hemorrhage is highest in the 6th, 7th and 8th decades of life and occurs somewhat later than the peak incidence for aneurysmal subarachnoid hemorrhage. The cause of many intracerebral hemorrhages is unknown. Hypertension has been implicated as a cause, but there is not a clear-cut relationship between the presence of systemic arterial hypertension and the development of an intracerebral hemorrhage. Brain tumors, vascular malformations and cocaine abuse are all associated with the development of intracerebral hemorrhage. The most common sites for intracerebral hemorrhage are in the basal ganglia and occur in the putamen, globus pallidus or thalamus. Pontine and cerebellar hemorrhages each account for 10% of all intracerebral hemorrhages, respectively. Hemorrhages occurring in the frontal, temporal or occipital lobes are described as lobar hemorrhages. Clinical characteristics of intracerebral hemorrhage: Lesions occurring in the putamen most often cause a contralateral hemiparesis or hemiplegia and may progress to produce coma of death. Headaches may be present at the onset of the hemorrhage but are frequently not noted. Patients with thalamic hemorrhages are somewhat more likely to initially have a hemisonsory loss and then develop a hemiparesis. Gaze disturbances are also frequently noted. A progressive or gradual deterioration to a maximum neurological deficit characterizes the development of an intracerebral hemorrhage and usually distinguishes it from arterial occlusion due to embolus or thrombosis. Management of intracerebral hemorrhage: Patients with small intracerebral hemorrhages may be managed conservatively and observed for neurological deterioration. If there is no significant neurological deficit or if the maximum neurological deficit is not severe, no specific treatment other than anti-hypertensive treatment may be required. For patients who have more profound neurological deficits, hypertension should be treated cautiously and anti-convulsants and steroids should be administered. An extremely lethargic or comatose patient should be intubated to protect the airway. Angiograms may be performed on intracerebral hemorrhages that occur in unusual locations or associated with hemorrhage in the subarachnoid space, since an aneurysm or AVM may cause an intracerebral hemorrhage. A lobar hemorrhage in a young patient may be more suggestive of all underlying tumor or vascular malformation and therefore angiograms will frequently be indicated. Surgical treatment: Patients with accessible lobar hemorrhages who are deteriorating neurologically will often improve with surgery. Large dominant hemisphere basal ganglia lesions in elderly patients are probably not suitable candidates for surgery. The decision to operate depends on the patient's neurological deficit, evidence of progression of the deficit, the location of the hemorrhage and an assessment of the neurological prognosis, given all these factors, by the treating physicians. A craniotomy is usually performed over the most superficial aspect of the hemorrhage. The hemorrhage cavity is entered and the hematoma is aspirated and removed. Biopsies of the wall of the hemorrhage cavity are always done to determine if a tumor or vascular malformation may be present and causative. Many patients with intracerebellar hemorrhage may require a ventriculostomy to manage concomitant hydrocephalus.