Liver Transplant: What to expect
Information for patients and families
We would like you and your family to have some information on the “typical” experience
of a patient having a liver transplant. But please remember, everyone’s experience is
different. Use this description only as a general guide. If your course is different, please
don’t worry. As always, you and your family should talk with your nurses and doctors
about what you can expect from your surgery.
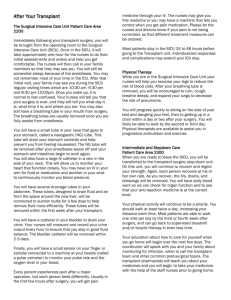
Intensive care: The first 24 hours
For the first 24 hours after your surgery, you will be in an intensive care unit (ICU). You
may remain in the ICU for a day or longer depending on your progress. Here, a team of
specially trained doctors, nurses, respiratory therapists, and others will provide constant
care and monitoring. Here are some of the things you can expect in intensive care:
When you first wake up you will have a “breathing tube” in your throat. You won’t be
able to speak at this point. Please remember that the nurses in this area are experts at
communicating with patients who cannot talk. They are very skilled at finding out what
you need.
You’ll have a few intravenous (IV) lines in your arms and in your upper chest or neck.
The IV’s are used to give you fluids and to draw blood. They are also used to give pain
medicine, and to give medicines to fight rejection and infection of your new liver.
A small rubber tube will also be in your nose. This tube goes into the stomach and
drains the normal fluids so you don’t feel sick to your stomach. Another tube that will
be used to give you special feedings may also be in the nose.
You won’t be eating or drinking during this phase of your recovery.
You’ll have a small tube (a catheter) in place in your bladder to drain your urine.
There will be a few tubes or drains going into your abdomen. These will drain excess
fluid from around your new liver. You may hear “suction” noises from these tubes.
Small patches on your chest are connected to a heart monitor and allow the staff to
watch your heart.
You’ll be either asleep or very drowsy during most of your stay in intensive care. When
you do begin to wake up, you may find soft restraints on your arms and legs.
Sometimes, you move around without knowing it as you are waking up. The restraints
are there to keep you safe and make sure the tubes and lines stay in place. Once you are
more fully awake, we’ll take these off and ask you to move your arms and legs around
on your own. This is one way to check your recovery from anesthesia.
You’ll find thick stockings on your legs. These are used to help your circulation.
Someone will be with you nearly all the time during this phase. They will be checking
your heart rate, blood pressure, urine output, temperature, and other signs of recovery.
Other staff members are available to help your family during this phase. Our social
work, case management, and pastoral care staff may all be called upon to be with
anyone who is anxious or upset.
Your family may visit you for very brief periods. But for most of the 24 hours
following surgery, you won’t be awake enough to visit with your family or friends.
They may want to wait at home for most of this first day. We can give them phone
numbers to call to check on your progress, and your surgeon will call them as soon as
your operation is over. You’re the one having the surgery, but this is the time that your
family needs to rest. They’ll be needed later to help you as you begin to really recover
from your transplant.
Transfer to Farr 6: The day after surgery
Most patients leave intensive care some time on the day after surgery. But some stay longer.
In general, a patient is moved soon after the breathing tube is removed and the oxygen level
and other signs are stable.
Here are some of the things you can expect on the day after your surgery.
Several of the tubes, including the breathing tube in your throat, will be taken out
before you are transferred to the transplant floor.
You’ll have a chest X-ray to check your lungs before you leave the ICU.
Blood tests to check your new liver will be done daily.
You’ll begin breathing exercises every hour while awake. This helps you recover and
helps prevent complications. A nurse or therapist will help you with the exercises.
The nurses will help you sit up several times. You’ll meet with a physical therapist who
will begin to work with you on an activity plan for your recovery.
You’ll feel very tired from your surgery and will need lots of rest.
You still won’t be able to eat or drink anything. But 6-12 hours after the tube is out of
your throat, you’ll be able to have ice chips.
The dressing over your wound will be removed and your incision will be checked.
(This is done each day.)
You’ll get pain medicine through your IV to make sure you are comfortable.
You’ll continue to receive medicine to fight rejection of your new liver and medicine to
help prevent infection. Your heavy leg stockings will still be on.
Three – five days after your surgery
At three – five days after surgery, you’re awake and alert. Every day, you’ll be able to do a
little more. In fact, moving around as much as you can is a very important part of your
recovery. This is also the time when your nurses and doctors will be teaching you how to
care for yourself once you go home. They’ll be asking you to take part in your own care
while you are still in the hospital so you’ll be more prepared to care for yourself at home.
Here are some of the things you can expect at three–five days after surgery:
You’ll be fully into your physical therapy program at this point. During this time, your
therapist will go over your exercise program with you. Although the program is
different for everyone, most patients follow this kind of schedule:
Day three – Walk in the hall with help two–three times.
Day four–five – Walk three times in the in the hall. Many people can walk
alone at this point, but you may need a walker for support.
On day five, you’ll also be able to take your own sponge bath. A nurse or someone
from your family will help you gather the supplies you need.
You’ll begin to start eating again. This goes slowly at first, so try to be patient. You’ll
start with liquids, then slowly move to solid food. You may meet with a dietitian about
your meal plan, and you’ll begin to learn about the diet you’ll need to follow at home.
More tubes and catheters will be removed during this period. Usually, the last tube that
helps drain the area of surgery is removed on about day five.
You’ll continue with breathing exercises every hour while awake, and your heavy leg
stockings will still be on until you are walking three–four times a day.
You’ll have blood drawn each day to check your progress. Your blood sugar will be
checked carefully by a small pin prick to the finger. Sometimes, diabetes (high blood
sugar) can develop after liver surgery. Your doctors and nurses will explain more if this
happens.
Your oxygen level will be checked by a small device that clips on your finger.
You will start to get your medicines in pill form rather than through your IV. This
includes pain medicine, as well as the medicines that fight infection and rejection of
your liver.
Your nurses will begin to teach you and your family about your medicines.
Your nurses will also begin to talk with you and your family about checking your
weight, blood pressure, and temperature. This will be important when you go home.
If you have high blood sugars after surgery, you may need to learn to check your blood
sugar on your own. Your nurses will begin to teach you how.
Now is the time to start thinking about what you’ll need after you go home. Our case
managers, social workers, and psychologists are available to help you and your family if
needed. We also recommend you watch Good Questions about Going Home, which airs
several times a day on the medical center’s Care!TV, channel 35.
Day five until the day of discharge ….Getting ready to go home
For the next few days, your recovery continues much as it has during days three –five. As
your day of discharge nears, here are some changes that you can expect in your routine:
Your breathing exercises are changed to every two hours while you are awake.
You’ll be up in the chair 45 minutes at a time, and you’ll walk in the hall at least three–
four times a day for 10 minutes.
You’ll be able to sit or stand by the sink and bathe yourself without help.
You will be eating regular food. If you’ve developed diabetes, you may need a diabetic
diet. A dietitian will explain this to you if needed.
Your physical therapist will continue to work with you and your family and answer any
questions you have about activity after discharge.
Your nurses will be working closely with you to make sure you know how to take your
medications safely once you go home. They will make sure you know the name,
purpose, and side effects of each of your medicines. You will be given a master
medication schedule so that you begin to learn what medications you take at various
times. Please refer to the schedule each time you take medications so that you become
familiar with your new drug regime. If you have any questions about your medications,
please be sure to ask your nurse.
Your nurses will teach you about things to expect after surgery. They will make sure
you and your family understand how to take care of any problem.
You will receive a schedule of all your follow-up appointments and blood tests.
We hope this brochure helps you and your family know what to expect when you come for
your liver transplant. If there is anything you don’t understand, please ask your doctors
and nurses. We want to make sure your stay is as safe and comfortable as possible.
This material was prepared by clinicians from the transplant service at Beth Israel Deaconess Medical Center. It is produced and
distributed by The Beth Israel Deaconess Learning Center. ©2004, Beth Israel Deaconess Medical Center. All rights reserved.
MC0776 REV 1/04