Paediatric Referral Guidelines for Cardiology Outpatients Clinics
advertisement
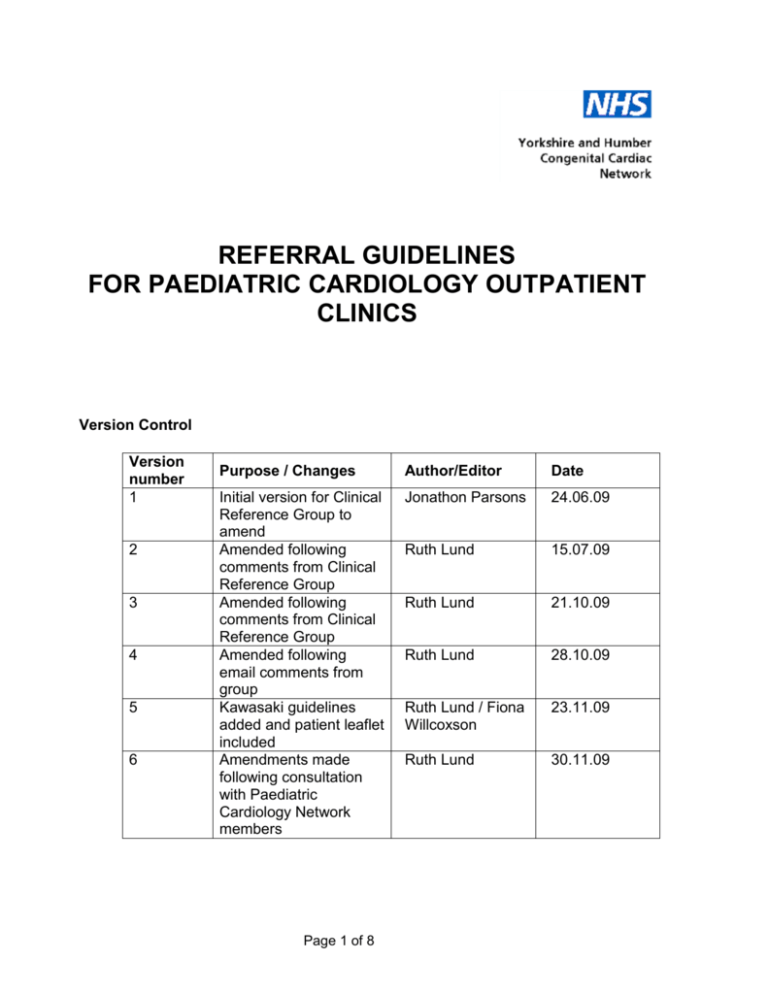
REFERRAL GUIDELINES FOR PAEDIATRIC CARDIOLOGY OUTPATIENT CLINICS Version Control Version number 1 2 3 4 5 6 Purpose / Changes Author/Editor Date Initial version for Clinical Reference Group to amend Amended following comments from Clinical Reference Group Amended following comments from Clinical Reference Group Amended following email comments from group Kawasaki guidelines added and patient leaflet included Amendments made following consultation with Paediatric Cardiology Network members Jonathon Parsons 24.06.09 Ruth Lund 15.07.09 Ruth Lund 21.10.09 Ruth Lund 28.10.09 Ruth Lund / Fiona Willcoxson 23.11.09 Ruth Lund 30.11.09 Page 1 of 8 These guidelines should be read in conjunction with the Yorkshire and Humber patient pathway diagram for children and young people with a suspected cardiac anomaly (Appendix 1). Referral pathways Emergency Emergency referrals should be made directly to the tertiary paediatric cardiology unit (Level 3 on the pathway diagram) after assessment and initial management in the outreach hospital. Routine These should be considered for assessment by a Paediatrician or team with expertise in Paediatric Cardiology in a Level 2 clinic before being referred to Level 3. Types of patients seen Patients generally belong to the following categories: Prenatal diagnosis Follow up of previously diagnosed congenital heart defects either in the tertiary unit or at the outreach hospital Follow up management of arrhythmias Follow up of post-operative cardiac surgical or intervention patients Referrals from GPs, paediatricians, community paediatricians, nurse specialists (these referrals should be made to a Paediatrician with expertise in Paediatric Cardiology). Prenatal diagnosis If prenatal diagnosis of a congenital heart defect has been made, then either the baby will need to be transferred to the tertiary unit or booked into the outreach paediatric cardiology clinic, as appropriate. Discussions need to take place with the tertiary centre about the location of delivery of the baby. If the baby is delivered locally in the outreach hospital, the baby will require evaluation after delivery and discussions with the tertiary unit will be necessary for transfer or for booking into the outreach paediatric cardiology clinic, as appropriate. Page 2 of 8 Neonates and young infants up to 8 weeks Previously unsuspected congenital heart defect in a newborn with a murmur and otherwise clinically well: 1. These babies need a review before discharge, including saturation monitoring. If the murmur is assessed as representing a significant risk of congenital heart disease, or there are other concerns such as desaturation (<95%), then the case will need to be discussed urgently with the paediatric cardiology team at LGI. 2. Babies with a murmur ought to be reviewed at 5 to 7 days by a paediatrician (including saturation monitoring) unless an experienced clinician can confidently assess them as being at low risk of having significant underlying congenital heart disease, in which case outpatient follow up should be arranged in 4 to 6 weeks. The information in appendix 3, along with a verbal explanation should be given to parents of all babies with a murmur. Clear instructions and guidance should be given to the parents and GPs if there are clinical concerns. 3. If there is a persistent murmur which is felt to be consistent with congenital heart disease at the 5 to 7 day review, then the baby should be booked into the local Level 2 paediatric cardiology clinic. The baby should follow the pathway outlined in Appendix 1. N.B. If the echocardiogram performed locally shows a cardiac defect which is unlikely to be haemodynamically significant, such as a small atrial septal defect, patent arterial duct or ventricular septal defect, or a minor degree of outflow obstruction, then the baby should be reviewed in 4 to 10 weeks in the Level 2 clinic. Neonates and infants diagnosed with congenital heart defects will require individual discussion between Levels 2 and 3 on a case by case basis. Page 3 of 8 New referrals of older infants (> 8 weeks) and children These referrals generally fall into the following categories: 1. Murmur felt significant enough to require diagnostic evaluation 2. Cyanosis 3. Chest pain 4. Palpitations 5. Syncope or dizziness 6. Referral for screening because of family history of congenital heart defect, cardiomyopathy or other syndromes 7. Kawasaki disease These patients should be seen by a paediatrician with expertise in paediatric cardiology: 1. Murmur: This guidance should not exclude general paediatricians from assessing the significance of the murmur. If the murmur is considered to be pathological, then the child should be referred to Level 2 care. If an abnormality is suspected clinically or found on the echocardiogram the patient should be referred to Level 3 as shown in Appendix 1. Minor lesions, such as small ventricular septal defects, atrial shunts, or mild pulmonary valve stenosis may be followed up in Level 2 if appropriate. Persisting lesions should be reviewed within 1 year by the paediatric cardiologist (Level 3). 2. Cyanosis: Oxygen saturation should be checked. If there is evidence of central cyanosis, then the patient should be discussed with the paediatric cardiologist. 3. Chest pain: Generally these patients and their parents require reassurance as to the musculo-skeletal nature of the chest pain. The patients can be seen in a general paediatric clinic. If a cardiac opinion is required, then they should be seen in the Level 2 clinic and investigations arranged if deemed necessary. If these are normal, then only in exceptional cases should a referral be made to the Level 3 service, otherwise the patient/parents can be reassured and discharged. 4. Palpitations: These patients should be seen in the general paediatric clinic and investigations arranged. These may include ECG, 24-hour ECG tape, and, if indicated, an echocardiogram and treadmill exercise test. If all these investigations are normal, the patient can be discharged. If there is still doubt or if there is an abnormality found, then the patient should be booked into the Level 2 clinic. Page 4 of 8 5. Syncope or dizziness: Patients should be seen by a paediatrician in the general paediatric clinic initially to find out whether the symptoms are cardiac or neurological in origin and so that appropriate investigations can be arranged. Such cases should be dealt with according to the DH Guidelines, which can be found on the following webpage, listed under ‘Initial Treatment 4 - Care Pathway for Children’. http://www.dh.gov.uk/en/Healthcare/Coronaryheartdisease/DH_4117048 6. Referral for advice because of family history of congenital heart defects, cardiomyopathy, and other syndromes: Services for Inherited Cardiac Conditions are provided by Leeds Teaching Hospitals Trust and Sheffield Teaching Hospitals Trust (in association with the Sheffield Children’s Hospital). These families can be discussed with the ICC service at the discretion of the paediatrician, rather than being referred to the paediatric cardiologist. Details of the Inherited Cardiac Conditions Service can be found by going to the following website and clicking on the relevant link: http://www.yorksandhumberhearts.nhs.uk 1. Kawasaki disease: Indications for early review during acute illness by Level 2: Atypical Kawasaki’s Pathological murmur Pericardial effusion Otherwise review at 10-14 days once over acute illness. Continue aspirin until review with Level 2 at 6 weeks - if normal discontinue aspirin and discharge from follow -up. If abnormal, continue to review via shared care between paediatric cardiologist (Level 3) and Level 2 clinician. Page 5 of 8 Children and young people diagnosed with congenital heart defects Suitable follow up for these patients will be decided jointly between the paediatric cardiologist and the paediatrician. Follow up will be dependant on the individual patient and may take place in the general paediatric clinic, the Level 2 clinic or the Level 3 clinic as appropriate. Page 6 of 8 Appendix 1 Patient Pathway for Children and Young People with a Suspected Cardiac Anomaly Suspected cardiac anomaly picked up by by GP, general paediatrician or neonatologist Most common reasons for referral to Level 2: • Murmur • Cyanosis • Chest Pain • Palpitations • Syncope or dizziness • Family history of Congenital heart disease disease*or or ICC (i.e. to be screened) Possible involvement from: • Surgeons • Cardiologists • Specialist Technicians • Paediatrician PaediatricianswSI wSIininCardiology Cardiology Discharge back to GP LEVEL 2 CLINIC Including diagnostic tests and results LEVEL 1 follow-up (general paediatrician) LEVEL 2 follow-up (paediatrician or team with expertise in cardiology) LEVEL 3 jointly agreed diagnosis, treatment and care package LEVEL 3 LEVEL 2 LEVEL 1 treatment and/or follow up at Tertiary Centre management by paediatrician or team with cardiac expertise in Secondary Care return to general paediatrician LEVEL 3 is specialist (Tertiary) level care and involves a paediatric cardiologist LEVEL 2 is Secondary level care from a paediatrician or team with expertise in cardiology LEVEL 1 is any other care at Secondary level Page 7 of 8 Appendix 2 Information Leaflet for Parents / Carers of babies found to have a murmur (embedded electronically – can be opened printed out as a trifold leaflet) Appendix 3 List of working group participants: Eva Stuwe; Paediatrician; Scarborough Fiona Willcoxson; Paediatric Cardiologist; Leeds Jane Allen; Sonographer; York Jonathan Parsons; Paediatric Cardiologist; Leeds Jo Quirk; Nurse Specialist; Leeds Matthew Babirecki; Paediatrician; Airedale Mike Fresson; Nurse Specialist; Leeds Porus Bustani; Neonatologist, Sheffield Rupal Patel; Paediatrician, Hull Sam Bainbridge; Sonographer; Bradford Sam Oddie; Neonatologist; Bradford Sandeep Kapoor; Paediatrician; North Lincs and Goole Page 8 of 8