Psychotherapy And Medication Options For Depression
advertisement
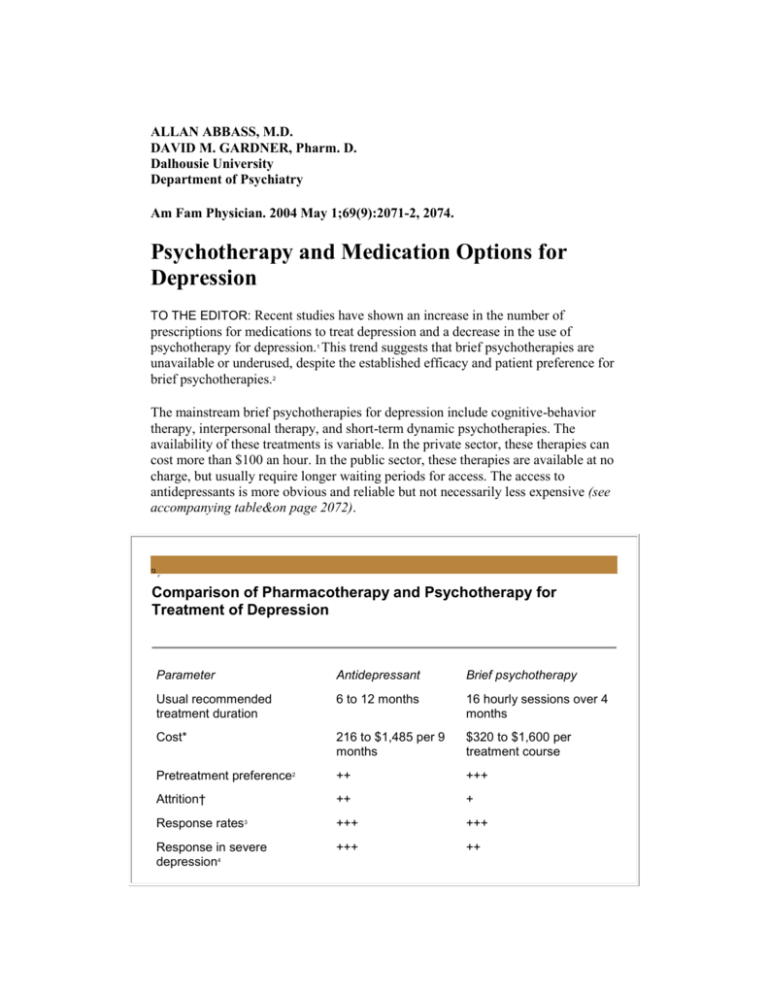
ALLAN ABBASS, M.D. DAVID M. GARDNER, Pharm. D. Dalhousie University Department of Psychiatry Am Fam Physician. 2004 May 1;69(9):2071-2, 2074. Psychotherapy and Medication Options for Depression TO THE EDITOR: Recent studies have shown an increase in the number of prescriptions for medications to treat depression and a decrease in the use of psychotherapy for depression.1 This trend suggests that brief psychotherapies are unavailable or underused, despite the established efficacy and patient preference for brief psychotherapies.2 The mainstream brief psychotherapies for depression include cognitive-behavior therapy, interpersonal therapy, and short-term dynamic psychotherapies. The availability of these treatments is variable. In the private sector, these therapies can cost more than $100 an hour. In the public sector, these therapies are available at no charge, but usually require longer waiting periods for access. The access to antidepressants is more obvious and reliable but not necessarily less expensive (see accompanying table&on page 2072). Comparison of Pharmacotherapy and Psychotherapy for Treatment of Depression Parameter Antidepressant Brief psychotherapy Usual recommended treatment duration 6 to 12 months 16 hourly sessions over 4 months Cost* 216 to $1,485 per 9 months $320 to $1,600 per treatment course Pretreatment preference2 ++ +++ Attrition† ++ + Response rates3 +++ +++ Response in severe depression4 +++ ++ Remission rate2,3 ++ to ++++ ++ to +++ Relapse rates on cessation2,5 ++ + Adverse effects +++ + Access/convenience ++++ ++‡ Key: + = 0 to 25 percent effect; ++ = 25 to 50 percent effect; +++ = 50 to 75 percent effect; ++++ = at least a 75 percent effect. *-Cost range for antidepressant treatment is based on the purchase prices (including a $9 monthly dispensing fee) of the least expensive selective serotonin reuptake inhibitor (SSRI) at minimum dosage (fluoxetine [Prozac], 10 mg per day) to the most expensive SSRI at maximum dosage (citalopram [Celexa], 60 mg per day). Cost range of brief psychotherapy is based on publicly provided therapy to private psychologist-provided therapy. †-Early treatment withdrawal from ongoing therapy (attrition) was used to measure treatment acceptability. ‡-Access to psychotherapy may be higher than we have indicated, especially in urban settings. However, caregivers, because of system problems, often censor this option without fully exploring it with their patients. Information from references 2 through 5. For most patients with depression of mild to moderate severity, psychotherapy and antidepressants appear equally effective.3 In severe cases, antidepressants may provide greater symptomatic relief.4 Psychotherapy is preferred by patients, and treatment tolerance and acceptance appears better.2,3 Comparative studies,5 which have included only older antidepressants (e.g., tricyclic antidepressants, monoamine oxidase inhibitors), have demonstrated lower dropout rates with brief psychotherapies (22.2 percent) than with pharmacotherapies (37.1 percent). The fact that dropout rates with the use of newer antidepressant agents remain high with only a modest advantage over older antidepressant agents implies that this advantage for psychotherapies persists. This greater acceptance may be partly related to adverse effects, which are a common reason for prematurely terminating therapy with antidepressant drugs. Adverse effects, at least in terms of somatic side effects, do not appear to be a factor with psychotherapy. Some studies5 also have shown an enduring effect with psychotherapy that reduces the risk of relapse and recurrence after treatment has been terminated (20 percent versus 50 percent relapse at two years for psychotherapy and pharmacotherapy, respectively). Even though the literature is unclear, combinations of psychotherapy and antidepressant medications may have an added effect in certain patients5 and may be less costly to the health care system than pharmacotherapy alone.6 Given the equal efficacy and patient preference for psychotherapies, we are compelled to examine why the rates of psychotherapy use have decreased while the prescribing of antidepressant medications has increased. The expensive and effective marketing of pharmaceutical companies has made a generation of physicians well versed in the prescription of antidepressants. Is it possible that physicians are not aware, because of "marketing" deficits, of the effectiveness, acceptability, and preferences for psychotherapies? Is there an education bias in medical schools and residency programs that fails to emphasize these options? Or, is it because physicians cannot access psychotherapies even if that is what their patients would prefer? It is vital that we answer these questions, in the service of our patients with depression. REFERENCES 1. Tanielian TL, Marcus SC, Suarez AP, Pincus HA. Datapoints: Trends in psychiatric practice, 1988-1998: II. Caseload and treatment characteristics. Psychiatr Serv 2001;52:880. 2. Chilvers C, Dewey M, Fielding K, Gretton V, Miller P, Palmer B, et al. Antidepressant drugs and generic counselling for treatment of major depression in primary care: randomised trial with patient preference arms. BMJ 2001;322:772-5. 3. Casacalenda N, Perry JC, Looper K. Remission in major depressive disorder: a comparison of pharmacotherapy, psychotherapy, and control conditions. Am J Psychiatry 2002;159:1354-60. 4. Elkin I, Gibbons RD, Shea MT, Sotsky SM, Watkins JT, Pilkonis PA, et al. Initial severity and differential treatment outcome in the National Institute of Mental Health Treatment of Depression Collaborative Research Program. J Consult Clin Psychol 1995; 63:841-7. 5. Canadian Psychiatric Association, Canadian Network for Mood and Anxiety Treatments (CANMAT). Clinical guidelines for the treatment of depressive disorders. Can J Psychiatry 2001;46 (suppl 1):5S-90S. 6. Burnand Y, Andreoli A, Kolatte E, Venturini A, Rosset N. Psychodynamic psychotherapy and clomipramine in the treatment of major depression. Psychiatr Serv 2002;53:585-90.