Neuropharmacology_Paper
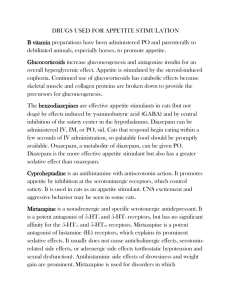
advertisement
Mirtazapine in Pregnancy 1 Running head: MIRTAZAPINE EXPOSURE IN PREGNANCY Mirtazapine exposure during pregnancy: literature review and implications Barnard College Sarah Stillman Mirtazapine in Pregnancy 2 Background During childbearing years, depression affects nearly nine percent of the America female population. Moreover, about one-fifth of pregnant mothers experience depressive symptoms during pregnancy (Frieder, 2011). In today’s culture of popping pills for every symptom, the use of antidepressants becomes a conundrum when considering the adverse side effects for the developing fetus. Studies found negative birth outcomes, not limited to low birth weight, shorter gestation and increased risk for cognitive and behavioral effects for newborns born to depressed mother, even without pharmacological treatment (Frieder, 2011). However, children born to depressed mothers tend to have more sleep problems, feeding issue and deficits to environmental stimulation behaviors occur at a higher rate in children of depressed mothers. There seems to be no clear solution. In 2004, the Federal Drug Association changed labeling criteria to include the neurobehavioral risks for newborns when mothers use Selective Serotonin Reuptake Inhibitors (SSRIs) and Selective Norepinephrine Reuptake Inhibitors (SNRIs). Spurred by the controversial debate on antidepressant use during pregnancy, the issue of negative birth outcomes and mental health was brought to the forefront of conversation. Despite a lack of conclusive evidence, doctors recommend to pregnant women that they suspend usage for fear of harming the unborn child. Needless to say, the use of antidepressants in pregnancy requires constant maintenance and many women are unable to receive pharmacological treatment for depression while pregnant. Not only does this put these women at significant danger for withdrawal symptoms for those who stop immediate once finding out that they are pregnant. The associated negative birth outcomes and antidepressant use during pregnancy places a major stress of mother who have to Mirtazapine in Pregnancy 3 balance their own mental health with the possible harm to their newborn. So mothers are forced to make a difficult choice without conclusive facts. Since the early 1990s, many short-term studies, both animal and human, reviewed the developmental effects of antidepressants. The studies looked at neurodevelopmental, behavioral, and birth outcomes, however findings were mixed. Research has been centered on the three main types of antidepressants, tri-cyclic antidepressants (TCAs), SSRIs and SNRIs. However a newer drug, Mirtazapine has been less studied in the pregnant population, and these has been no comprehensive review of literature. Mirtazapine (Remron) is a mixed mechanism, serotoninnorepinephrine reuptake inhibitor (SNRI) that is used to treat depression and anxiety but also nausea and hyperemesis gravidarum. It is a unique antidepressant that decreases neurotransmitter synthesis and release by blocking both noradrenergic alpha-2 and 5-HT1a autoreceptors that ultimately increase noradrenergic and serotonergic activity (Ettinger, 2011). The use of antidepressants in pregnancy is a multi-pronged issue. Not only is depression a leading mental health problem, the risks to mother and fetus if left untreated are substantial. Mothers fear harming the developing fetuses, but must also precariously balance their own mental health concerns. However this fear is aggravated by the large numbers of studies, on antidepressants exposure in pregnancy and its association to negative birth outcomes, because evidence is two-sided. Despite the swaths of research focused on SSRIs and SNRIs in a pregnant population, little research has inquired about the effects of mirtazapine during pregnancy and its association to negative birth outcomes. Mirtazapine is a new antidepressant and has yet to receive the proper attention about its implications during pregnancy. It would seem beneficial to review current findings to formulate conclusions and examine necessary steps for further scientific exploration. Mirtazapine in Pregnancy 4 Literature Review The objective of this literature review was to examine the findings of past research on the antidepressant, Mirtazapine in pregnancy. A thorough search located only four studies, one animal study, 1 comparison study and two case studies on mirtazapine. Due to the limited research on this drug, other literature, looking at SSRIs and TCAs in pregnancy, was used a point of comparison to understand the evidence on Mirtazapine. The lack of research on mirtazapine not only speaks to the need for further research in this area, but also severely limits the ability to summarize conclusive evidence. Summarized antidepressant research covers five areas: effects on pregnancy outcomes, effects on birth outcomes, teratogenicity, neurodevelopmental effects on offspring, and behavioral effects on offspring. In total the reviewed research includes four animal studies, one on mirtazapine and two on SSRIs, and seven human studies, one prospective comparative studies on mirtazapine, two case reports on mirtazapine and five short-term controlled cohort studies using SSRIs and TCAs. Effects on pregnancy outcomes Over the years, many studies have researched the risk of spontaneous abortion and the use of antidepressants. Regarding Mirtazapine, a prospective comparison study of 104 pregnant had three comparison groups for pregnant women, one exposed to mirtazapine, one diseasematched group taking another antidepressant and one non-depressed group not taking antidepressants. Women, in the mirtazapine-exposed group found 20 spontaneous abortions, at a rate of 75% for live births compared to 85.5% live births for the non-antidepressant group. A majority of the spontaneous abortions occurred in the first trimester when 95% of women took mirtazapine. After analysis there was not a significant difference between the rates of spontaneous abortion in the mirtazapine group compared to other antidepressants. However the Mirtazapine in Pregnancy 5 rate of spontaneous abortions in both antidepressant groups was significantly higher than the non-antidepressant group (Djulus, Koren, Einarson, Wilton, Shakir, Diav-Citrin, Kennedy, Lavigne, De Santis & Einarson, 2006). Contrary to this finding, a case report of six pregnant women taking mirtazapine at varying doses throughout pregnancy, and none of the pregnancies resulted in spontaneous abortion. Two patients had a history of past spontaneous abortion, but the reasons were unknown. However for this study the results were not statistically significant because of the small sample size and method of self-report for past reproductive history (Saks, 2001). In an animal study, when comparing litter size in rats, researchs found that in both double therapeutic dose (DTD) and therapeutic dosage (TD) experienced significantly smaller litter size than control (Sahoo, Pattnaik & Mishra, 2010). Extrapolating this data is difficult since it is impossible to represent litter size in a human population. However the animal study might suggest similar phenomena to spontaneous abortion in humans. In all the studies, future research needs to expand the sample size for studying mirtazapine’s association to risk of spontaneous abortion. In comparison to Mirtazapine, in a prospective survey study an incidence of higher miscarriages amongst the fluoxetine group (SSRI) compared to mothers not taking antidepressants. Amongst TCAs and SSRIs comparison groups, both had a tendency for high miscarriage than non-teratogen group. However neither of these high-risk groups produced a significant difference (Pastuszak, Schick-Boschetto, Zuber, Feldkamo, Pinelli, Sihn, Donnenfeld, McCormack, Leen-Mitchell, Woodland, Gardner, Horn & Koren, 1993). One limitation of this study was the small sample size of 128 participants, which made it impossible to see significant differences in the subgroups. Pastuzak et. al (1993) sited that data on the topic of spontaneous miscarriages was challenging to reconcile because depressed mothers typically have a higher Mirtazapine in Pregnancy 6 incidence of spontaneous abortions, even without an antidepressant. In summary, the small sample size in the reviewed literature limits conclusive data about a higher rate of spontaneous abortions due to mirtazapine. If there is an association, there is only a trend towards the hypothesis that mirtazapine exposure increases the risk of spontaneous abortion in a pregnant population. Effects on birth outcomes Low birth weight and shorter gestation period are a few poor birth outcomes often are associated with the use of antidepressants during pregnancy. Several studies suggested an association to negative birth outcomes due to mirtazapine. However other studies have not found this relationship with other associated antidepressants. Sahoo et al. (2010) found amongst a pregnant rat population significantly shorter gestation period and lower birth weight for rats that received DTD compared to TD and control groups. Rats who received TD had a significantly smaller litter size compared to controls but there was no significant difference between gestation time and birth weight when compared to controls. In the case report of six mothers taking mirtazapine throughout pregnancy, there was no preterm labor or low birth weight (Saks, 2001). Contrary to the previous findings, Djulus et al. (2011) in a comparative study of 77 mothers taking mirtazapine, found a higher incidence of preterm birth, lower gestational age at birth and lower birth weight. A few limitations in this study include, the small sample size, which made it impossible to detect any statistical power. In the animal study, low birth weight and shorter gestation were found only in the DTD group, but this result is difficult to translate to a human population that only takes a TD. In the case reports each mother presented was prescribed a different dose of Mirtazapine, the low TD nor high TD appeared to have impacted the pregnancy. Mirtazapine in Pregnancy 7 Similarly to Mirtazapine, research on SSRIs demonstrated trends of shorter gestational age but lacked conclusive evidence on low birth weight. Pastuszak et al. (1993) demonstrated that there was no significant difference in pregnancy outcomes, low birth weight or preterm delivery amongst 104 cases of mothers who used Prozac during the first trimester of pregnancy. Zeskind & Stephens (2004) found no statistical difference of low birth weight or preterm delivery in a matched-subject pool of 17 women who took a SSRI until delivery. Amongst all the cases, only 1 SSRI-exposed newborn was born before 37 weeks. Zeskind et al.’s (2004) findings suggest that there is no increased risk, however the small sample size does not provide sound statistical weight. A possible caveat for Pastuzak et al.’s (1993) findings is that antidepressant use during the third trimester is associated with lower birth weight and lower gestational age. Their study only looked at mothers who took Prozac in the first trimester. Supporting the correlation between third term exposure to SSRIs, Costei, Kozer, Ho, Ito & Koren (2002) illustrated a trend for lower birth weight at a p-value of .09 and a significant difference of preterm labor at a p-value of .02 for fetuses exposed to SSRI, paroxetine, in the third trimester. In conclusion, it appears that there is mixed evidence of antidepressant exposure and its effects on birth outcomes. However, SSRI evidence contradicts the findings about Mirtazapine, which suggest a stronger incidence of preterm labor particularly due to exposure in the third trimester. Terotogenicity Some studies indicated a relationship between antidepressant exposure in pregnancy and congenital malformations. However in the three studies of mirtazapine in pregnancy there was no evidence of a correlation between exposure and birth defects at TDs. Sahoo et. al. (2010) did note that the physical development of teeth and weight gain of rat pups in the DTD group was Mirtazapine in Pregnancy 8 significantly than TD and control group. No study on mirtazapine has looked at the long-term development of newborns and children exposure to mirtazapine in pregnancy. Amongst several studies exposure to TCAs or SSRIs throughout pregnancy did not produce significant differences of congenital malformations (Coleman, Christensen, Gonzalez, Rayburn, 1999; Costei et al., 2002; Nulman, Rovet, Donna, Stewart, Wolpin, Gardner, Thesis, Kulin & Koren, 1997; Patstuszak et. al, 1993; Simon et. al., 2002). In four human studies and one mouse study no major malformations were found. Coleman et.al (1999) found no facial abnormalities in a controlled study of 21 mice exposed to paroxetine, at upper TD. Concurrent with this evidence, Patstuzak et. al. (1993) did not see a higher incidence of major malformation amongst a 128 women exposed to fluoxetine in the first trimester. Another study investigating the neurodevelopment of infants, in a sample size of 217 pregnant women, split equally between exposure only in the first trimester and full term, exposed to TCAS and SSRIs found similar rates of malformations amongst the antidepressant group and controls (Nulman et.al, 1997). In a study of 314 pregnant women exposed to either a TCA or SSRI during pregnancy found no significant increase in major malformations, minor malformation or specific malformation compared to unexposed control. Costei et al. (2002) detected a higher incidence of neonatal complications due to paroxetine exposure in the third trimester in a human population. However none of these complications were major malformations and all conditions resolved after a short period of time. Nevertheless, this trend indicated involved mechanisms of drug exposure because infants exposed only during the first or second trimester did not experience such complications, so more research is needed to replicate these findings. In summary, a majority of reviewed studies demonstrated that there was not a higher incidence of malformation in infant exposed to an antidepressant. Though neonatal complications did occur, this seemed to correlate specifically Mirtazapine in Pregnancy 9 to exposure late in the third trimester. Though mirtazapine works on different mechanisms in the brain, if it were to follow the same outcomes as other antidepressants, it would not cause major malformations. Neurodevelopmental effects When determining the drawbacks and benefits of antidepressant use in pregnancy, it is important to consider the short- and long-term effects on the fetus. There are only a couple of studies that look at the long-term effects on the infant and only one animal study looked at longterm effects on offspring in a mirtazapine controlled group. Moreover, the studies vary in methodology, specifically in the assessments used to measure developmental success, which create a challenge for comparing results. There were two studies that reviewed neurodevelopmental effects of mirtazapine in pregnancy. In the only long-term study found, Sahoo et. al (2010), as discussed previously, completed a trial comparing DTD and TD doses of mirtazapine compared to a control in rats. Cognition and memory were tested on the 24th and 61st day post-birth. On the 24th day, DTD exposed pups showed a significant slower learning ability to escape the Morris water maze test compared to TD and control group. However, on day 61, there was no significant different between any of the three groups. In the case report of 6 women using mirtazapine during pregnancy, all delivered healthy babies with APGAR scores above 7 at 1 minute and 9 at 5 minutes. These findings demonstrate that there were no immediate or clear neurodevelopmental effects as a result of mirtazapine. However this study did not follow-up with mothers, so long-term effects were unknown. Similarly, 3 other studies investigating the neurodevelopmental effects of antidepressants found that there was not a significant difference between fetuses exposed and not exposed to an antidepressant. In an animal study conducted by Vohees, Acuff-Smith, Schilling, Fisher, Moran Mirtazapine in Pregnancy 10 & Buelke-Sam (1994), they examined the effects of fluoxetine and neurodevelopmental changes due to neurotoxicity. After completing the designed motor activity the data showed no significant treatment effect between exposed and unexposed rats. Researchers suggested that fluoxetine was not significantly toxic in a developing rat’s central nervous system. A clear limitation with this study is that fluoxetine persists longer in a human fetus’s CNS and therefore might produce a different result. Simon et. al. (2002) looked a neurodevelopmental effects in the human nervous system to see if there were significant differences between those exposed to TCAs or SSRIs and unexposed fetuses. Evidence illustrated that TCAs did not differ significantly in APGAR scores, however fetuses exposed to SSRIs had significantly lower APGAR scores than unexposed infants. Though this might appear as evidence for neurodevelopment effects of SSRIs, when controlled for premature delivery there was no longer a significant difference. This is important because the use of SSRIs in pregnancy is associated with premature delivery. Therefore, it might be suggested that SSRI exposure in pregnancy indirectly may cause neurodevelopment effects due to shorter gestation. A major limitation to this study was that mothers reported a high use of alcohol tobacco, marijuana and cocaine, all substances that significantly increase the risk of premature delivery (Simon et. al, 2002). Nulman et. al. completed a study of 217 mothers exposed to an SSRI or TCA, and delivered a healthy singleton baby at full term. This was one of the few long-term studies that examined a child between 16 – 82 months post-birth. Analysis showed no significant difference in cognitive, language or behavioral developments compared to an unexposed group. Also timing of exposure during pregnancy did not have a significant effect on IQ, as measured by the Bayley Scales of Infant Development or McCarthy Scales of Children’s Abilities. As discussed by Simon et. al. (2002), premature delivery can have a significant impact on neurodevelopment, and those exposed to mirtazapine or another Mirtazapine in Pregnancy 11 antidepressant are at risk for shorter gestational age. Though as discussed by Sahoo. et. al. (2010), it appears that offspring do make up for developmental delays with time, so there is hope of recovery. Behavioral Effects Little evidence was found discussing the behavioral effects of antidepressants in human populations, this is most likely due to the fact there are few long-term studies. Three animal studies were located discussing the effects of antidepressants, one on mirtazapine and another on paroxetine. Sahoo et. al. (2010) found the prenatal exposure to mirtazapine significantly affected the motor development of rat pups. In both the TD and DTD pups they were less active on the reflex activity on day 4 and 8 post-birth compared to the control, which demonstrated an inability to right itself from a supine position in two seconds. DTD pups were unable to effectively complete the swimming ability test and ascending mesh wire task, which tested the pup’s ability to respond to different environments where their body needed to be altered. These three measures exemplified how mirtazapine had behavioral effects in a rat pup population. However in a study of mouse pups exposure to paroxetine, no significant behavioral changes were observed. In a randomized control-group study, 21 mice were exposed two weeks before gestation and throughout gestation to paroxetine to achieve a concentration in rat serum of upper therapeutic level equivalent in humans (Coleman et. al, 1999). Offspring went through a battery of tests looking a motor, anxiety, reproduction and depression tasks in their juvenile and adult development. There were no significant differences between exposed and control group in social play, locomotor activity, and anxiety and depression tasks. However exposed group were significantly more likely to have separation vocalization. Research has suggested that this might be due to withdrawal symptoms and not specifically behavioral development effects (Frieder, Mirtazapine in Pregnancy 12 2011). These two studies demonstrate opposing findings, however it is possible that mirtazapine does produce behavioral changes in fetus that SSRIs do not. To draw more conclusive findings, future research should conduct studies looking at the long-term behavioral effects of mirtazapine in a human population. Conclusion Depression is one of the most commonly diagnosed mental disorders in America, and it's prevalent in 7-9% of pregnancies, which means its effects impact the mother, fetus and whole family. Pregnancy is a stressful time, physically and mentally. Coupled with maternal depression, it can increase the risk of impaired behavioral, cognitive and birth outcomes for the fetus. Therefore, some form of treatment is necessary. However more severe cases of depression might require an antidepressant. Mirtazapine is a newer antidepressant that has properties particularly helpful for relieving nausea and vomiting, which seem particularly appropriate for women experiencing morning sickness. However the risks and benefits of using mirtazapine and other antidepressants during pregnancy are unclear. Conflicting and even contradictory evidence provides an unclear path for pregnant mothers and clinicians. The current literature review hoped to summarize what has been found on exposure to mirtazapine in pregnancy and compare it to findings on other commonly used medications like SSRIs and TCAs. Evidence centered on five main topics including pregnancy outcomes, birth outcomes, teratogenicity, neurodevelopmental effects and behavioral effects. Though evidence is mixed, there seem to be a few clear trends. Ultimately, more research is needed to draw conclusive evidence and correct many of the limitations of past studies. From the limited research on mirtazapine, it appeared that mirtazapine exposure during the first trimester increased the risk of spontaneous abortion. Compared to other antidepressants Mirtazapine in Pregnancy 13 mirtazapine was no worse than any other. Together, antidepressants taken in the first trimester increased the incidence of spontaneous abortion in human populations and produced smaller litter size in rat samples. The exact mechanisms of why spontaneous abortion is more likely has yet to be researched. There were two main trends on birth outcomes. Mirtazapine increased the risk of low birth weight and preterm labor. However evidence on other antidepressants did not suggest such a cause. It is possible that due to the small sample size, those who participated were not representative of a whole. Another confounding variable was the various doses of mirtazapine given to the mother in pregnancy and the timing of exposure. Future studies will need to control for these factors to see if dosage or timing affect birth outcomes in a mirtazapine exposed population. Studies on antidepressants have postulated that exposure in the third trimester may be at fault for preterm labor; where as exposure in the first trimester is connected to spontaneous abortions. Future studies on mirtazapine will need to investigate this further. From the reviewed literature, there was no significant increase in malformations in fetuses exposed to mirtazapine during any point in gestation. Evidence on other antidepressants concur with this finding, siting that there was a higher likelihood of neonatal complications but the exact origins cannot be connected to mirtazapine. In terms of neurodevelopmental effect, mirtazapine showed a significant impact early on in post-birth test, however the difference disappeared with maturation. No studies have been completed on neurodevelopmental processes in a human population exposed to mirtazapine. SSRI evidence in rats suggested that there was no significant difference. In a human population, there have been various methodologies, which make comparing data difficult. APGAR scores typically give to every child post-birth, appeared to be significantly Mirtazapine in Pregnancy 14 lower in the SSRI group. However this was due to prematurity and not antidepressant exposure. Nevertheless SSRIs do increase the risk of premature delivery and indirectly may cause neurodevelopment delays. Little research has looked at behavioral effects of antidepressants in humans. However there has been research done in an animal population. Significant behavioral effects were seen in the mirtazapine population but were not observed in an SSRI rat population. Because of the limited data this evidence needs to be replicated to draw conclusive findings about mirtazapine possible harmful effects on behavior. Another difficulty was that no studies looked at behavioral mechanisms in a human population, making it difficult to generalize these findings. Despite the limited research, when put into context with the vast amount of research on SSRIs and TCAs, mirtazapine in pregnancy appears to have some risks. Though more research needs be completed to draw conclusive findings, initial research gathered suggests exposure to mirtazapine during pregnancy increases the risk of spontaneous abortion, premature delivery, low birth weight and possible behavioral effects. This literature reviewed pregnancy outcomes due to Mirtazapine in neonates after delivery. No research has looked at the effects of Mirtazapine on neural circuitry in neonates or in an animal population. This is a body of research desperately needs to be advanced. However, some work has been done in other braches of antidepressants, specifically with SSRIs. Though mentioned only briefly, Coleman et. al. (1999) found rat pups exposed to paroxetine were more likely to have separation vocalization. This is poignant because it suggests that the offspring are going through withdrawal symptoms. A new branch of research has begun to look at antidepressant withdrawal in the neonate. Evidence suggests due to antidepressant’s inhibition mechanisms, for example to the reuptake transporter protein, there are alternations in synaptic Mirtazapine in Pregnancy 15 concentrations, synaptogenesis and glial proliferation (Maciag, Simpson, Coppinger, Lu, Wang, Lin & Paul, 2006). Maciag et. al (2006) suggested through their review of literature that this exposure will create subtle changes in motor development and control, as observed in animal populations, which resulted from decreased firing in the dorsal raphe and density of receptors. The reasoning for why these mechanisms formed abnormally is unknown, however it was proposed that these alternation were caused by exposure during critical periods of neuronal development. Researchers extended these findings to hypothesize that similar effects would be found in humans, whereby producing enduring effects for the neonate into its adult life. Questions should be raised about the research presented. There are three main limitations to the research, limited sample sizes, lack of Mirtazapine research in human populations, and no research on Mirtazapine’s effects on neural circuitry. Sample size needs to be addressed in future work. A larger sample size would increase the statistical power of the findings as well as clarify other potential mediating effects. It would also allow for possible detection of covariates between groups. The limited number of studies on mirtazapine provides a pool of less than 100 women exposed to mirtazapine during pregnancy. This small sample can cause anomalies and decreases generalizability. Future research should increase sample sizes to allow for examination of infrequent outcomes and provide stronger statistical significance. The next set of studies should investigate and control for timing, duration and dosage of prenatal mirtazapine exposure, as well as continue to look for potential long-term effects in the infant. It is crucial that research produce longitudinal studies in a human population, because research has focused mainly on immediate post-birth measures, which does not take into account that major development of neurotransmitter systems continue up to 30 months, and apoptosis continues up to 25 years of age (Maciag et. al., 2006). By taking these next steps, it will be to begin to tease apart the impact Mirtazapine in Pregnancy 16 use of mirtazapine in pregnancy and the role maternal depression plays in understanding pregnancy and birth outcomes at the neuronal level that might amass long-term neurological and behavioral abnormalities. Mirtazapine in Pregnancy 17 References Coleman, F., Christensen, H., Gonzalez, C., & Rayburn, W. (1999). Behavioral changes in developing mice after prenatal exposure to paroxetine (paxil). American Journal of Obstetric and Gynecology, 181(5), 1166-1171. Costei, A., Kozer, E., Ho, T., Ito, S., & Koren, G. (2002). Perinatal outcome following third trimester exposure to paroxetine. Archives of Pediatric and Adolescent Medicine, 156, 1129-1132. Djulus, J., Koren, G., Einarson, T., Wilton, L., Shakir, S., Diav-Citrin, O., Kennedy, D., Lavigne, S., De Santis, M., & Einarson, A. (2006). Exposure to mirtazapine during pregnancy: a prospective, comparative study of birth outcomes. The Journal of Clinical Psychiatry, 67(8), 1280-1284. Ettinger, R. (2011). Psychopharmocology. (1st ed., p. 83). Upper Sadle River: Prentice Hall. Frieder, A. (2011). Antidepressant use during pregnancy. Expert Review of Obstetrics and Gynocology, 6(3), 285-294. Nulman, I., Rovet, J., Stewart, D., Wolpin, J., Gardner, H., Thesis, J., Kulin, N., & Koren, G. (1997). Neurodevelopment of children exposed in utero to antidepressant drugs. The New England Journal of Medicine, 336(4), 258-262. Pastuszak, A., Schick-Boschetto, B., Zuber, C., Feldkamp, M., Pinelli, M., Sihn, S., Donnenfeld, A., McCormack, M., Leen-Mitchell, M., Woodland, C., Gardner, A., Horn, M., & Koren, G. (1993). Pregnancy outcome following first-trimester exposure to fluoxetine (prozac). The Journal of the American Medical Association, 269(17), 2246-2248. Sahoo, J., Pattnaik, A., & Mishra, N. (2010). Behavioral and developmental changes in rats with prenatal exposure to mirtazapine. Scientia Pharmaceutica, 78, 451-463. Mirtazapine in Pregnancy 18 Saks, B. (2001). Mirtazapine: treatment of depression, anxiety, and hyperemesis gravidarum in the pregnant patient. a report of 7 cases. Archives of Women's Mental Health, 3, 165-170. Simon, G., Cunningham, M., & Davis, R. (2002). Outcomes of prenatal antidepressant exposure. The American Journal of Psychiatry, 159(12), 2055-2061. Vorhees, C., Acuff-Smith, K., Schilling, M., Fisher, J., Moran, M., & Buelke-Sam, J. (1994). A developmental neurotoxicity evaluation of the effects of prenatal exposure to fluoxetine in rats. Fundamental and Applied Toxicology, 23, 194-205. Zeskind, P., & Stephens, L. (2007). Maternal selective serotonin reuptake inhibitor use during pregnancy and newborn neurobehavior. Pediatrics: Official Journal of the American Academy of Pediatrics, 113(2), 368-375.