Visual System-94
advertisement
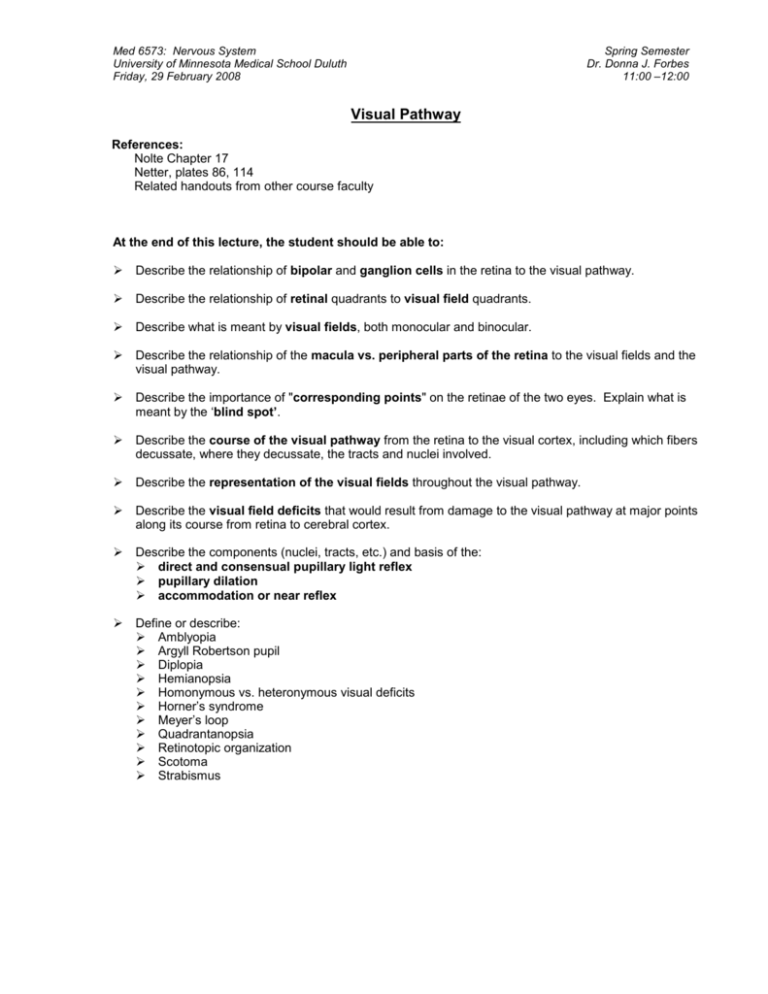
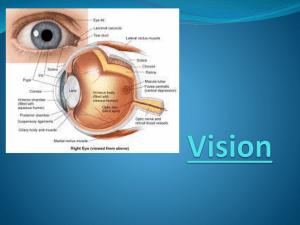
Med 6573: Nervous System University of Minnesota Medical School Duluth Friday, 29 February 2008 Spring Semester Dr. Donna J. Forbes 11:00 –12:00 Visual Pathway References: Nolte Chapter 17 Netter, plates 86, 114 Related handouts from other course faculty At the end of this lecture, the student should be able to: Describe the relationship of bipolar and ganglion cells in the retina to the visual pathway. Describe the relationship of retinal quadrants to visual field quadrants. Describe what is meant by visual fields, both monocular and binocular. Describe the relationship of the macula vs. peripheral parts of the retina to the visual fields and the visual pathway. Describe the importance of "corresponding points" on the retinae of the two eyes. Explain what is meant by the ‘blind spot’. Describe the course of the visual pathway from the retina to the visual cortex, including which fibers decussate, where they decussate, the tracts and nuclei involved. Describe the representation of the visual fields throughout the visual pathway. Describe the visual field deficits that would result from damage to the visual pathway at major points along its course from retina to cerebral cortex. Describe the components (nuclei, tracts, etc.) and basis of the: direct and consensual pupillary light reflex pupillary dilation accommodation or near reflex Define or describe: Amblyopia Argyll Robertson pupil Diplopia Hemianopsia Homonymous vs. heteronymous visual deficits Horner’s syndrome Meyer’s loop Quadrantanopsia Retinotopic organization Scotoma Strabismus Med 6573: Nervous System I. Visual System Pathways The Visual Pathway (Netter pl. 114; Nolte fig. 17-24 to 17-26) Reti na op tic nerve op tic ch iasm op tic tract La teral gen icu late nu cl of thala mus ge niculocalcarin e tra ct (op tic radi atio n) Vi sual Cortex (Are a 17 ) A. Retina (Netter pl. 86; Nolte figs. 17-2, 17-4 to 17-13; Dr. Downing’s materials on “Histology of the Eye”) 1. Retinal cell types a. Receptors: rods and cones b. Bipolar cells c. Ganglion cells Optic nerve is formed by the axons of these ganglion cells. 2. Retinal quadrants: a. The retina is divided into quadrants by horizontal and vertical lines or meridians, which pass through the fovea: Right eye Left eye UTQ UNQ UNQ UTQ nose LTQ LNQ LNQ Macula with fovea centralis in the center LTQ Optic papilla or nerve head (blind spot) RETINA (As you would see it through the patient’s pupil.) Temporal Hemiretina Nasal Hemiretina UTQ = upper temporal quadrant LTQ = lower temporal quadrant UNQ = upper nasal quadrant LNQ = lower nasal quadrant 2 Med 6573: Nervous System B. Visual System Pathways Visual Fields (Nolte fig. 17-31) 1. Visual field = the entire area which can be "seen" by the patient without movement of the head and with the eyes fixed on a single spot. Temporal Field of Left Eye Nasal Field of Left Eye 2. For convenience, the same lines or meridians that define retinal quadrants also define quadrants of the visual field. Upper Field F 3. Mapping of Visual Fields: Visual fields are recorded on charts so that the field is represented as the subject sees it. Thus, for the left eye, the upper field is plotted above, the lower field is plotted below, the temporal field is plotted to the left, and the nasal field is plotted to the right. Each eye is tested separately so “A” is the plot for the left eye and “B” is the plot for the right eye. Each of these plots is a Monocular Visual Field. Numbers along the meridians are degrees of visual angle from the center of the fovea (F). Lower Field Normal Monocular Visual Field of Left Eye 4. Monocular Visual Field = total extent of the external world perceived by one eye without movement of the head or change of ocular fixation. Visual field is not round. Blind spot is 15° to the temporal side of the visual field and on the horizontal meridian, corresponding to the optic disk that is located on nasal side of retina. F Normal Monocular Visual Field of Right Eye Right visual field Left visual field 5. Binocular Visual Field includes the monocular field of each eye. The central area is the portion of the visual field seen by both eyes (binocular region); the areas at the sides are the temporal monocular crescents of the visual field seen only by the nasal portions of each retina. F If eyes are aligned correctly by the extraocular muscles, the image falls on "corresponding points" of the two retinas and the subject perceives a Normal Binocular Visual Field single image. Diplopia occurs when the images are not aligned to fall on corresponding points of the retina. Be sure to distinguish between the "Monocular visual field of the right eye" vs. the "Binocular right visual field" and vice versa for the left counterparts. 3 Med 6573: Nervous System Visual System Pathways 6. The image on the retina of an object located in the visual field is both inverted and reversed from right to left: Nasal Retina of Left Eye Left Visual Field Right Retinal Halves Temporal Retina of Right Temporal Retina of Left Eye Right Visual Field Left Retinal Halves Nasal Retina of Right Eye Upper Visual Fields Lower Retinal Halves of Both Eyes Lower Visual Fields Upper Retinal Halves of Both Eyes NOTE: To avoid confusion and abide by convention, central representation, deficits, etc., will be described in terms of visual fields and not retinal quadrants. (The literature is not consistent in its terms of reference--so be sure that you know whether a given source is referring to visual fields or retinal quadrants.) 4 Med 6573: Nervous System Visual System Pathways C. Optic Nerve (SSA) 1. Extends from the retina to the optic chiasm. 2. Composed of the axons of ganglion cells in the ipsilateral retina. D. Optic Chiasm 1. Located in the anterior part of the sella turcica, immediately in front of the pituitary gland. 2. Partial crossing of the axons from each optic nerve occurs within the chiasm. a. Axons from temporal fields cross. b. Axons from nasal fields do not cross. 3. Partial crossing is essential for binocular vision. E. Optic Tract 1. Continuation of the optic nerve axons from the optic chiasm to the lateral geniculate nucleus of thalamus. 2. Each tract contains axons that receive input from the contralateral visual field. a. L. optic tract receives from R. visual field. b. R. optic tract receives from L. visual field. Reminders about the optic nerve: Develops as an outgrowth of the diencephalon. Essentially a CNS tract; therefore, not a “true” cranial nerve. No associated cranial nerve nuclei in the brain stem. “Wilbrand’s Knee”: Immediately after crossing in the optic chiasm, fibers from upper temporal fields loop forward for a short distance into the optic nerve before they continue into the optic tract. See Lesion #3 for clinical implications. Recent evidence indicates this may be an artifact. While most optic tract fibers terminate in LGN, many also terminate in the superior colliculus/pretectum (see Visual Reflexes). Suprachiasmatic nucl. of the hypothalamus (involved with synchronizing visual input with circadian rhythm) also receives visual input at the optic chiasm level. From optic tract to visual cortex (post-chiasmatic portion of the pathway), each side of the brain deals with the contralateral visual field. F. Lateral Geniculate Nucleus (LGN) 1. Primary termination of optic tract axons. 2. Each LGN receives input from the contralateral visual field. 3. Precise retinotopic organization within the LGN. G. Geniculocalcarine Tract (= Optic Radiation) 1. Axons of LGN neurons travel to Area 17 via the retrolenticular & sublenticular portions of the internal capsule. 2. Axons representing upper and lower fields are separated by macular fibers and take different routes to the cortex: a. Fibers from upper visual fields travel forward into the temporal lobe as Meyer's loop before turning toward the occipital cortex. b. Fibers from lower visual fields travel more directly through the parietal lobe toward the occipital cortex. (Dashed lines from LGN to cortex in diagram on page 4) c. Macular fibers lie intermediate in the radiation. (Not really shown on the diagram.) H. Visual Cortex 1. Primary visual cortex (Area 17 or striate cortex) is located on either side of and within the calcarine fissure. a. Upper visual fields project to the lingual gyrus. b. Lower visual fields project to the cuneate gyrus. c. Macular representation is most caudal in Area 17. d. Peripheral field representation occupies the rostral two-thirds of Area 17 (monocular segment is most rostral). 2. Association visual cortex (Areas 18 and 19) a. Input from Area 17 and elsewhere. b. Deals with complex aspects of vision - such as recognition of subjects and their significance. c. Lesions of association visual cortex result in visual agnosia. d. Projections to superior colliculus (via optic radiation and brachium of superior colliculus): automatic scanning movements (such as those involved in reading) accommodation/convergence reflex 5 Med 6573: Nervous System Visual System Pathways II. Defects in the Visual Pathway Left Right 1. Normal visual fields Not retinal quadrants 2. Blindness of the right eye 3. Blindness of right eye + contralateral left upper quadrantanopia 4. Bitemporal heteronymous hemianopsia 5. Left homonymous hemianopsia 6. Left upper homonymous quadrantanopsia 7. Left homonymous hemianopsia with sparing of macular vision Definitions 1. Strabismus (squint): Failure of coordination of extraocular eye muscles, resulting in deviation of the affected eye and diplopia. 2. Diplopia: Double vision due to failure of the image to be aligned on corresponding points of the retinae of the left and right eyes. 3. Amblyopia (lazy eye): Decreased visual acuity in the absence of anatomical defects in the visual pathway. Secondary to strabismus; to avoid diplopia, the vision in one eye is suppressed at the level of the visual cortex. Occurs in children with the critical period variously reported as ending by age 3/4 years and up to 8 years. 4. Scotoma: Area or 'island' of visual loss within the visual field. 5. Quadrantanopsia: Defective vision or blindness in approx. one-fourth of the visual field. 6. Hemianopsia: Defective vision or blindness in approx. one-half of the visual field. 7. Homonymous defects: Visual defects restricted to either the right or the left visual field (postchiasmatic defects). 8. Heteronymous defects: Visual defects involving parts of both the left and the right visual fields so that visual field defects are non-overlapping. (Almost always occur at the chiasm). 9. Congruous defects: Visual defects are equivalent in each monocular visual field. (#5 above) 10. Incongruous defects: Visual defects are not equivalent in each monocular visual field. (#3 above) 11. Altitudinal defects: Visual defects are in the upper or lower aspect of the visual fields. (#6 above) 6 Med 6573: Nervous System Visual System Pathways III. Visual Reflexes A. Pupillary Light Reflex (i.e. constriction in response to light; = Miosis) (Nolte fig. 17-38) Pretectal Nuclei Optic nerve + Tract + + Superior Colliculus Brachium of the Superior Colliculus Ipsilateral Nucleus of Edinger Westphal (pre-gang) Ipsilateral Ciliary Ganglion DIRECT REFLEX Constriction of Pupil (post-gang) Posterior Commissure (pre-gang) Pretectal Nuclei + Superior Colliculus AFFERENT LIMB (II) Contralateral Nucleus of Edinger Westphal (post-gang) Constriction of Pupil CONSENSUAL REFLEX Contralateral Ciliary Ganglion EFFERENT LIMB (III) CENTRAL CONNEX 1. Afferents bypass the lateral geniculate nucleus and enter the brachium of the superior colliculus (AKA superior brachium). 2. The reflex is abolished if either the afferent (II) or efferent (III) components are damaged. (Lesion of II Marcus Gunn pupil) 3. Blindness due to a lesion in the optic radiation or visual cortex would not result in loss of the pupillary light reflex since this is a subcortical pathway. 4. In a patient with total blindness in one eye due to an optic nerve lesion, a consensual light reflex can be elicited in the 'blind' eye upon stimulation of the 'good' eye. B. Pupillary Dilation (= Mydriasis) Decreased light to pupil Severe pain Strong emotional stimulus ? Cortex, Thalamus & Hippocampus ? Hypothalamus (CNS control center for AN S) Reticular Formation Reticulospinal fibers Dilation of pupil Superior Cervical Ganglion (post-ganglionic sympathetic) 7 (pre-ganglionic sympathetic) Preganglionic Sympathetic Neurons in Thoracic Cord (T1-T2) Med 6573: Nervous System Visual System Pathways Horner's Syndrome: 1. Pupillary constriction due to paralysis of the dilator pupillae muscle. 2. Ptosis due to paralysis of smooth muscle in the eyelid. 3. Flushed and dry skin due to vasodilation and absence of sweating. Deficits result from interruption of the sympathetic innervation to the head. The lesion producing the syndrome could be located in either the CNS or the PNS areas related to this sympathetic innervation. Symptoms are ipsilateral to the lesion. C. Accommodation Reflex (AKA “Near Reflex” or “Accommodation-Convergence Reaction”) (Nolte fig. 17-38) 1. Initiated when gaze is shifted from a distant object to a near one and the image on the retina becomes blurred. 2. Reaction involves: a. Ocular convergence - both medial recti contract to align image. (GSE) b. Pupillary constriction - constrictor pupillae muscles contract to sharpen the image. (GVE) c. Lens thickening - ciliary muscle contracts, increasing refractive power of the lens for focusing on a near object. (GVE) 3. Efferent limb of the reflex is carried by the GSE and GVE components of the oculomotor nerve. 4. Afferent limb and central connections of the reflex are unclear but probably some version of the following: optic tract lateral geniculate nucleus of thalamus optic radiation primary visual cortex association visual cortex optic radiation brachium of superior colliculus superior colliculus the oculomotor nuclei oculomotor nerve (GVE and GSE components) 5. Be aware of the term "Argyll Robertson pupil” where the pupil accommodates to near objects but does not react to light. a. Seen in patients with tabes dorsalis/tertiary syphilis, systemic lupus erythematosus and diabetes mellitus. b. Indicates that the pathways for pupillary constriction associated with these two reflexes are somewhat different. There is some evidence that the lesion associated with an Argyll Robertson pupil may be located in the pretectal area. 8