protocols for use by the rapid response team registered nurse
advertisement
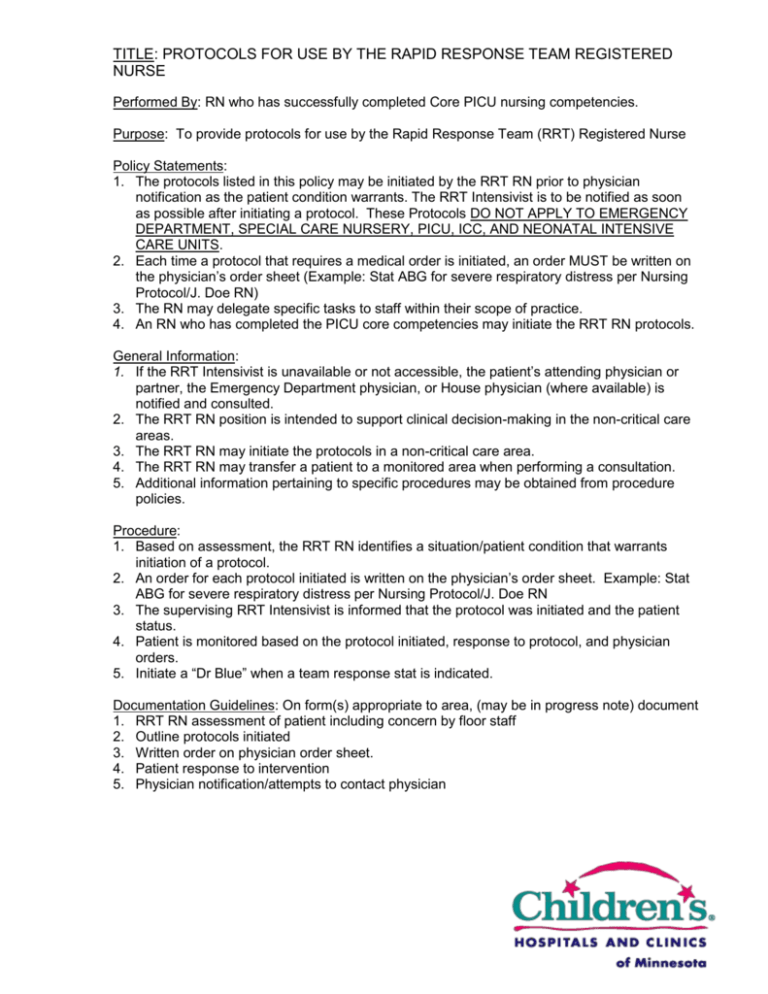
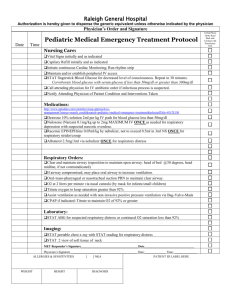
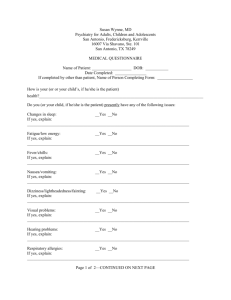
TITLE: PROTOCOLS FOR USE BY THE RAPID RESPONSE TEAM REGISTERED NURSE Performed By: RN who has successfully completed Core PICU nursing competencies. Purpose: To provide protocols for use by the Rapid Response Team (RRT) Registered Nurse Policy Statements: 1. The protocols listed in this policy may be initiated by the RRT RN prior to physician notification as the patient condition warrants. The RRT Intensivist is to be notified as soon as possible after initiating a protocol. These Protocols DO NOT APPLY TO EMERGENCY DEPARTMENT, SPECIAL CARE NURSERY, PICU, ICC, AND NEONATAL INTENSIVE CARE UNITS. 2. Each time a protocol that requires a medical order is initiated, an order MUST be written on the physician’s order sheet (Example: Stat ABG for severe respiratory distress per Nursing Protocol/J. Doe RN) 3. The RN may delegate specific tasks to staff within their scope of practice. 4. An RN who has completed the PICU core competencies may initiate the RRT RN protocols. General Information: 1. If the RRT Intensivist is unavailable or not accessible, the patient’s attending physician or partner, the Emergency Department physician, or House physician (where available) is notified and consulted. 2. The RRT RN position is intended to support clinical decision-making in the non-critical care areas. 3. The RRT RN may initiate the protocols in a non-critical care area. 4. The RRT RN may transfer a patient to a monitored area when performing a consultation. 5. Additional information pertaining to specific procedures may be obtained from procedure policies. Procedure: 1. Based on assessment, the RRT RN identifies a situation/patient condition that warrants initiation of a protocol. 2. An order for each protocol initiated is written on the physician’s order sheet. Example: Stat ABG for severe respiratory distress per Nursing Protocol/J. Doe RN 3. The supervising RRT Intensivist is informed that the protocol was initiated and the patient status. 4. Patient is monitored based on the protocol initiated, response to protocol, and physician orders. 5. Initiate a “Dr Blue” when a team response stat is indicated. Documentation Guidelines: On form(s) appropriate to area, (may be in progress note) document 1. RRT RN assessment of patient including concern by floor staff 2. Outline protocols initiated 3. Written order on physician order sheet. 4. Patient response to intervention 5. Physician notification/attempts to contact physician Rapid Response Team Protocols RESPIRATORY Nursing Protocols 1. O2 to keep saturations > 90%. CARDIOVASCULAR Nursing Protocols 1. Peripheral IV and/or keep open an existing IV with normal saline. 2. Monitoring as indicated 2. STAT chest x-ray with reading. Oximetry Cardio respiratory Apnea 3. Suction as needed. 4. For a patient in respiratory distress Call Respiratory Therapy for Respiratory Care Assessment and give any previously ordered treatment STAT x1. Respiratory treatment X1 of Albuterol 2.5 mg (0.5 mls) in 2.5 mls of NS nebulized using 8 – 10 L of O2 flow ABG or VBG testing one time. STAT chest x-ray with reading. 5. May return to last stable ventilator setting if patient fails ventilator weaning as evidenced by: Respiratory rate O2 saturation 90% Level of consciousness Anxiety Contact Respiratory Care for Respiratory Care Assessment and to Return patient to last stable ventilator Setting. 6. Transfer to higher level of care if indicated. 3. For Chest pain: Obtain STAT 12 lead EKG and report results to supervising physician. Cardiac monitoring (e.g.: Lead II) O2 to keep saturation 90%. B/P-Pulse-Resp. every 5 minutes and document. 4. For symptomatic hypotension (40mm Hg drop in systolic baseline), call supervising Intensivist STAT and: Utilize MODIFIED Trendelenburg position by elevating legs and leaving head flat. DO NOT use Trendelenberg position as it may increase respiratory distress and cause refractory bradycardia or hypotension. Bolus with 10 mls/kg NS IV. Monitor B/P-Pulse-Resp. every 5 minutes and document until patient is no longer symptomatic, returns to baseline, or is transferred to a monitored bed. Use non-invasive automatic cuff or doppler stethoscope to monitor B/P. Remove topicals that may cause hypotension such as Nitroglycerin patch/paste, Duragesic, or Catapres patch. Hold oral antihypertensive until physician is consulted. 5. For suspected/active bleeding order and draw: STAT CBC and send to lab Type and screen and hold pending CBC results. If Hgb 8, send type and screen to lab and set up 2 units packed cells 6. Transfer to higher level of care if indicated.