Objectives 36 - U
advertisement
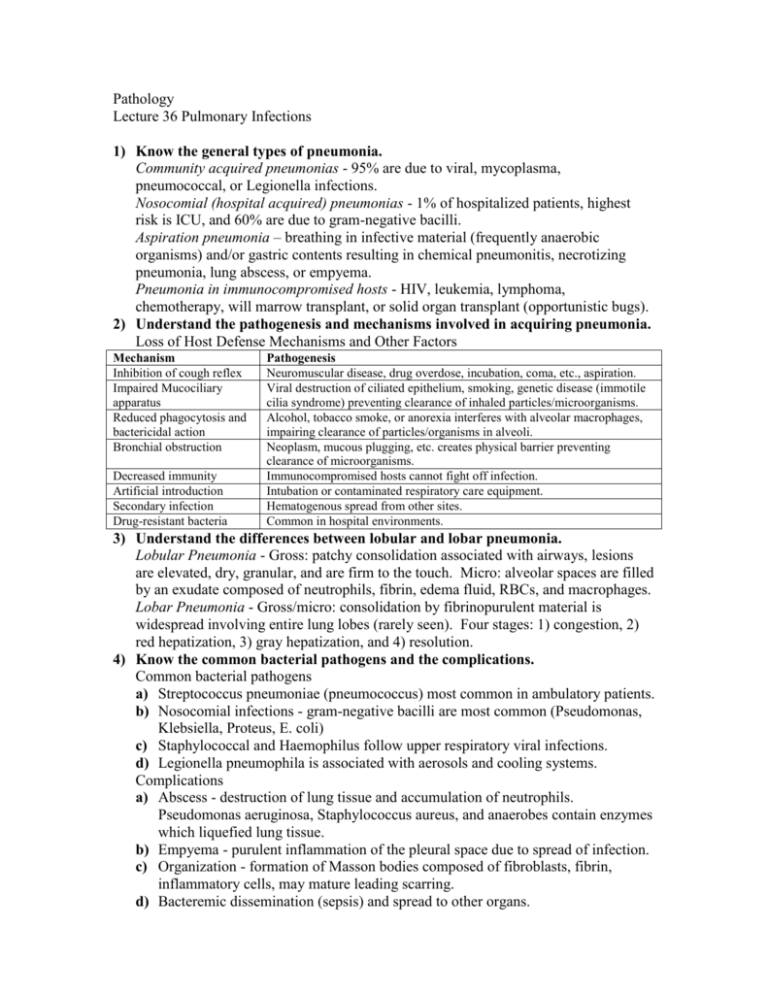
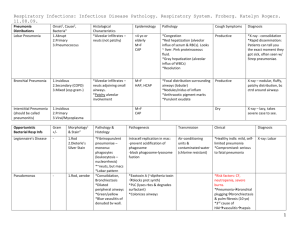
Pathology Lecture 36 Pulmonary Infections 1) Know the general types of pneumonia. Community acquired pneumonias - 95% are due to viral, mycoplasma, pneumococcal, or Legionella infections. Nosocomial (hospital acquired) pneumonias - 1% of hospitalized patients, highest risk is ICU, and 60% are due to gram-negative bacilli. Aspiration pneumonia – breathing in infective material (frequently anaerobic organisms) and/or gastric contents resulting in chemical pneumonitis, necrotizing pneumonia, lung abscess, or empyema. Pneumonia in immunocompromised hosts - HIV, leukemia, lymphoma, chemotherapy, will marrow transplant, or solid organ transplant (opportunistic bugs). 2) Understand the pathogenesis and mechanisms involved in acquiring pneumonia. Loss of Host Defense Mechanisms and Other Factors Mechanism Inhibition of cough reflex Impaired Mucociliary apparatus Reduced phagocytosis and bactericidal action Bronchial obstruction Decreased immunity Artificial introduction Secondary infection Drug-resistant bacteria Pathogenesis Neuromuscular disease, drug overdose, incubation, coma, etc., aspiration. Viral destruction of ciliated epithelium, smoking, genetic disease (immotile cilia syndrome) preventing clearance of inhaled particles/microorganisms. Alcohol, tobacco smoke, or anorexia interferes with alveolar macrophages, impairing clearance of particles/organisms in alveoli. Neoplasm, mucous plugging, etc. creates physical barrier preventing clearance of microorganisms. Immunocompromised hosts cannot fight off infection. Intubation or contaminated respiratory care equipment. Hematogenous spread from other sites. Common in hospital environments. 3) Understand the differences between lobular and lobar pneumonia. Lobular Pneumonia - Gross: patchy consolidation associated with airways, lesions are elevated, dry, granular, and are firm to the touch. Micro: alveolar spaces are filled by an exudate composed of neutrophils, fibrin, edema fluid, RBCs, and macrophages. Lobar Pneumonia - Gross/micro: consolidation by fibrinopurulent material is widespread involving entire lung lobes (rarely seen). Four stages: 1) congestion, 2) red hepatization, 3) gray hepatization, and 4) resolution. 4) Know the common bacterial pathogens and the complications. Common bacterial pathogens a) Streptococcus pneumoniae (pneumococcus) most common in ambulatory patients. b) Nosocomial infections - gram-negative bacilli are most common (Pseudomonas, Klebsiella, Proteus, E. coli) c) Staphylococcal and Haemophilus follow upper respiratory viral infections. d) Legionella pneumophila is associated with aerosols and cooling systems. Complications a) Abscess - destruction of lung tissue and accumulation of neutrophils. Pseudomonas aeruginosa, Staphylococcus aureus, and anaerobes contain enzymes which liquefied lung tissue. b) Empyema - purulent inflammation of the pleural space due to spread of infection. c) Organization - formation of Masson bodies composed of fibroblasts, fibrin, inflammatory cells, may mature leading scarring. d) Bacteremic dissemination (sepsis) and spread to other organs. 5) Know the common viral pathogens and presentation. How does viral pneumonia differ from bacterial pneumonia? Common viral pathogens: influenza, adenovirus, measles, and varicella (most common pneumonia in children, <10% in adults). Note: Mycoplasma and Chlamydia are common in adults and clinically similar to viral pneumonia. Presentation: fever, headaches, muscle aches, and dry, hacking nonproductive cough. Mortality is <1% in most common competition is secondary bacterial pneumonia. Differences from bacterial pneumonia: Gross: may be patchy or lobar, bilateral or unilateral, congested, reddish blue color, and sometimes hemorrhagic. Micro: mononuclear infiltrate, proteinaceous fluid in alveolar spaces, hyperplastic Type II pneumocytes, hyaline membrane lined alveolar walls, sometimes necrosis of bronchial alveolar epithelium (herpes, varicella, and adenovirus), and viral inclusions (CMV, herpes, and measles). 6) Know the common fungal pathogens and their relevance and prognosis for the patient. Fungal pathogen Coccidiodomycosis Histoplasmosis Tuberculosis Relevance >80% persons in endemic areas have a positive skin test. Primarily granulomatous inflammation, possibly purulent reaction. Identified using silver stain as small (2-5 µ) dark oval shaped forms producing epithelioid cell granulomas and coagulative necrosis Increased incidence due to AIDS epidemic and emergence of drug-resistant strains. Caseating granulomas with primary or secondary complex, miliary spread, and bronchopneumonia Prognosis Most primary infections are asymptomatic, 10% have lung lesions, pleuritic pain, and cough Primary infection is usually innocuous unless patient is immunocompromised Primary infection asymptomatic or flu-like illness. Secondary infection more severe, erosion producing hemoptysis. 7) Understand the disease states associated with opportunistic infections and their implications for the patient. Disease Pneumocystis carinii Aspergillus species Zygomycetes (Mucor and Rhizopus) Cryptococcus Candida and Torulopsis species CMV/Herpes Simplex Actinomyces and Nocardia Implications Produces an alveolar infiltrate of foamy material and mononuclear cells. Diagnosis is based on identifying the grouped, 4-5 µ, cup-shaped organisms. Ubiquitous organism found in soil and commonly inhaled into the lungs. May grow in old scars or invade parenchyma producing a necrotizing pneumonia. Commonly invades veins and arteries producing hemorrhagic infarcts. Like Aspergillus, it frequently invades arteries and veins. Hyphae are non-septate and branch at 90° Inhaled encapsulated yeast causing mild pulmonary symptoms and often spreading to the CNS in immunocompromised patients. Yeasts that are part of the normal flora but can produce bronchitis, bronchopneumonia, hemorrhagic pneumonia, and acute abscess. Can produce hemorrhagic interstitial pneumonias. Filamentous, branching bacterium which can produce acute pneumonias with rapid progression to abscesses.