Resuscitation
advertisement

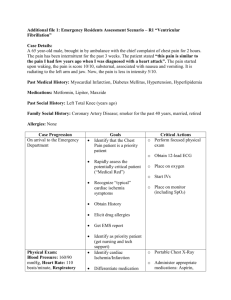
Resuscitation The following are only general guidelines taken from the APLS manual and need to be varied according to the condition of the child Cardiac arrest in children is rarely due to primary cardiac disease, they are mostly secondary to hypoxia (birth asphyxia, inhalation of foreign body, bronchiolitis, asthma and pneumothorax) or secondary to neurological dysfunction (poisoning, convulsions) The management of a critically ill child requires a systematic, well rehearsed team approach. Nowhere is a well-functioning team more vital than in the emergency situation. Success depends on each team member carrying out his or her own tasks and being aware of the skills of the other team members.The whole must be under the direction of a team leader. One person should be responsible for documentation of all the drugs etc given. Preparation If warning has been received of the child’s arrival, then preparations can be made: Ensure the appropriate help is available Work out the likely drug, fluid and equipment needs Initial assessment Airway Is the child breathing? If no – an attempt to open the airway should be made using the head tilt/chin lift manoeuvre (see APLS/EPLS manual) Breathing Is the child breathing? (look, listen and feel) If no – give 5 initial rescue breaths Circulation Is there no pulse or pulse < 60 beats per minute or no signs of circulation? If yes – commence cardiac compressions Chest compressions should compress the lower third of the sternum The finger/thumb or hand position for all ages is found by locating the xiphisternum and placing the finger/thumb or hand one finger breadth above this. 2 Infants: Infant chest compression can be more effectively achieved using the hand encircling technique; the infant is held with both the rescuers hands encircling the chest. The thumbs are placed in the correct position, as above, and compression carried out. (See APLS manual for diagrams). This only works for 2 rescuers. If alone, the single rescuer should use the 2 finger approach. Children: Place the heel of one hand over the lower third of the sternum one finger breadth above the xiphisternum. Lift the finger to ensure pressure is not applied over the child’s ribs. Position yourself vertically above the child’s chest and, with your arm straight, compress the sternum to depress it by approximately 1/3 rd of the depth of the chest. For larger children this may be achieved by using both hands with the fingers interlocked. Again, see APLS manual for diagrams. Once the correct technique has been chosen and the area for compression identified, 15 compressions should be given to 2 ventilations Compression rate is 100/minute for all ages Intravenous/intraosseus access Consider intubation Weight = 2(age years + 4) The following pages contain the APLS algorithm 3 Stimulate and assess response Open airway Check breathing 5 rescue breaths Check pulse or signs of circulation CPR 15 ventilations:2 compressions Shockable? VF/VT algorithm Assess rhythm 4 Non-shockable? PEA,asystole Non-Shockable - Asystole and PEA: Ventilate with high concentration O2 Continue CPR Continue CPR Intubate IV/IO access Adrenaline 10mcg/kg ( 0.1mls 1:10,000 solution) IV or IO Pause briefly to check monitor every 2 minutes 4 minutes CPR Consider and correct reversible causes of cardiac arrest based on any history of the event and any clues that are found during the resuscitation – 4Hs and 4Ts Hypoxia Tension pneumothorax Hypovolaemia Tamponade Hyperkalaemia Toxic substances Hypothermia Thromboembolic 5 Shockable - VF and pulseless VT. DC shock 4j/kg 2 minutes CPR check monitor Intubate, high flow O2 IV/IO access DC shock 4j/kg 2 minutes CPR check monitor Intubate IV/IO access Adrenaline10mcg/kg then DC shock 4j/kg 2 minutes CPR check monitor Amiodarone 5mg/kg then DC shock 4J/kg 2 minutes CPR check monitor Consider 4Hs 4Ts Consider alkalising agents Adrenaline then DC shock 4J/kg 2 minutes CPR check monitor 2 minutes CPR check monitor DC shock 4J/kg ALS Updated March 2009 review 2011 Ref : APLS manual 4th Edition 6