Metabolic Diseases
advertisement
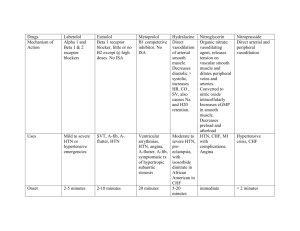
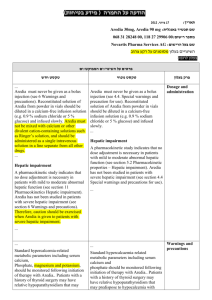
Metabolic Diseases Background Some metabolic diseases present throughout the life span from infancy to adulthood with signs or symptoms of hepatic dysfunction including: Hepatomegaly Jaundice Hypoglycaemia Elevation of hepatic enzymes Hyperammonaemia Failure to thrive Protein or food intolerance Anorexia, vomiting and diarrhoea Adverse affects of hepatic dysfunction on the central nervous system include ataxia, stupor, coma and hypoglycaemic episodes. Examples of in born errors with hepatic dysfunction: Urea cycle defects Organic aciduria Fatty acid oxidation defects Hepatic glycogen storage diseases Tyrosinaemia Transferase deficient galactosaemia Hereditary fructose intolerance Wilson’s disease Various storage disorders Almost all disorders are autosomal recessive with incidence ranging from 1 in 10,000 to 1 in 500,000. Some diseases are detected by screening before any signs of symptoms are present. Hyperammonaemic states and organic acidurias can occasionally present with hepatic more than CNS findings. Differential diagnosis Precious time can be lost if the diagnosis of an in born error is not considered and hepatopathy and CNS symptoms are attributed to perinatal insults. Infections; TORCH Toxins Pancreatitis Congenital hepatic and bowel duct malformations Malrotational volvulus Ketotic hypoglycaemia Reye syndrome History A full history is essential. Important questions would include: Is there a family history of death in early infancy or undiagnosed severe liver disease? Is there any pattern to the illness? o Metabolic deterioration to fasting or childhood infection o Association of symptoms with ingestion of protein, lactose, sucrose o salicylate and viral infections o Inability of patient to fast for longer than 8-12 hours Physical examination Full examination essential Tachypnoea (caused by metabolic acidosis or respiratory alkalosis Hepatomegaly Jaundice CNS findings Failure to thrive Investigations The most useful samples are those taken at the time of admission when acutely ill, and this opportunity should not be missed. If a non-metabolic diagnosis is made subsequently, samples for the special bio-chemical tests can always be discarded. 1. Essential preliminary tests a) FBC & differential Coagulation screen b) Blood gas and acid base status Bio-chemical profile Plasma-glucose Plasma amino acids Urine must be saved for organic and amino acids (the best sample is the first urine past at the time of acute admission). Diagnostic abnormalities often disappear quickly following IV glucose or other resuscitation. A urine bag should be applied at once and if possible at least 5mls of urine collected and save the next urine sample past as well. c) Other tests indicated by the clinical features – see below 2. Hypoglycaemia without obvious cause a) b) c) d) e) f) g) h) Us & Es, blood gas and acid base status Liver function tests Glucose Insulin Growth hormone Cortisol Amino acids – OH Butyrate, free fatty acids, Lactate (if hepatomegaly) if possible, take extra 2mls of blood into a lithium heparin tube, which can be separated and stored for special tests (e.g. carnitine) i) Blood spot on Guthrie card for ACE R carnitines spot plasma ammonium Urine First urine should be tested for ketones and stored for organic and amino acid analysis. 3. Suspected hyperammonaemia Ammonia is noted usually when the urea cycle defect is a possible diagnosis and should be measured in any newborn with unexplained lethargy, neurological disturbances, fits, vomiting or hyperventilation, especially if the baby was well initially in the first 24-72 hours of life. Significant values generally exceed 150micromol/l. This is not an exhausted list of tests, further more specialist testing may be required. Treatment Restore acid base balance Administer intravenous glucose at 5-9mg/kg per minute to prevent catabolism Acute detoxification to protect the CNS/ remove ammonia/may require haemofiltration or haemodialysis to be done in a specialist unit Long –term therapy requires a diet deficient in the offending dietary component, examples of this include: organic acidurias, protein restriction, high carbohydrate, glycine, carnitine Urea cycle disorders, protein restrictions, agents that foster waste, nitrogen removal: Sodium Benzoate and Sodium Phenylbutyrate – hypoglycaemic disorders; avoidance of fasting, uncooked starch released carbohydrate over a prolonged period, continuous night feeds by NG tube Bibliography Five-minute paediatric consult – Second Addition Reviewed 2008, next review 2011