Maternal Health in India, Srinivasulu
advertisement
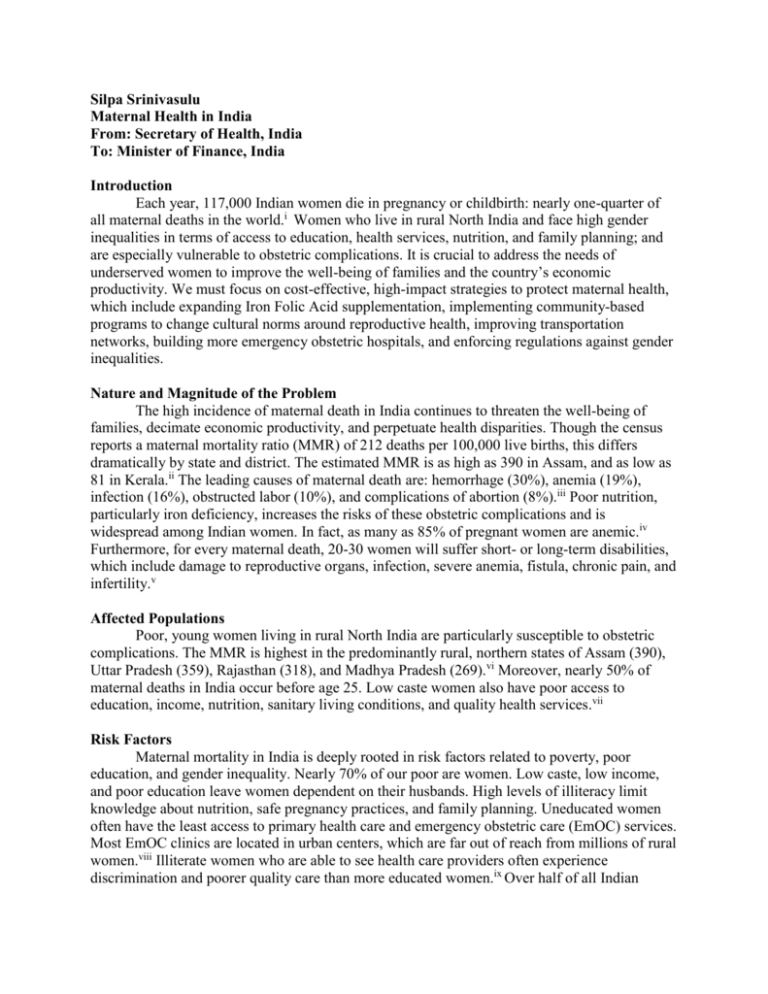
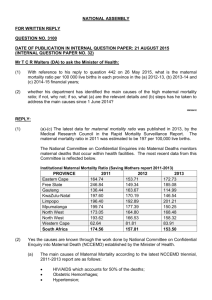
Silpa Srinivasulu Maternal Health in India From: Secretary of Health, India To: Minister of Finance, India Introduction Each year, 117,000 Indian women die in pregnancy or childbirth: nearly one-quarter of all maternal deaths in the world.i Women who live in rural North India and face high gender inequalities in terms of access to education, health services, nutrition, and family planning; and are especially vulnerable to obstetric complications. It is crucial to address the needs of underserved women to improve the well-being of families and the country’s economic productivity. We must focus on cost-effective, high-impact strategies to protect maternal health, which include expanding Iron Folic Acid supplementation, implementing community-based programs to change cultural norms around reproductive health, improving transportation networks, building more emergency obstetric hospitals, and enforcing regulations against gender inequalities. Nature and Magnitude of the Problem The high incidence of maternal death in India continues to threaten the well-being of families, decimate economic productivity, and perpetuate health disparities. Though the census reports a maternal mortality ratio (MMR) of 212 deaths per 100,000 live births, this differs dramatically by state and district. The estimated MMR is as high as 390 in Assam, and as low as 81 in Kerala.ii The leading causes of maternal death are: hemorrhage (30%), anemia (19%), infection (16%), obstructed labor (10%), and complications of abortion (8%).iii Poor nutrition, particularly iron deficiency, increases the risks of these obstetric complications and is widespread among Indian women. In fact, as many as 85% of pregnant women are anemic.iv Furthermore, for every maternal death, 20-30 women will suffer short- or long-term disabilities, which include damage to reproductive organs, infection, severe anemia, fistula, chronic pain, and infertility.v Affected Populations Poor, young women living in rural North India are particularly susceptible to obstetric complications. The MMR is highest in the predominantly rural, northern states of Assam (390), Uttar Pradesh (359), Rajasthan (318), and Madhya Pradesh (269).vi Moreover, nearly 50% of maternal deaths in India occur before age 25. Low caste women also have poor access to education, income, nutrition, sanitary living conditions, and quality health services.vii Risk Factors Maternal mortality in India is deeply rooted in risk factors related to poverty, poor education, and gender inequality. Nearly 70% of our poor are women. Low caste, low income, and poor education leave women dependent on their husbands. High levels of illiteracy limit knowledge about nutrition, safe pregnancy practices, and family planning. Uneducated women often have the least access to primary health care and emergency obstetric care (EmOC) services. Most EmOC clinics are located in urban centers, which are far out of reach from millions of rural women.viii Illiterate women who are able to see health care providers often experience discrimination and poorer quality care than more educated women.ix Over half of all Indian women deliver without the assistance of a skilled birth attendant and only 40% of deliveries take place in an institution.x North Indian women also face striking health shortages compared to South Indian women. Only 23% in the North, compared to 44% in the South, received information on danger signs during pregnancy and childbirth; 60% in the North, compared to 91% in the South, received Iron Folic Acid (IFA) supplements.xi Though illegal, about 40% of rural girls are given away in marriage before age 18.xii States with high rates of child marriage also have the worst rates of maternal mortality. Additionally, most women have low social status and cannot negotiate sexual relationships and family planning with their partners. One in three maternal deaths could be prevented if all women had access to contraceptives.xiii As a result, young women often experience obstetric complications due to early or undesired pregnancies and multiple pregnancies in close intervals. Some traditional practices limit a woman’s access to nutrition. Some women and girls are not permitted to eat until the men have finished eating. In poor households, this custom leaves very little food remaining for females. Thus, they cannot consume enough nutrients, particularly iron, necessary to maintain a pregnancy and deliver healthy babies.xiv Furthermore, the stigma around discussing sex severely limits a woman’s ability to protect her reproductive health. Economic and Social Consequences The consequences of maternal death have drastic economic and social implications for the future of our country. An Indian mother is the center of her household and caretaker of her family. Therefore, her health status is a major determinant of her children’s health. When she dies or is left disabled, her family struggles to survive. UNCIEF reports that “infants whose mothers die within the first six weeks of their lives are more likely to die before reaching age two than infants whose mothers survive.”xv For her surviving, yet undernourished children, studies have shown that “almost all undernutrition indicators were associated with lower educational achievement” and impaired cognitive ability.xvi This contributes to unproductive generations, cycles of poverty, and economic losses for the country. Moreover, obstetric complications, like fistula, not only cause disability, but ostracize women from their families and communities. Priority Action Steps Low cost, high impact strategies to reduce maternal mortality must focus on: improving nutritional status, changing sociocultural norms around reproductive health, tackling delays in EmOC and transportation, and strengthening laws against gender inequalities. In the short run, we must expand IFA supplementation to reach all women, particularly in the North. Community health workers can distribute a weekly dose of IFA to girls between ages 10 and 19 and to pregnant women. It costs only nine rupees to provide 52 tablets per girl per year.xvii This program has succeeded in Vadodara, Gujarat to lower rates of anemia in adolescent girls from 75% to 53% in less than two years. xviii With expansion and commitment, women in other states can also achieve better nutritional status. In the short term, the National Rural Health Initiative must build upon existing villagebased education programs, such as the Inner Spaces Outer Faces Initiative, to teach families and communities about safe pregnancy and child-birth practices and contraception. This interactive approach will promote dialogue and increase the accessibility and demand for family planning services. It will reduce stigma surrounding sex, combat discrimination, encourage the delay of marriage and first birth, and promote community ownership of women’s health.xix We must follow Tamil Nadu’s example in addressing the three delays that harm maternal health. State governments must work with community health centers (CHCs) to improve the quality and accessibility of services. This includes training skilled birth attendants to deliver babies, recognize obstetric emergencies, and handle minor complications.xx Investment in mobile phones, reliable communication networks, safe roads, and ambulances can greatly improve the diagnosis of complications and swift transport to appropriate facilities. In the long-run, we must establish more Comprehensive EmOC hospitals located within an hour of all rural villages to improve timely and quality provision of care.xxi Other long term interventions include changes in policy and regulations. The government should monitor CHCs to prevent discrimination against low caste and uneducated women. Ultimately, the social position of girls will improve only with strict enforcement of laws against gender inequality, particularly against child marriage and for equal access to education. To succeed, political commitment and collaboration among government, law enforcement, and communities is crucial. Bibliography i Center for Reproductive Rights. Maternal Mortality in India: Using International and Constitutional Law to Promote Accountability and Change, 2009. 10. <http://reproductiverights.org/sites/crr.civicactions.net/files/documents/MM_report_FINAL.pdf>. ii India. Ministry of Home Affairs. Office of the Registrar General. Special Bulletin on Maternal Mortality in India 2007-2009. Census and Vital Statistics (2011): 1-4. <http://www.censusindia.gov.in/vital_statistics/SRS_Bulletins/Final-MMR%20Bulletin-200709_070711.pdf>. iii World Health Organization. India: Improving Maternal, Newborn, and Child Health in the South-East Asia Region, 2004. 29. <http://www.searo.who.int/LinkFiles/Improving_maternal_newborn_and_child_health_india.pdf>. iv Center for Reproductive Rights, Maternal Mortality in India, 14. v Center for Reproductive Rights. Salenta v. Uttar Pradesh, 2010. 2. <http://reproductiverights.org/sites/crr.civicactions.net/files/documents/Salenta_v_UP.pdf>. vi India, Special Bulletin on Maternal Mortality in India 2007-2009, 4. vii Center for Reproductive Rights, Maternal Mortality in India, 25. viii UNICEF. “Maternal Mortality: Neglected for too Long.” Progress for Children: A Report Card on Maternal Mortality, 2008. 11. <http://www.unicef.org/childsurvival/files/Progress_for_ChildrenNo._7_Lo-Res_082008.pdf>. ix Center for Reproductive Rights, Maternal Mortality in India, 15-16. x Ibid, 19. xi Ibid, 21. xii Ibid, 16. xiii Ibid, 19. xiv Ibid, 14. xv UNICEF, “Maternal Mortality: Neglected for too Long,” 3. xvi Victoria, Ceasar G., et. al. “Maternal and child undernutrition: consequences for adult health and human capital.” The Lancet 371.9609 (2008). 345. <http://www.thelancet.com/journals/lancet/article/PIIS0140-6736%2807%2961692-4/fulltext>. xvii Walker, Angela. “Iron supplementation helping to end inter-generational cycle of anaemia in India.” UNICEF 2011. <http://www.unicef.org/infobycountry/india_57722.html>. xviii Gulati, Gurinder. “The red tablet is the secret of my energy.” UNICEF 2005. <http://www.unicef.org/india/health_631.htm>. xix Cooperative for Assistance and Relief Everywhere, Inc. and International Center for Research on Women, Challenge and Change: Integrating the Challenge of Gender Norms and Sexuality in a Maternal Health Program. Edited by Anthony Jaffee. New Delhi: 2010. <http://www.care.org/careswork/whatwedo/health/srh/Challenge-and-Change-2010.pdf?s_src=1707607 70000>. xx Skolnik, Richard L. "Women’s Health." Global Health 101. 2nd ed. Burlington, MA: Jones & Bartlett Learning, 2011. Print. p.196. xxi Ibid.